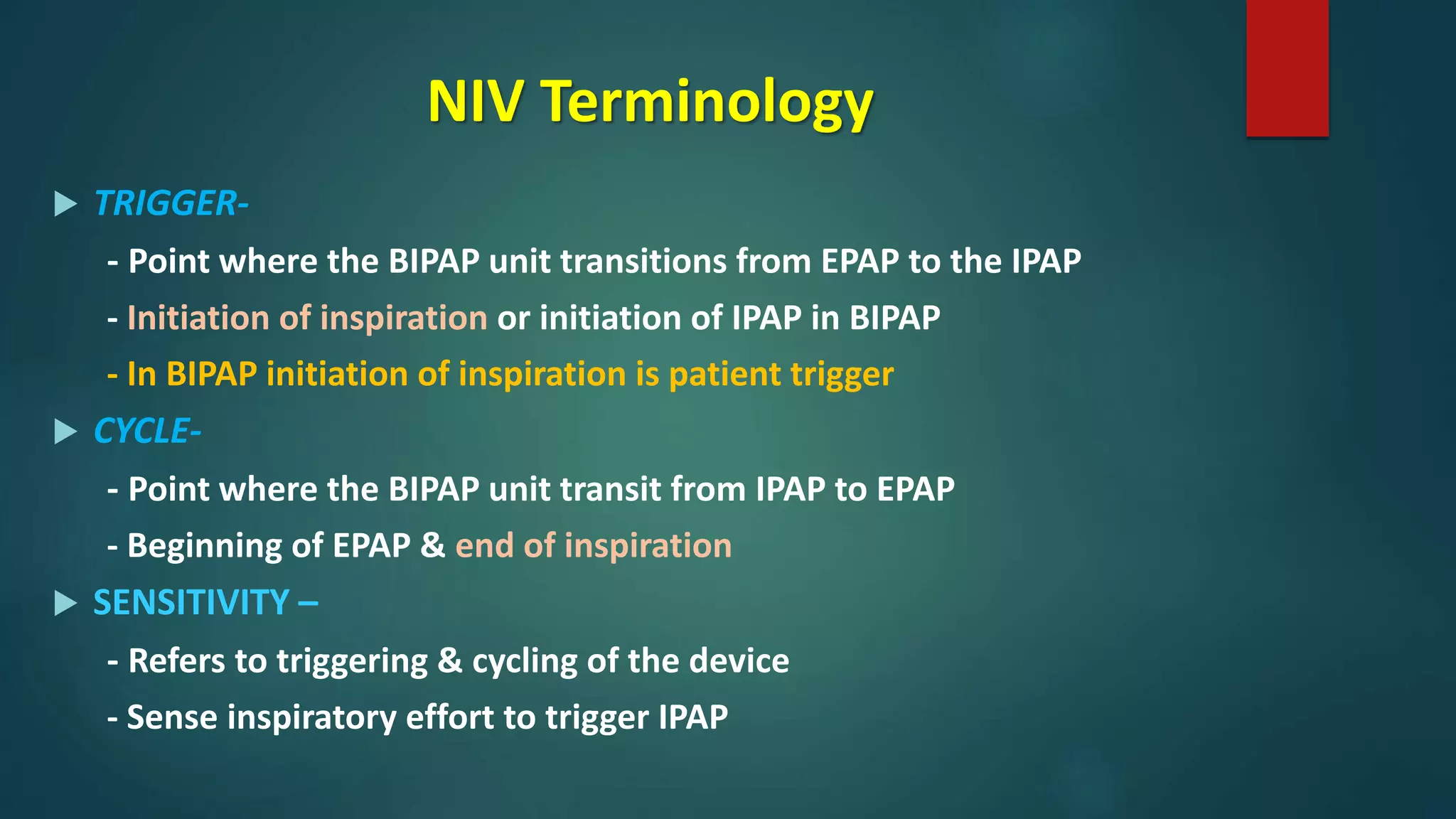
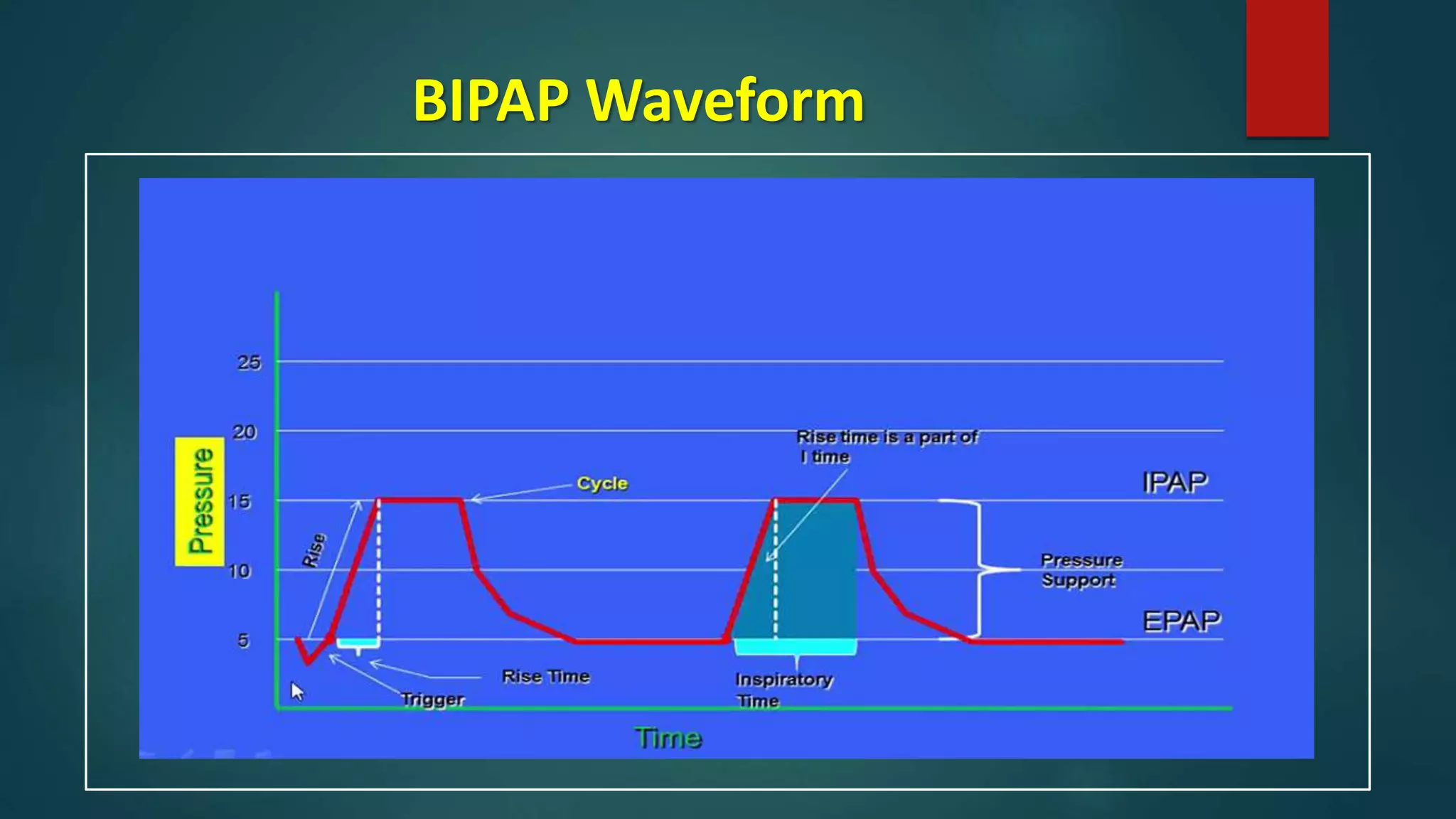
