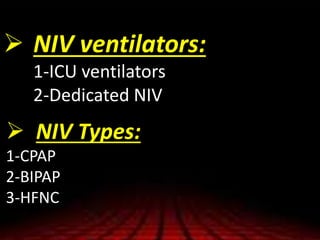
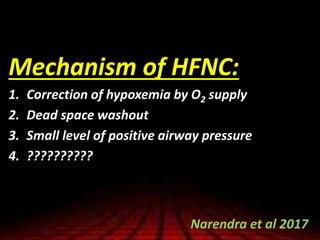
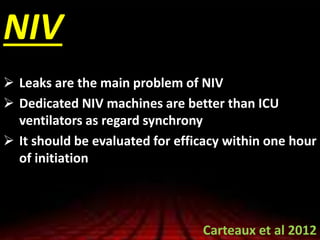
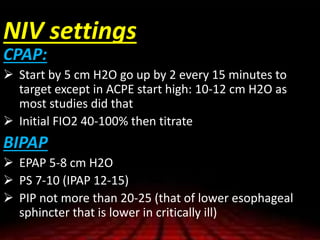
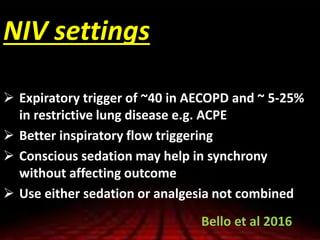
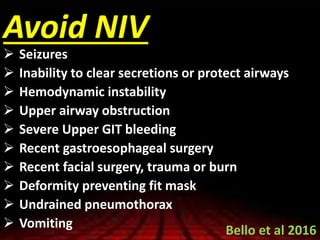
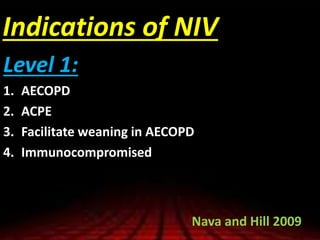
Non-invasive ventilation (NIV) is an effective treatment for acute respiratory failure, particularly in conditions like acute exacerbations of COPD and acute cardiogenic pulmonary edema, offering benefits such as improved oxygenation and reduced need for intubation. Different NIV types (CPAP, BiPAP, and HFNC) are recommended for specific conditions, but factors like patient cooperation and mask fit are crucial for success. However, NIV is not recommended for certain patient groups, such as those with altered mental status or rapidly progressive neuromuscular diseases, and its efficacy should be evaluated quickly after initiation.