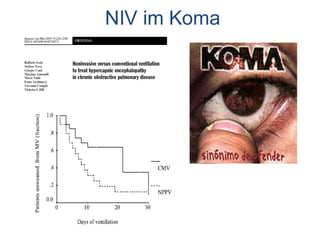
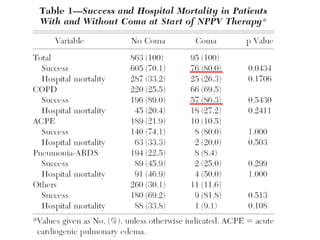
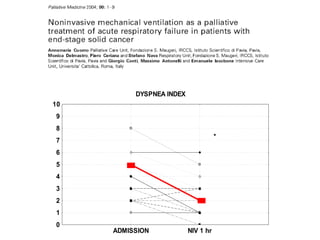
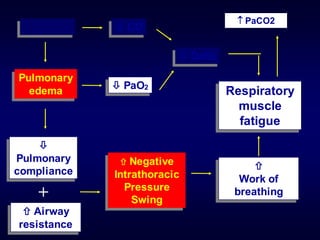
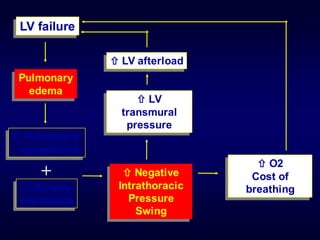
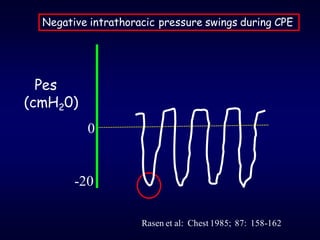
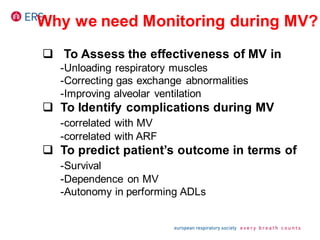
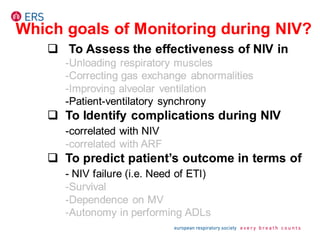
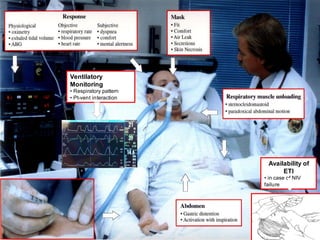
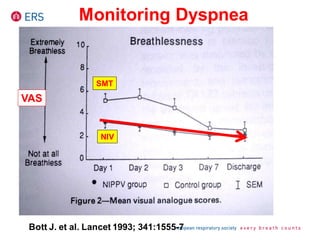
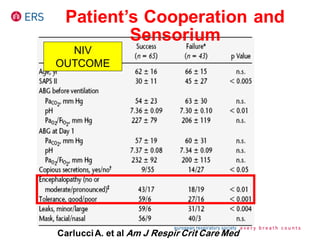
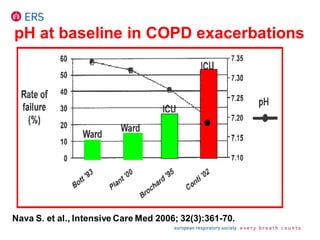
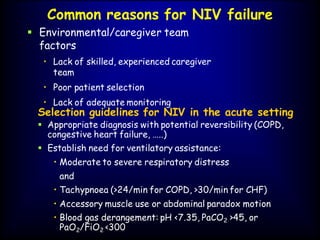
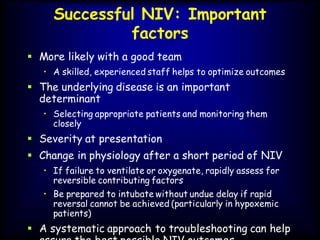
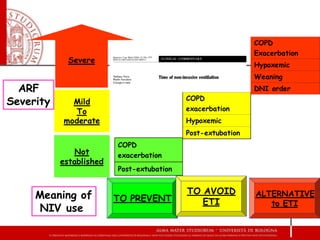
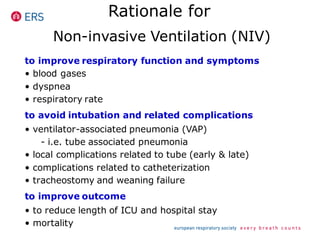
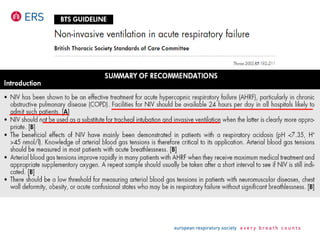