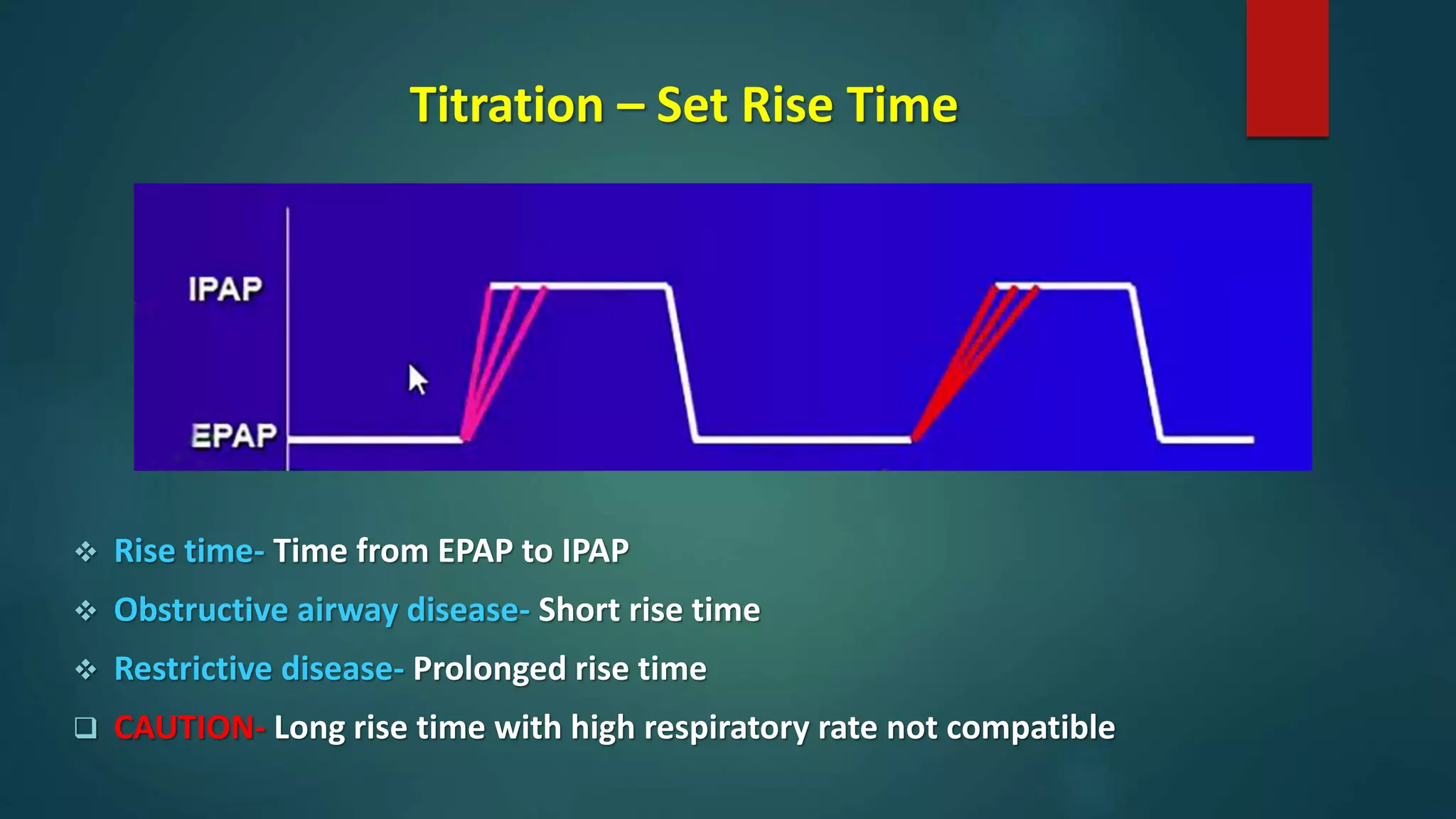
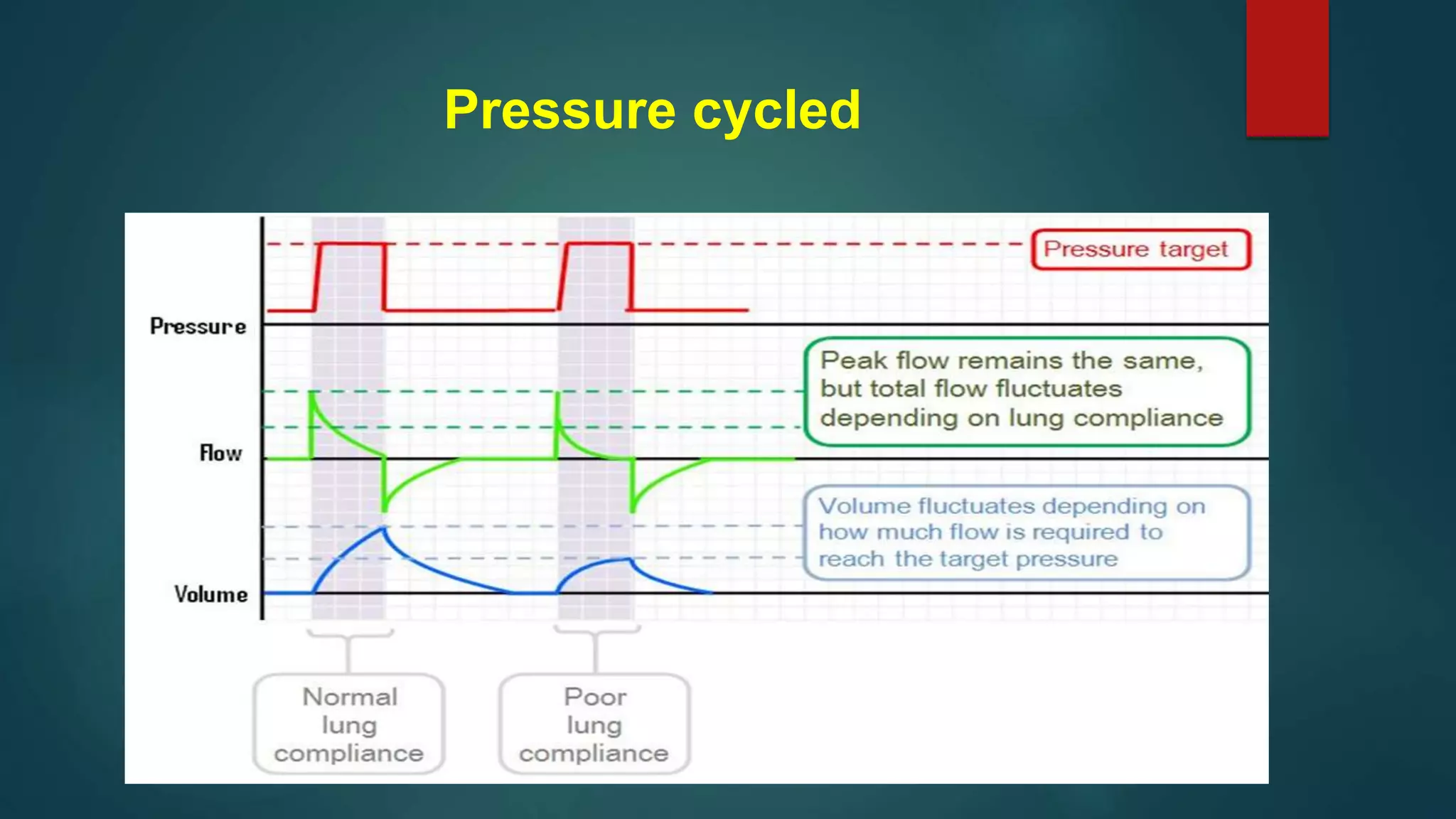
