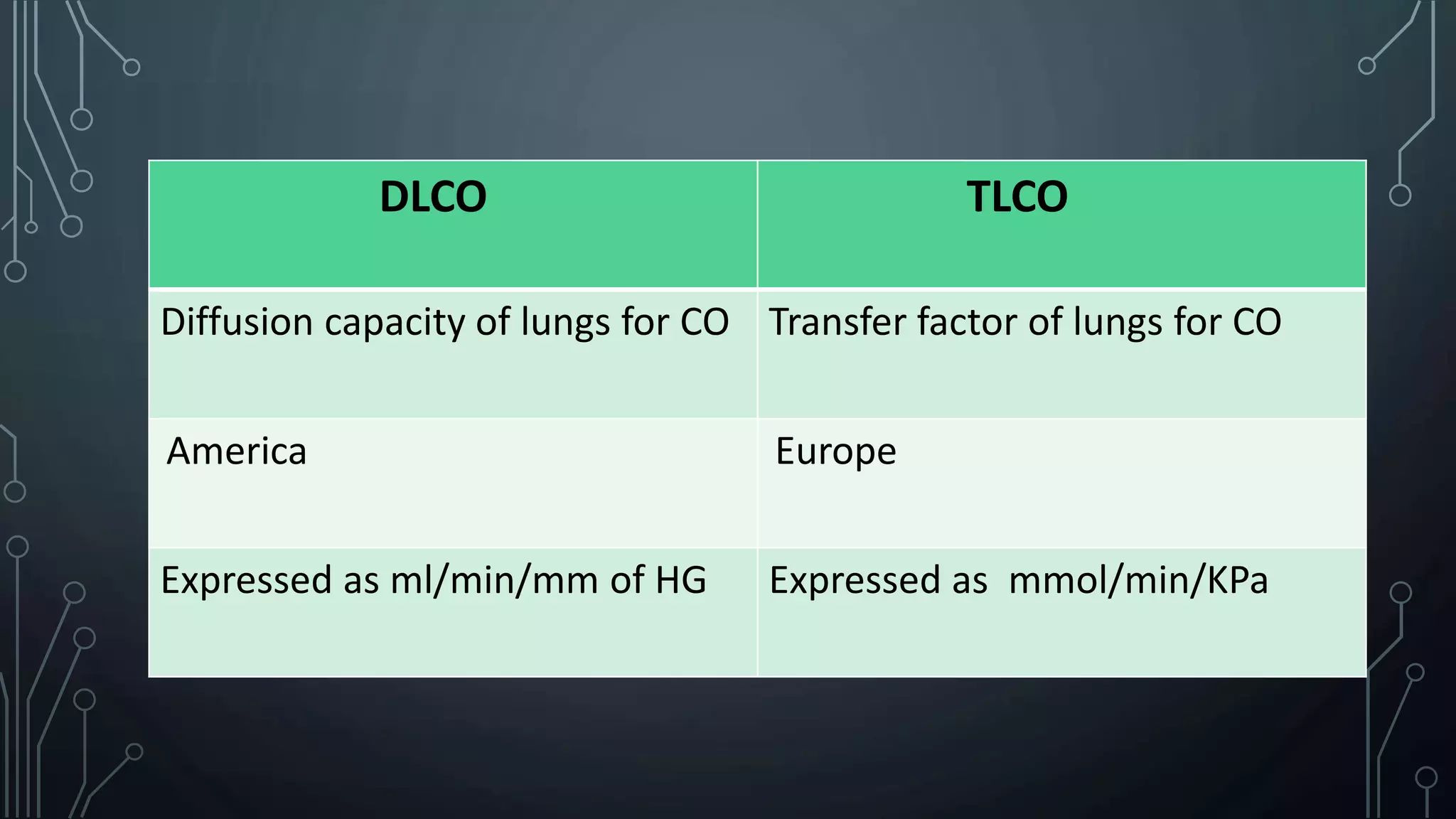
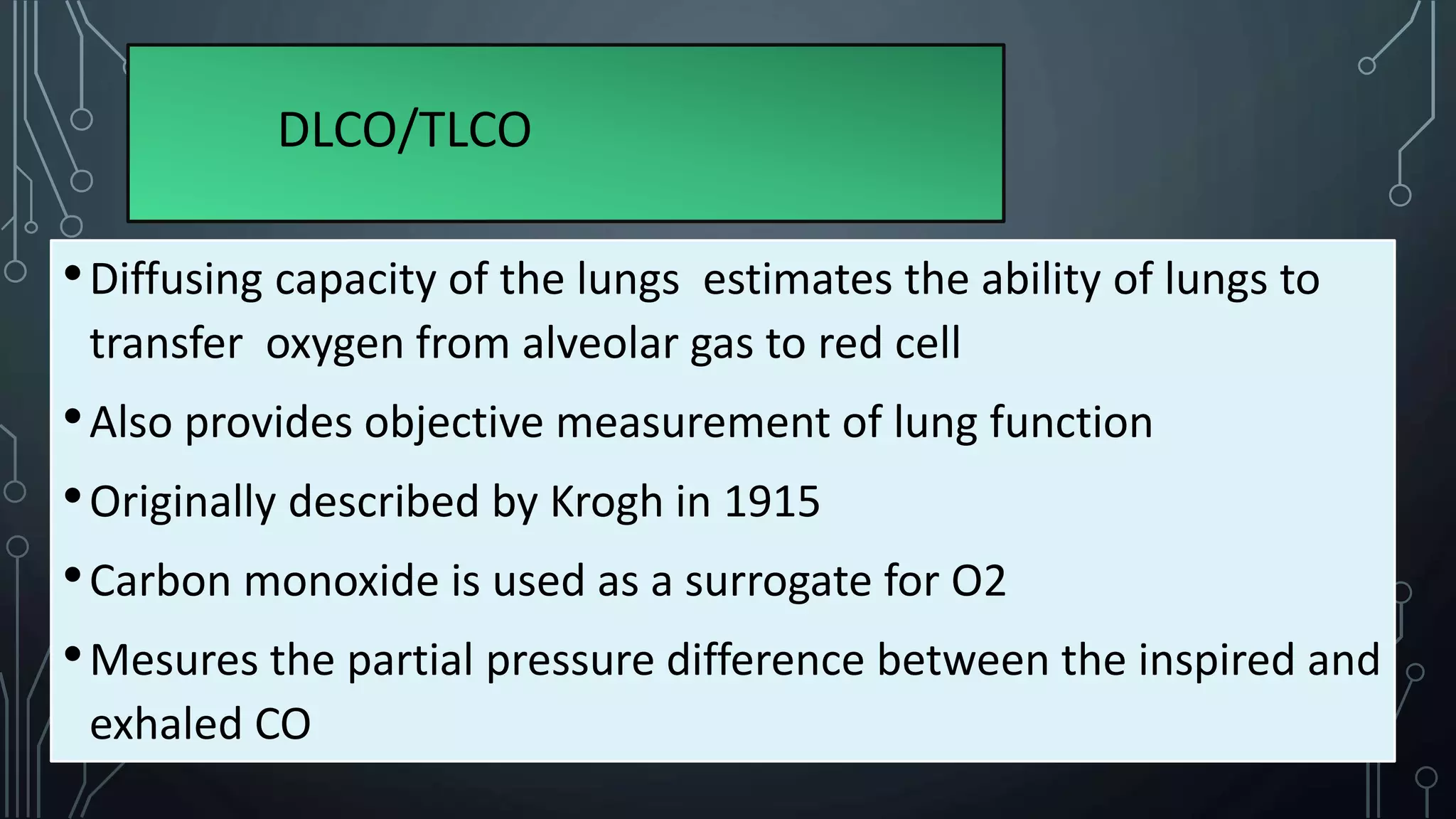
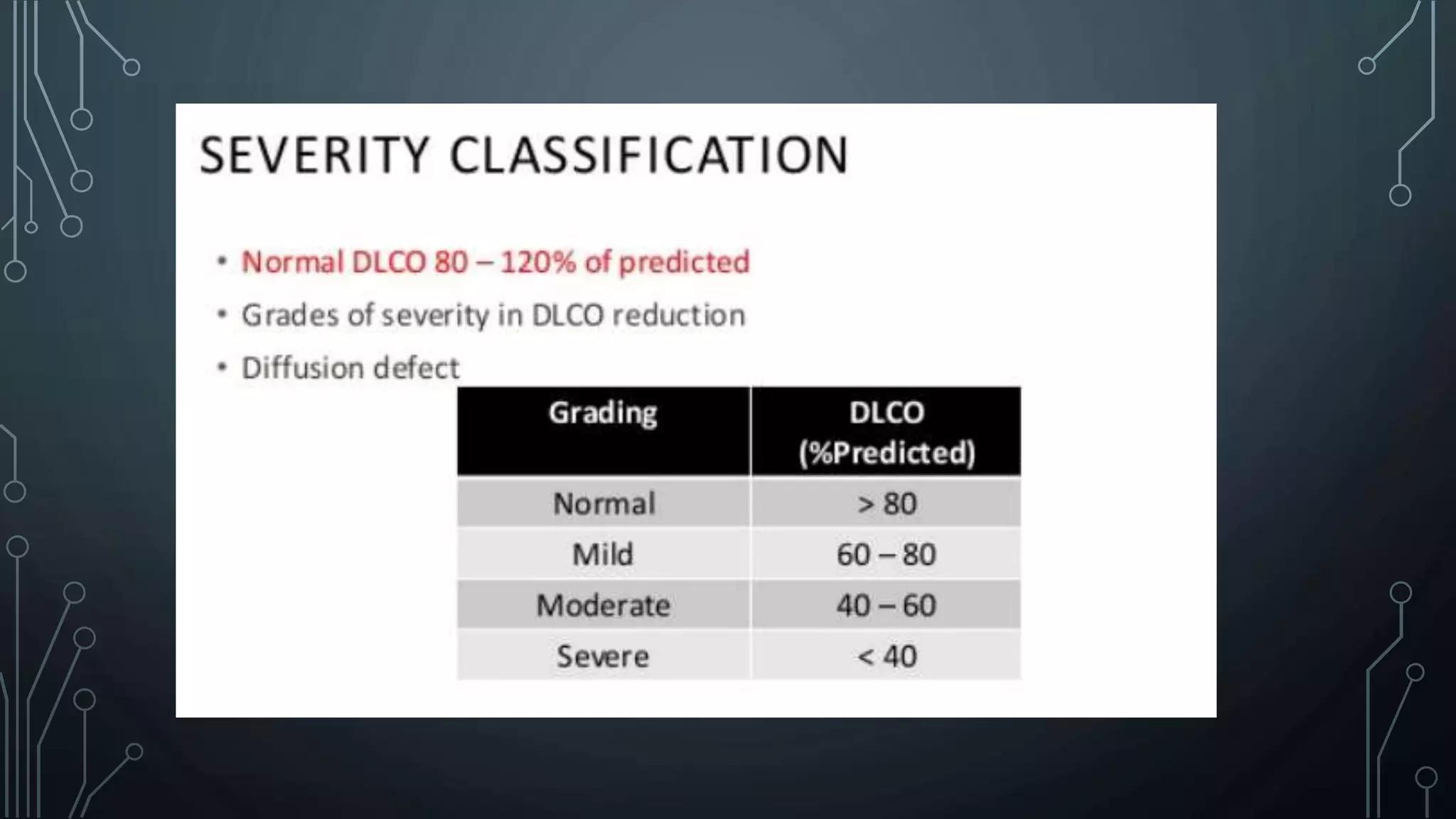
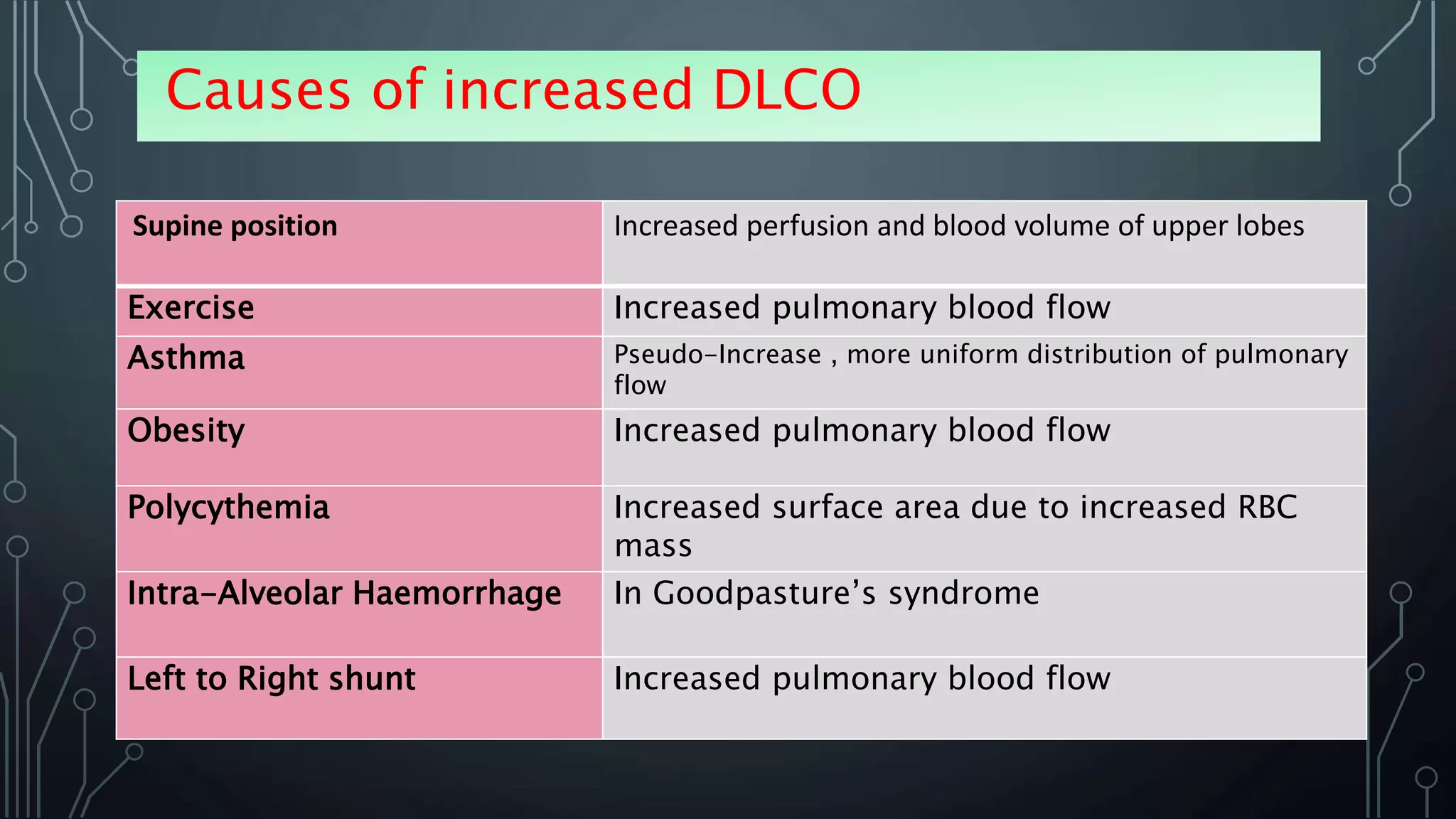