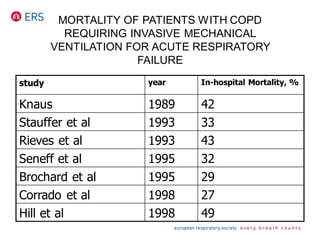
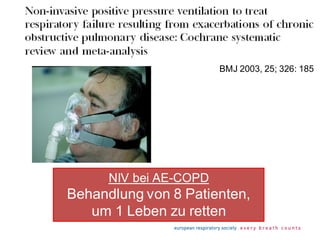
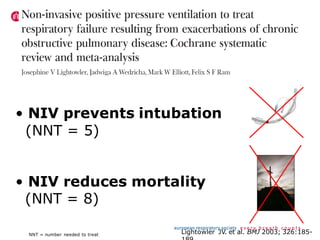
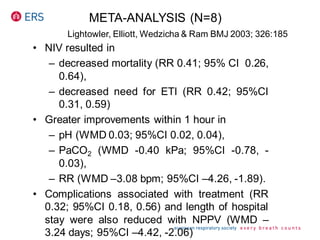
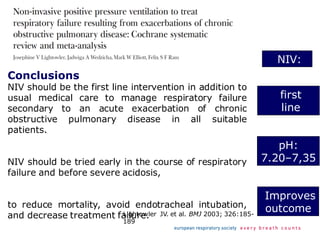
1) NIV is effective for acute hypercapnic respiratory failure caused by COPD exacerbations to prevent intubation and reduce mortality.
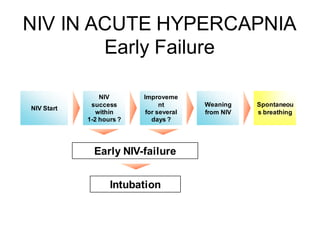
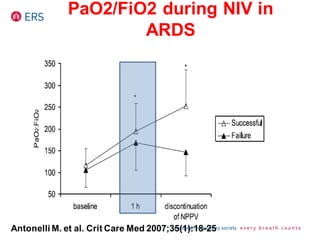
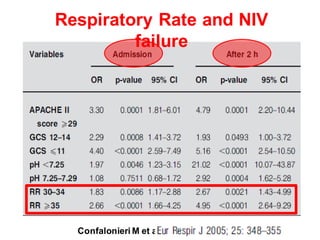
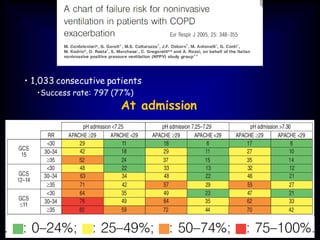
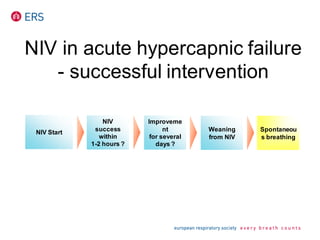
2) NIV is most effective when started early in respiratory failure before severe acidosis develops. It improves blood gases and respiratory status within 1-2 hours.