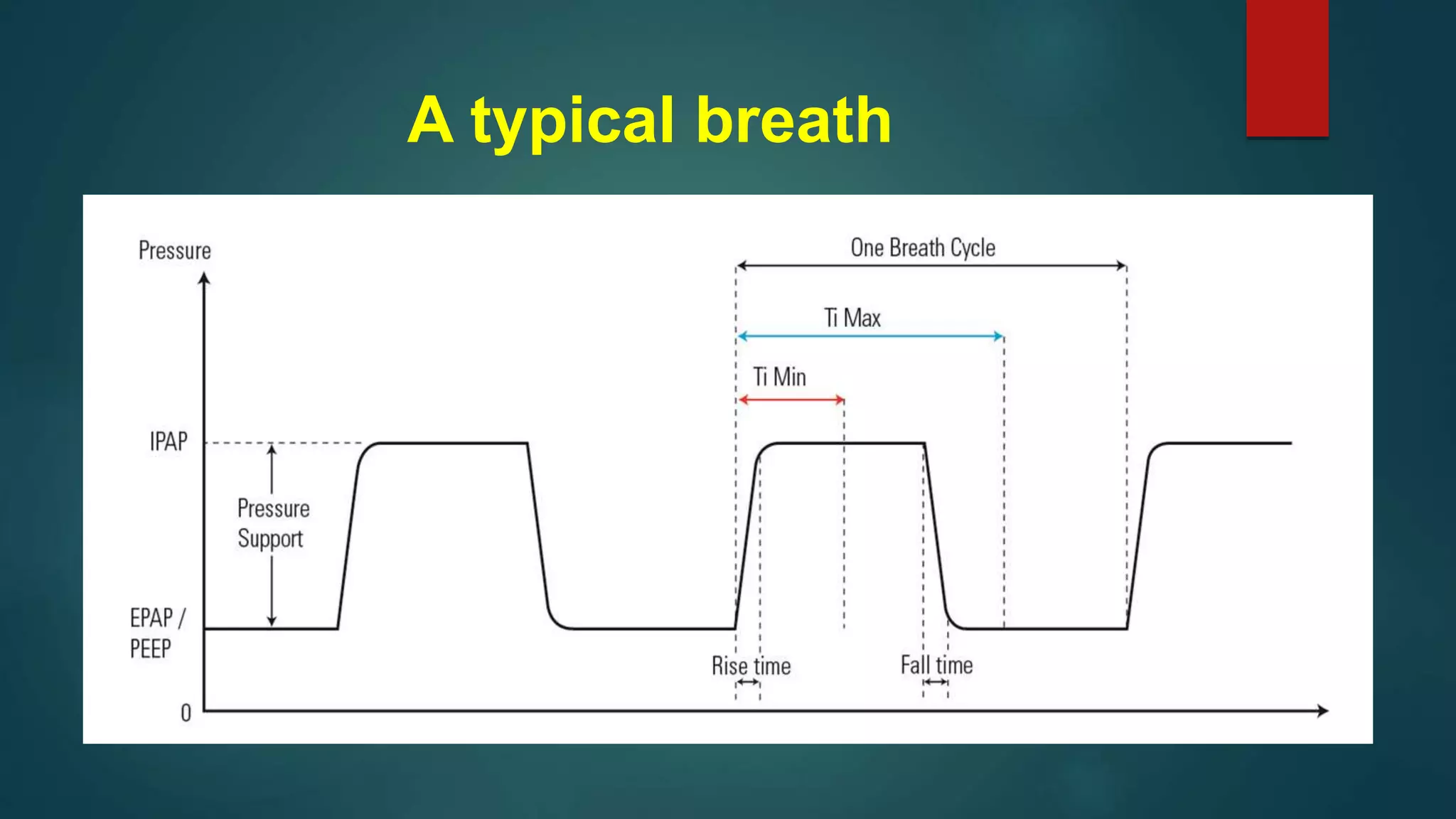
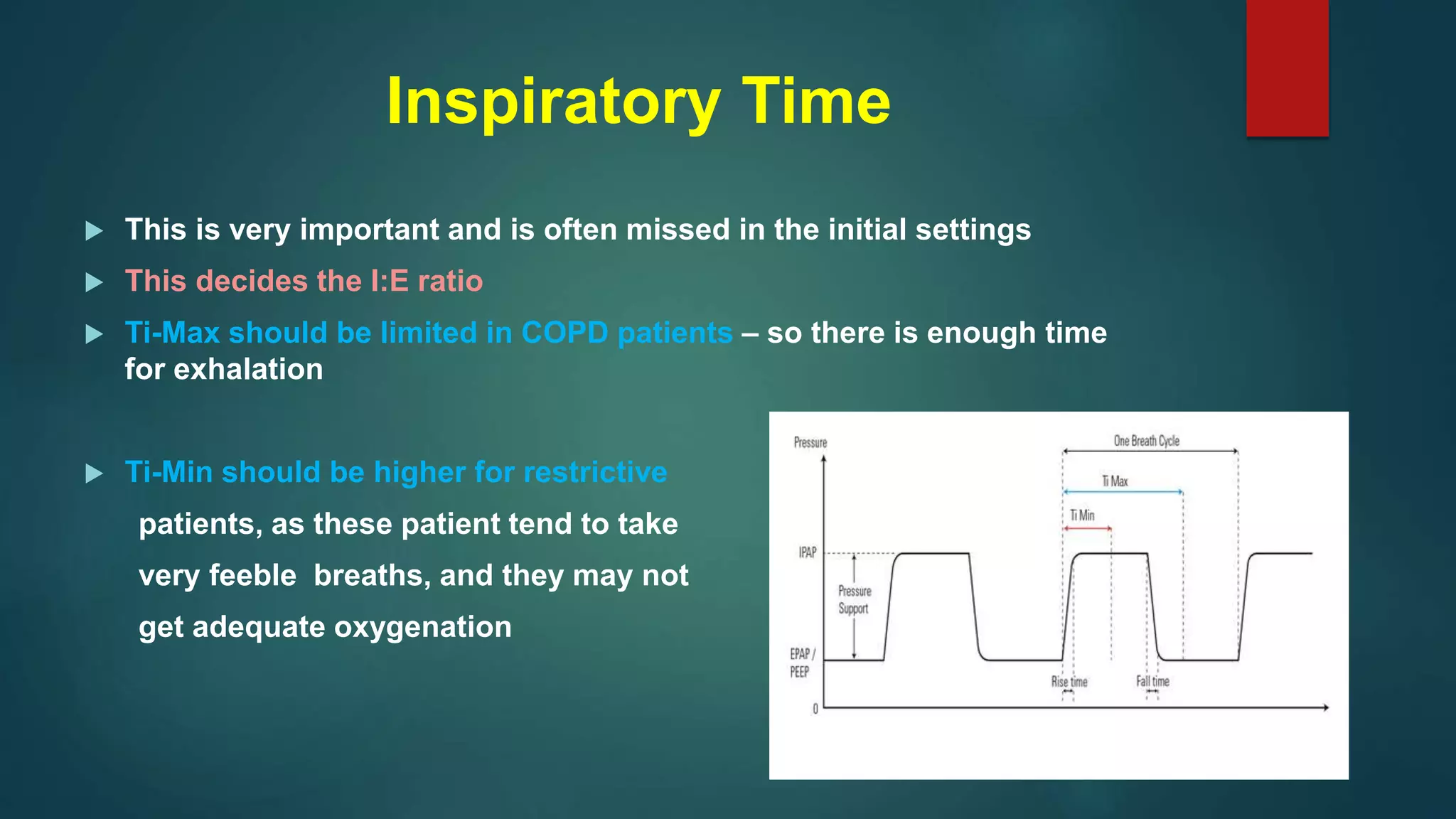
