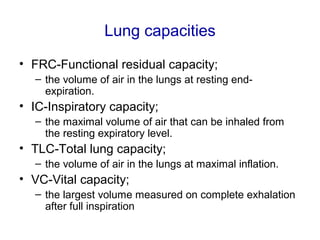
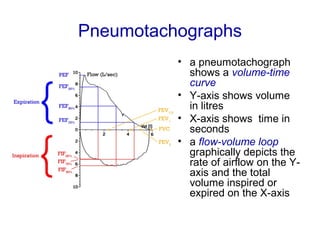
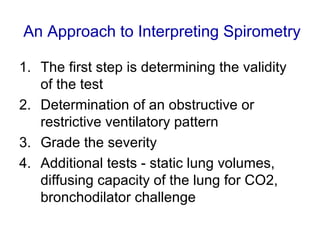
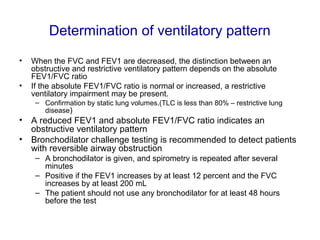
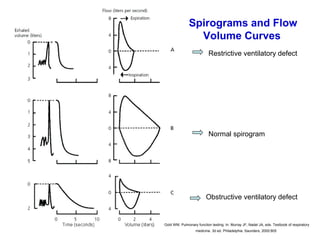
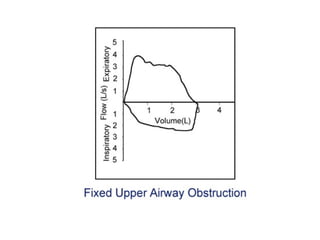
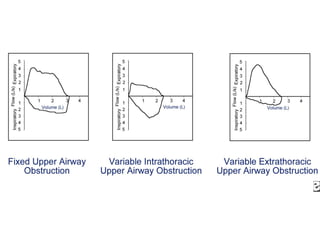
This document provides information on pulmonary function testing and spirometry. It defines key lung volumes and capacities that are measured, such as FVC, FEV1, FRC, RV. Normal values for various pulmonary function tests are provided. Spirometry is described as the most common pulmonary function test used to measure breath volume and flow. The document outlines the technique for spirometry and how to interpret the results to determine if a restrictive or obstructive ventilatory pattern is present. Limitations of spirometry and contraindications to its use are also discussed.