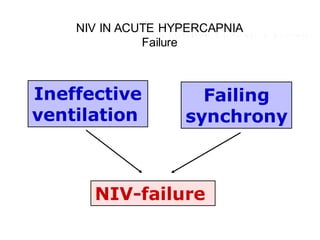
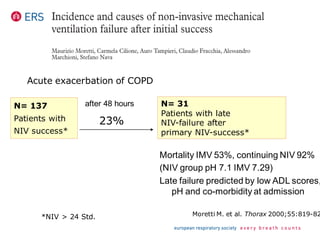
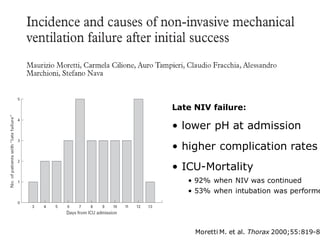
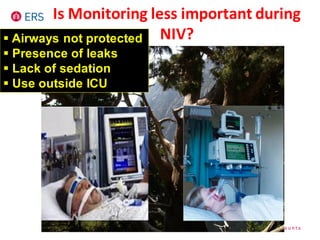
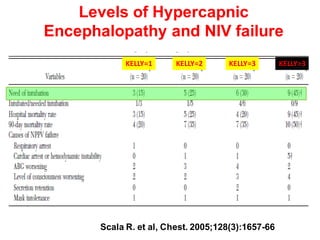
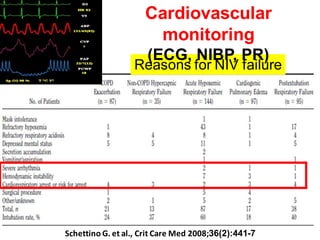
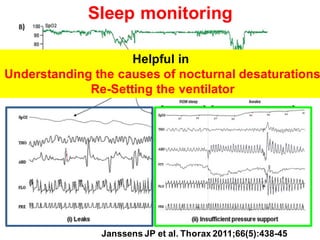
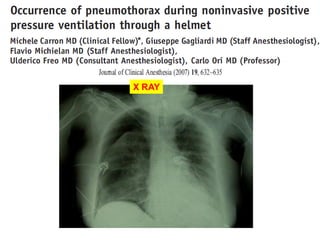
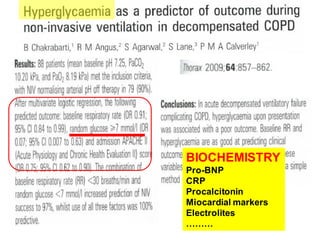
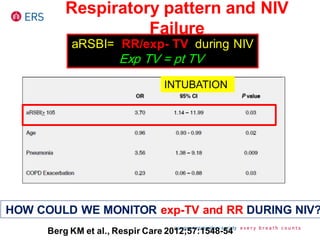
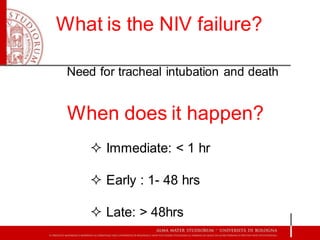
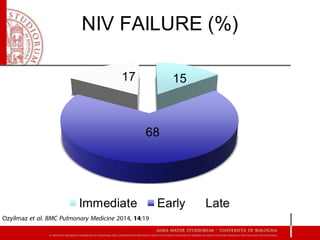
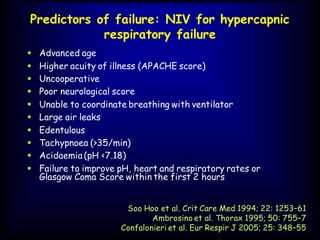
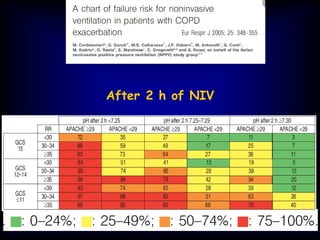
3) While NIV success rates are high initially, late failure can still occur in around 23% of patients and is associated with increased mortality if intubation is then required. Close monitoring is needed.




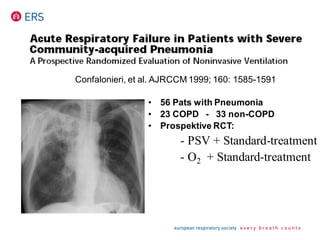
![Am J Respir Crit Care Med 1999;160:1585-15
*
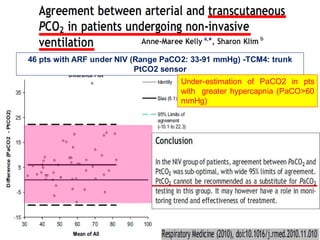
PaCO2 [mmHg]
Intubation [%]
ICU – length of stay [d]
2-Mo-moratliy [%]
NIV Standard
73
0
<1
11
68
55
8
63
32
38
3
43
34
47
5
33
NIV Standard
*p < 0.05
COPD (n = 23) Non-COPD (n = 33)
* *
*
* *](https://image.slidesharecdn.com/nivinacuesettings-160924232947/85/NIV-in-Acute-settings-45-320.jpg)