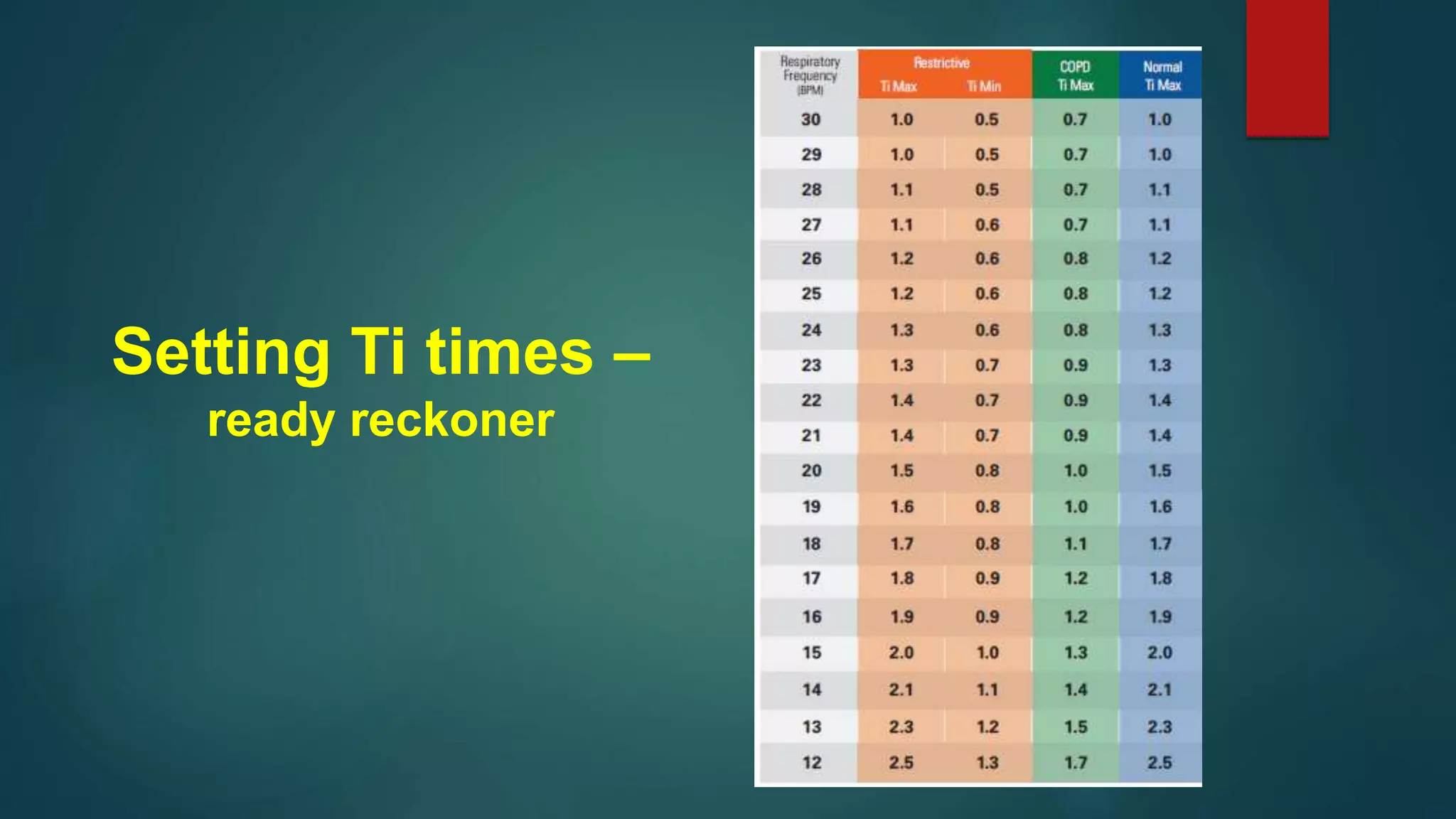
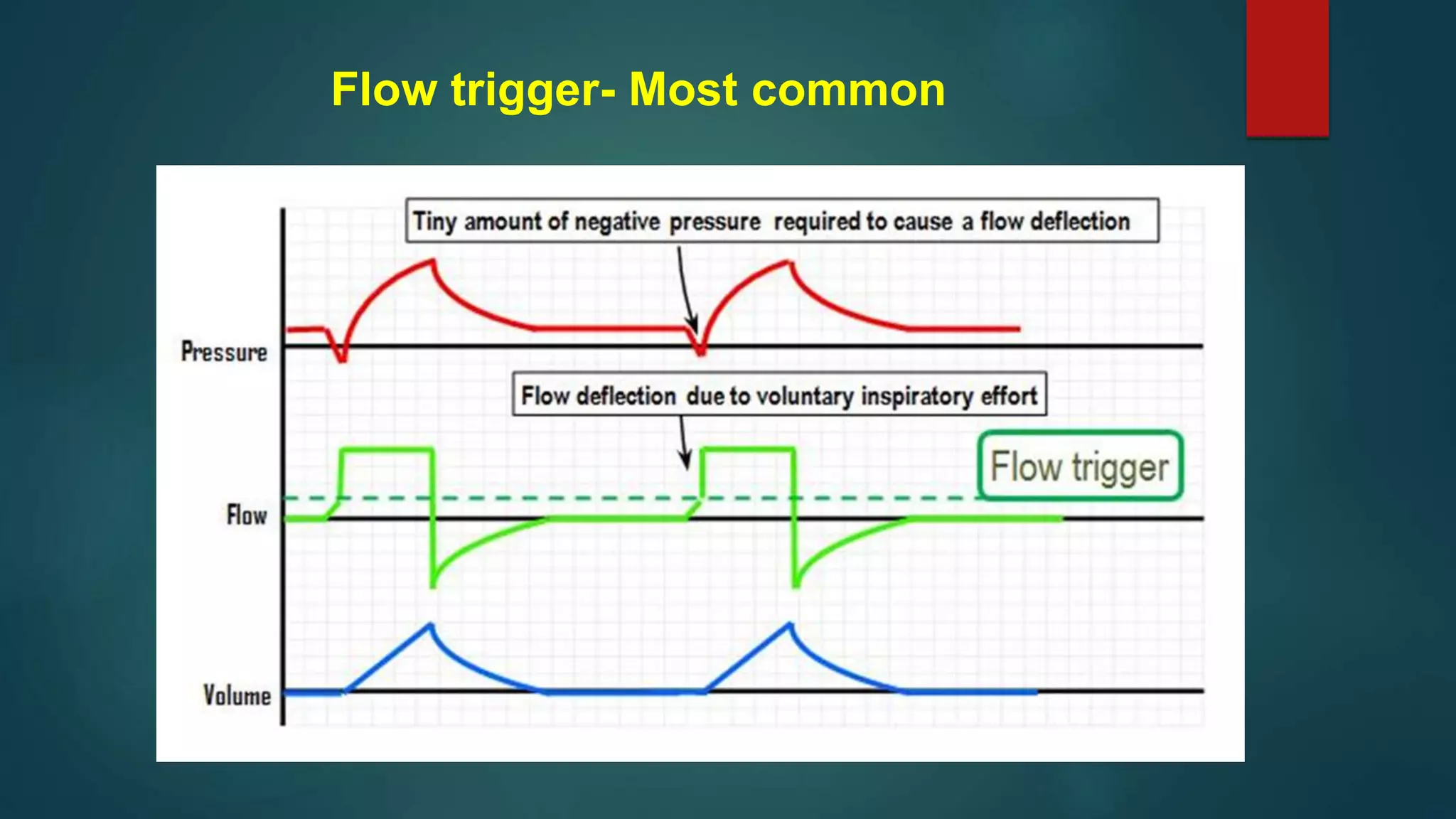