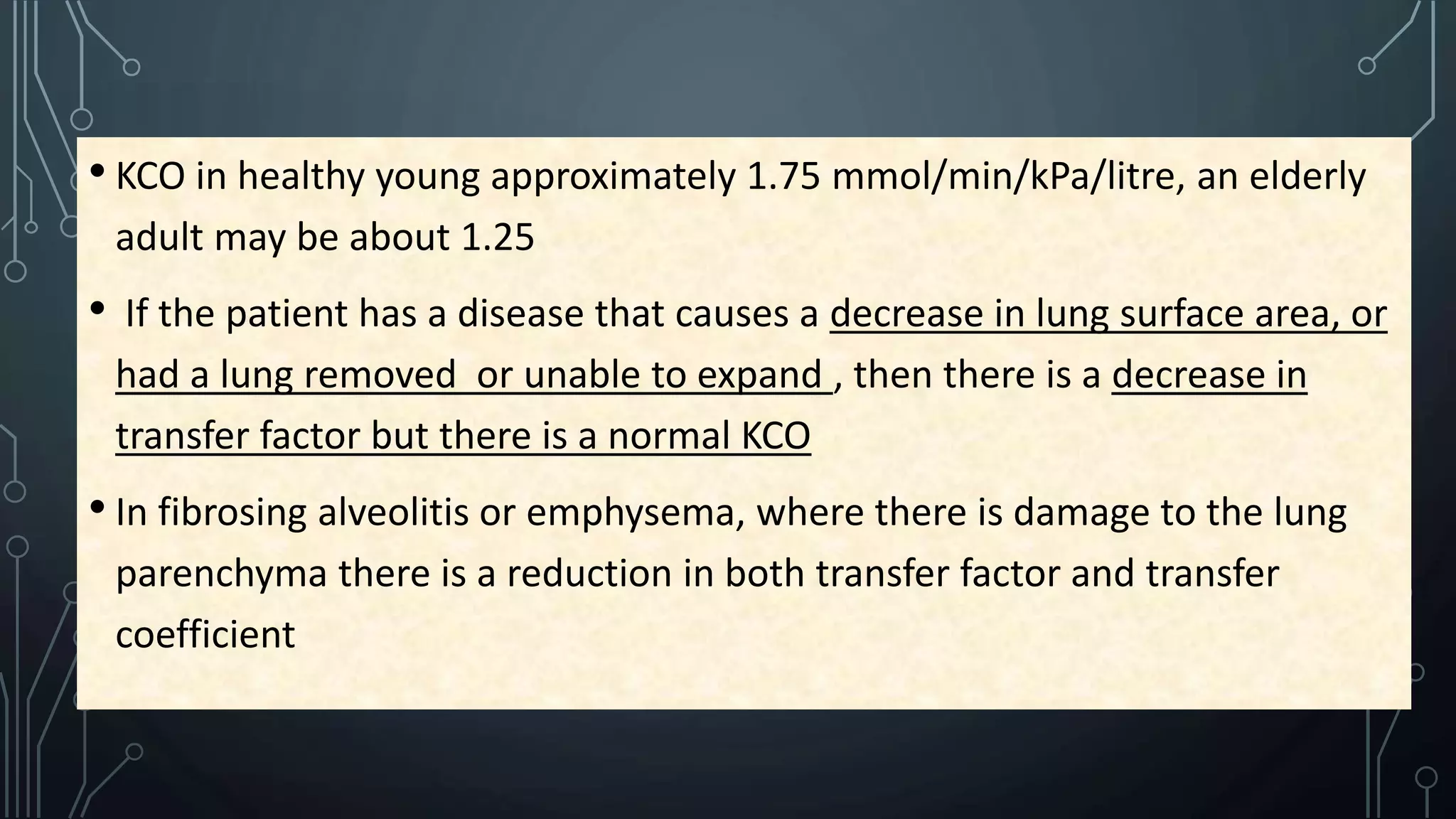
DLCO/TLCO measures the ability of the lungs to transfer carbon monoxide from the alveoli to the blood. It estimates the surface area and thickness of the alveolar-capillary membrane. CO is used instead of oxygen because its transfer is diffusion limited and it binds readily to hemoglobin. A single-breath hold method is most common where the patient inhales a gas mixture and holds their breath for 10 seconds while CO uptake is measured. DLCO can help identify interstitial lung diseases, emphysema, pulmonary hypertension and assess treatment response. Reduced DLCO may be due to decreased surface area from conditions like emphysema, or increased membrane thickness from fibrosis. Adjustments are made