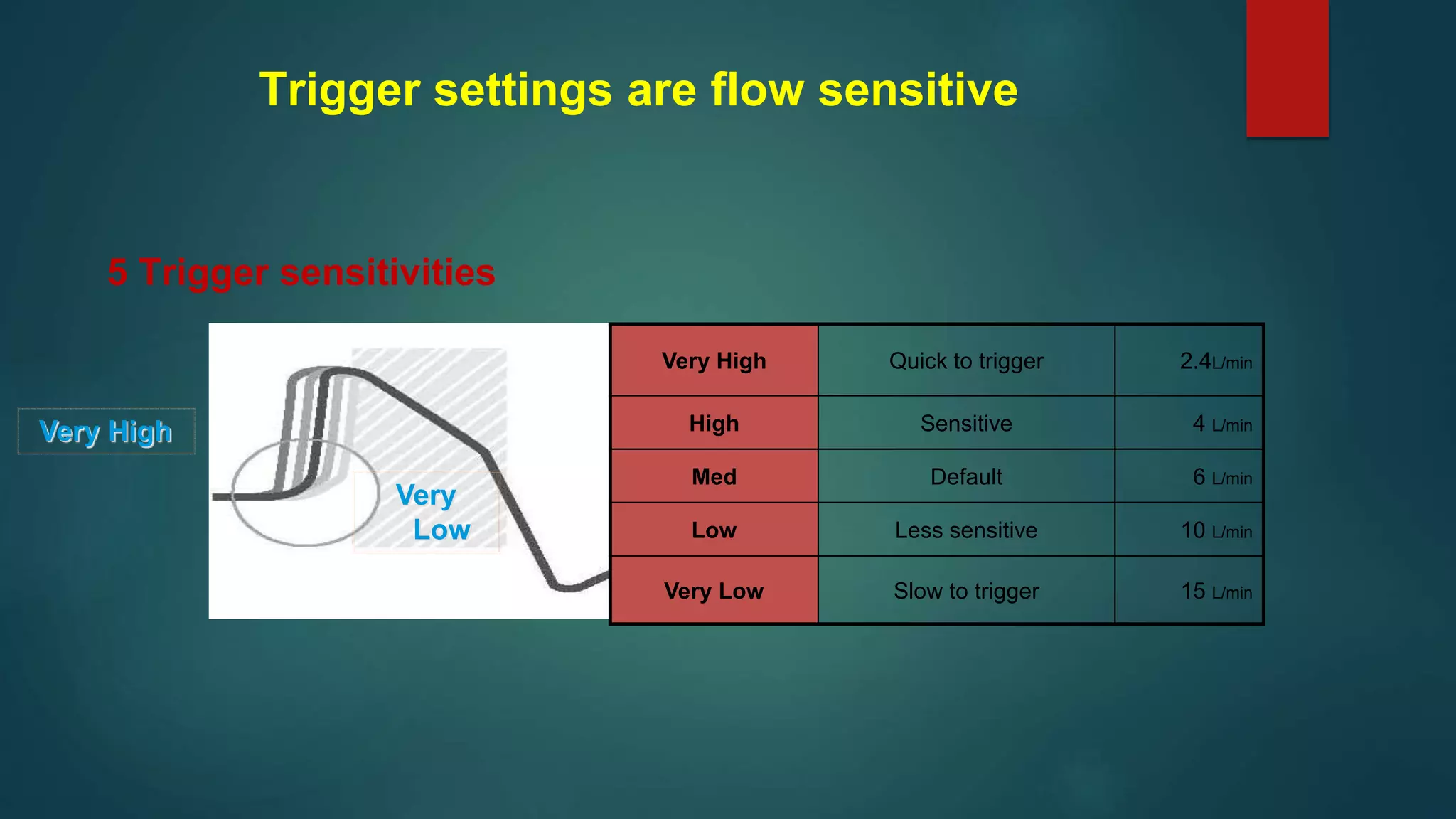
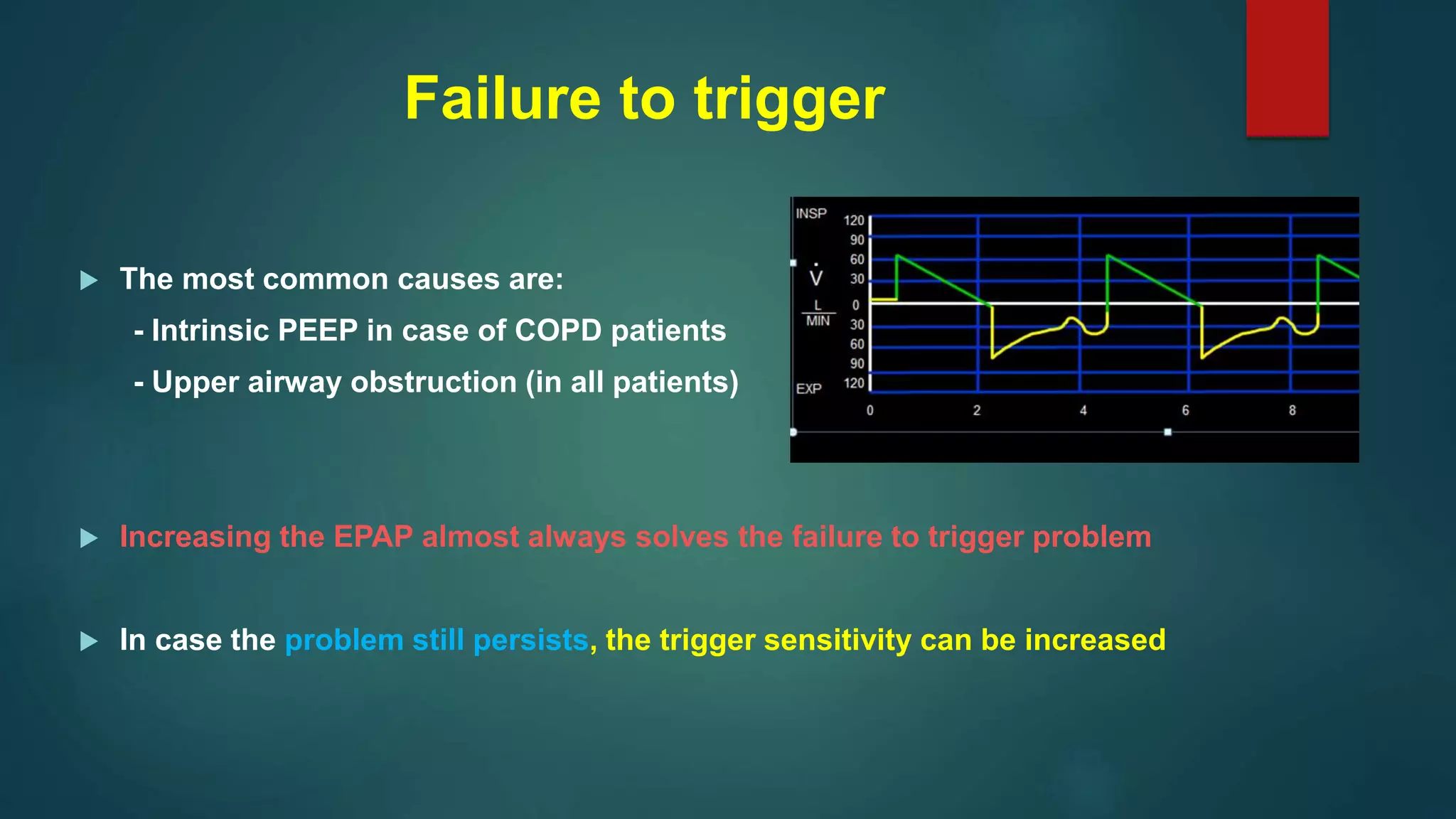
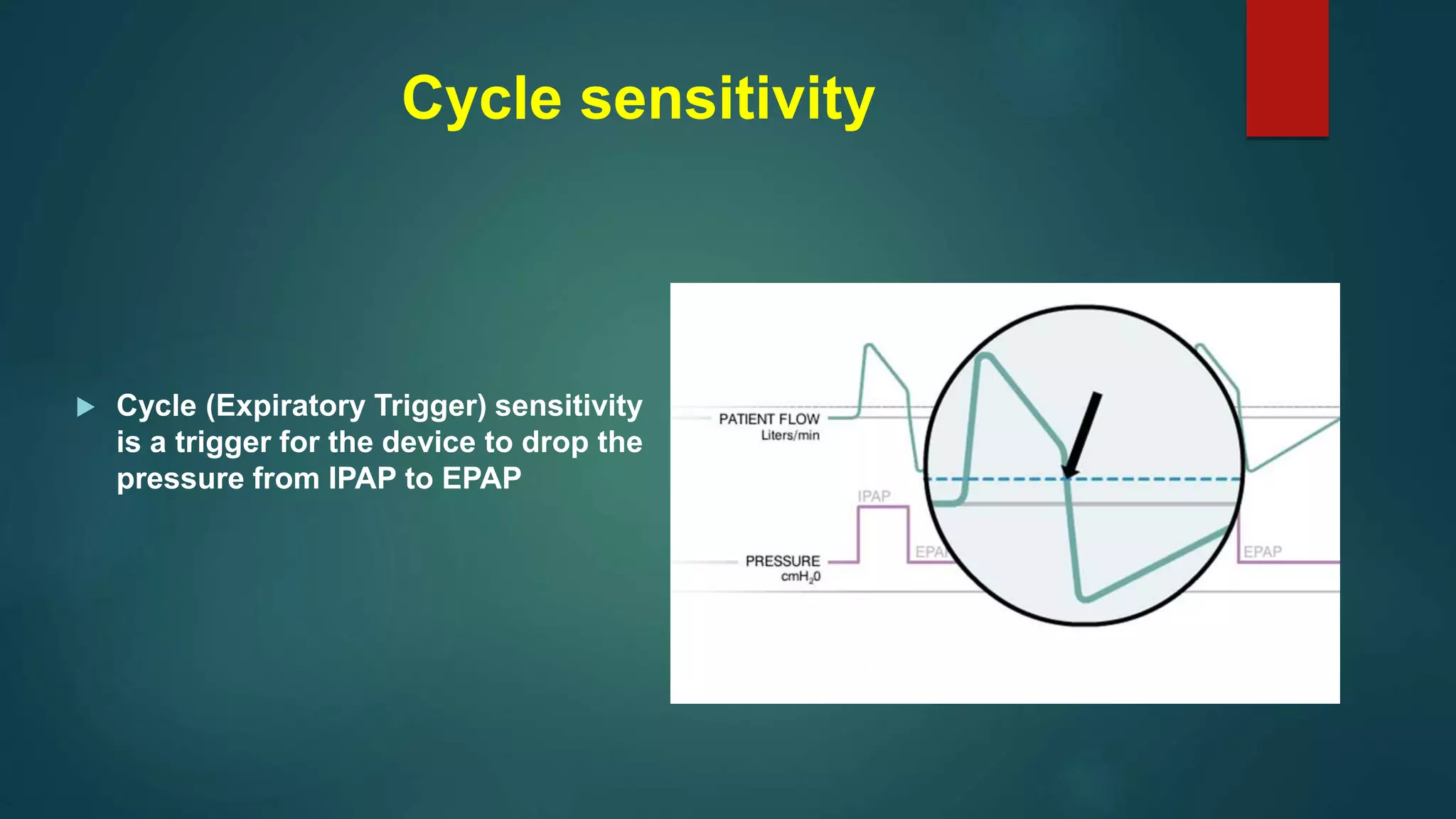
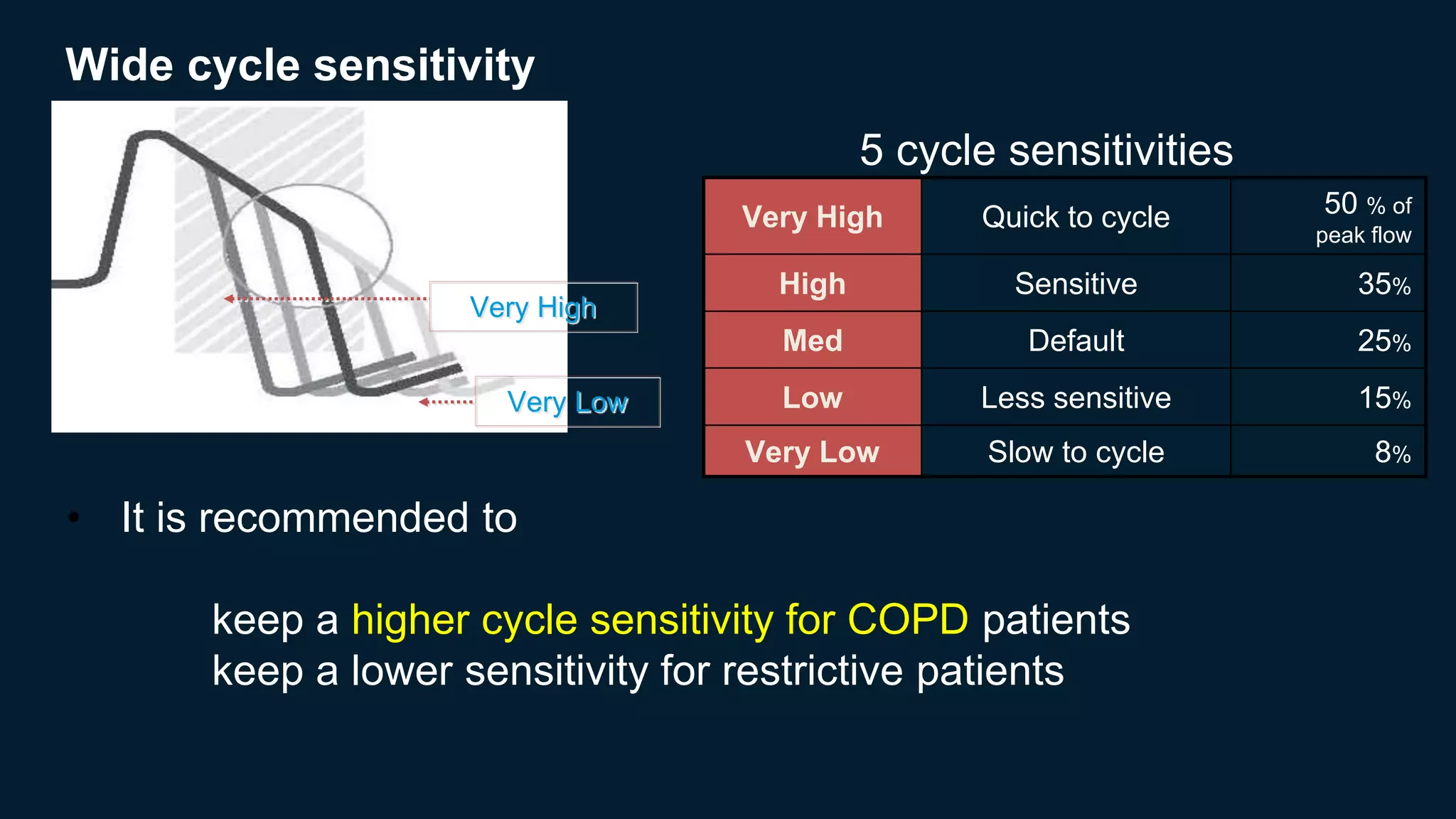
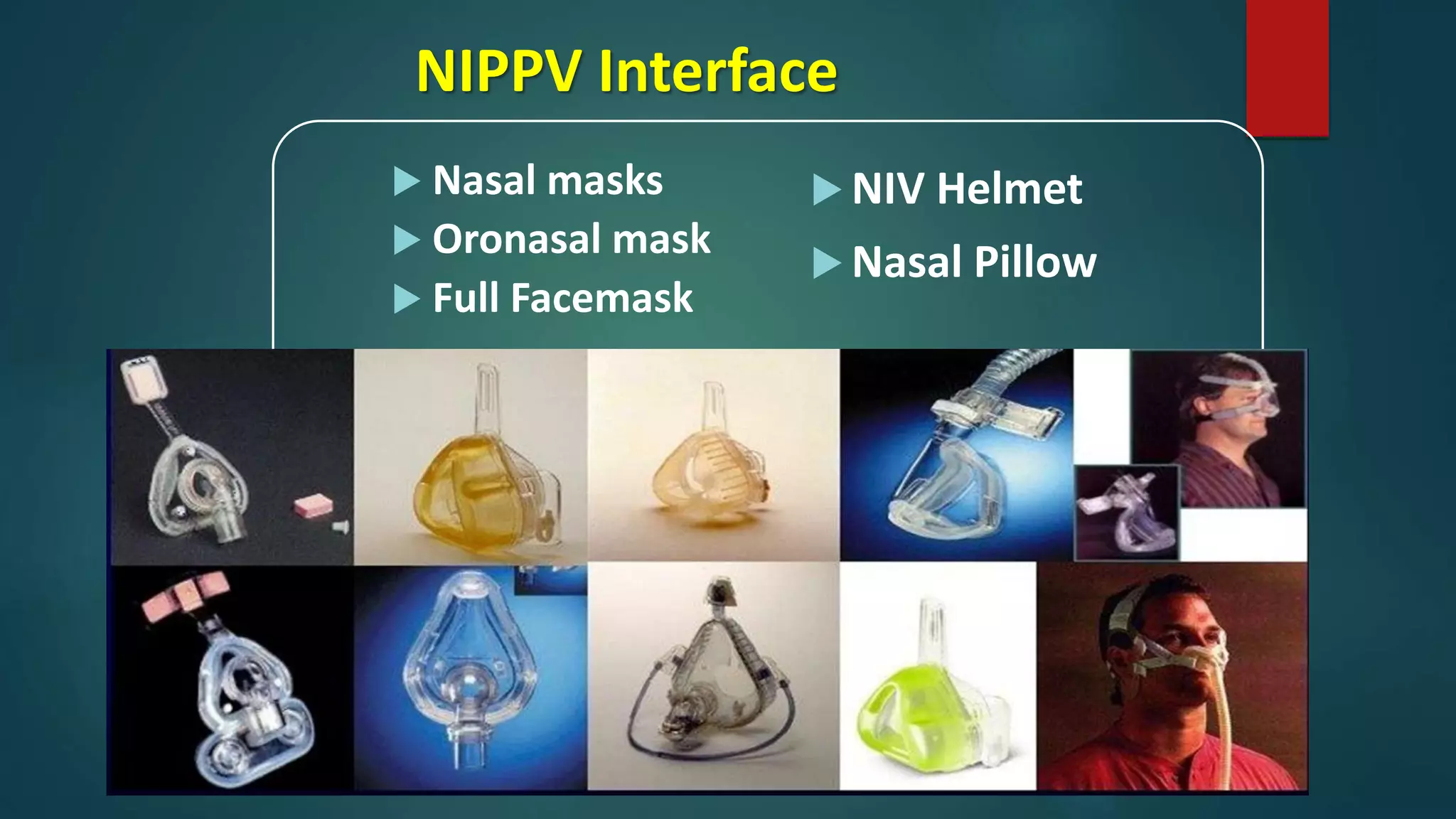
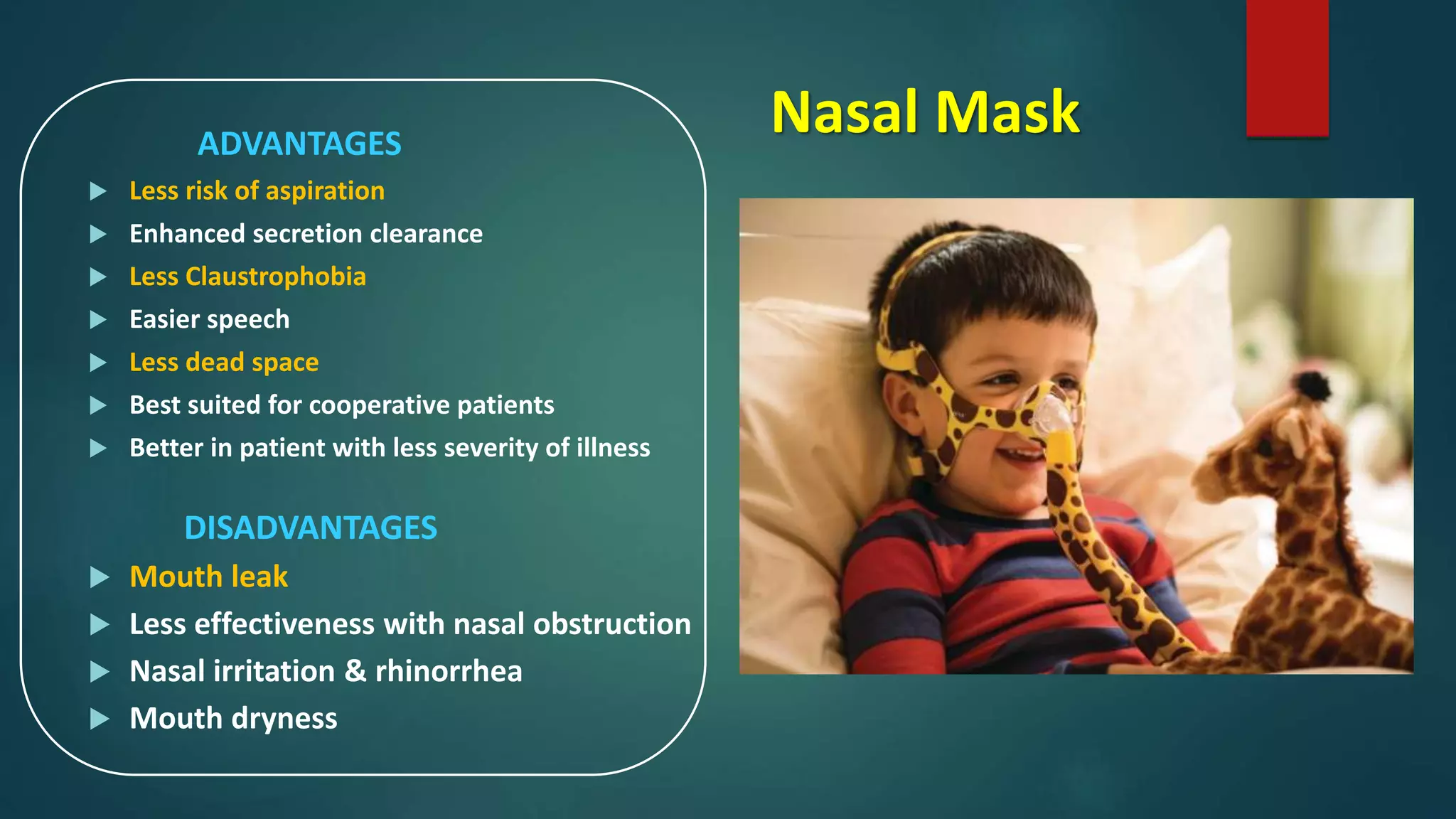
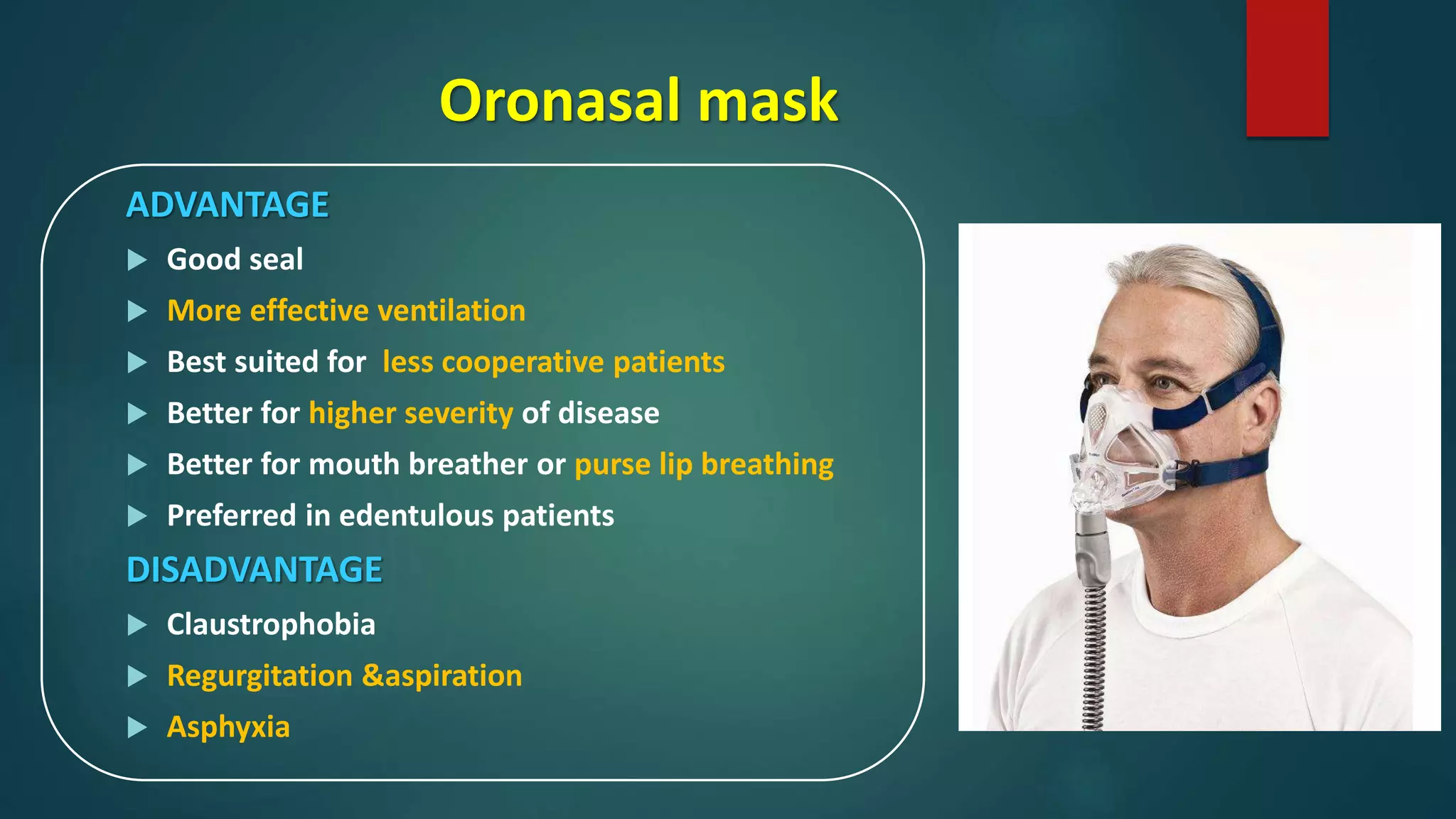
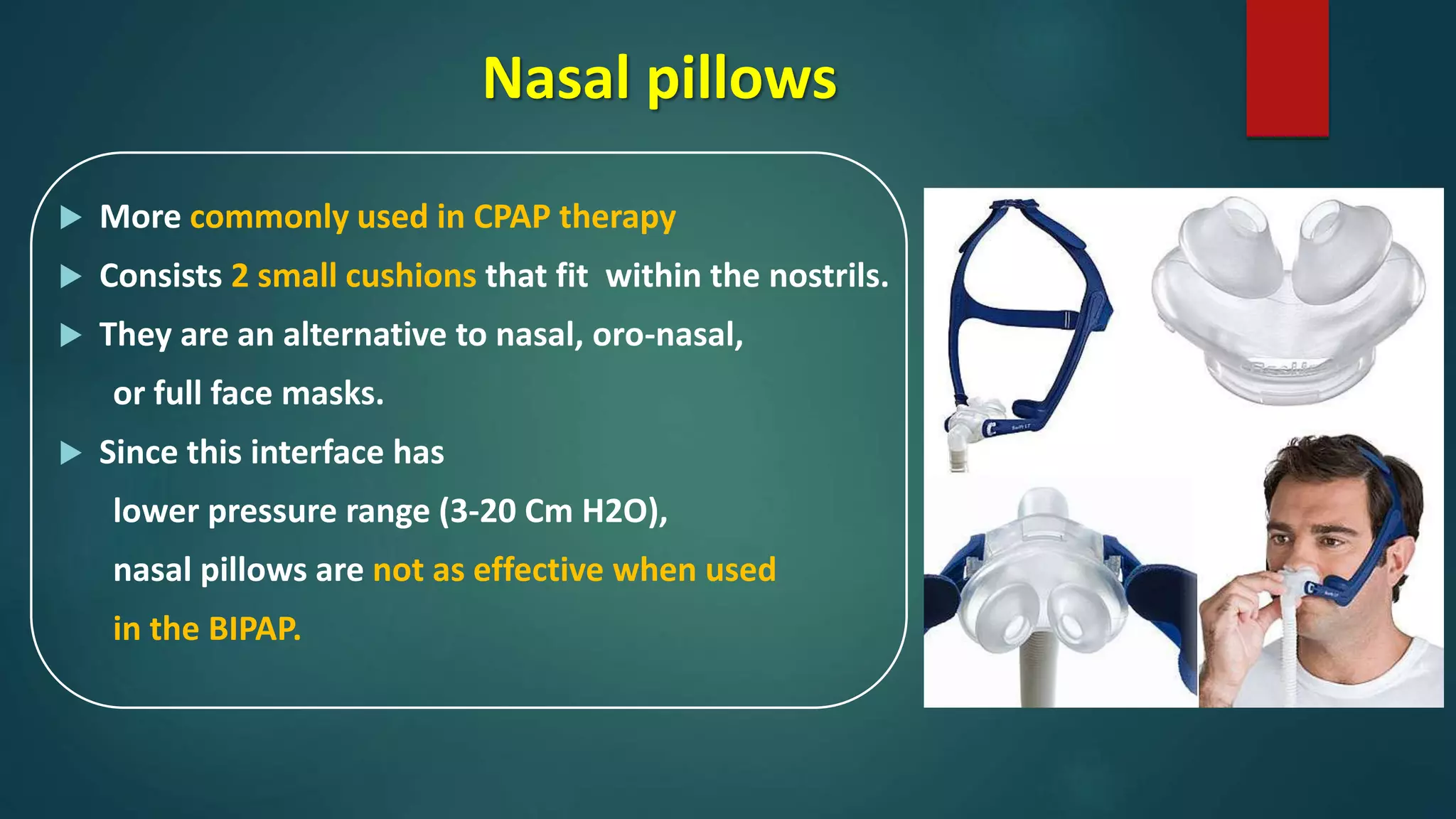
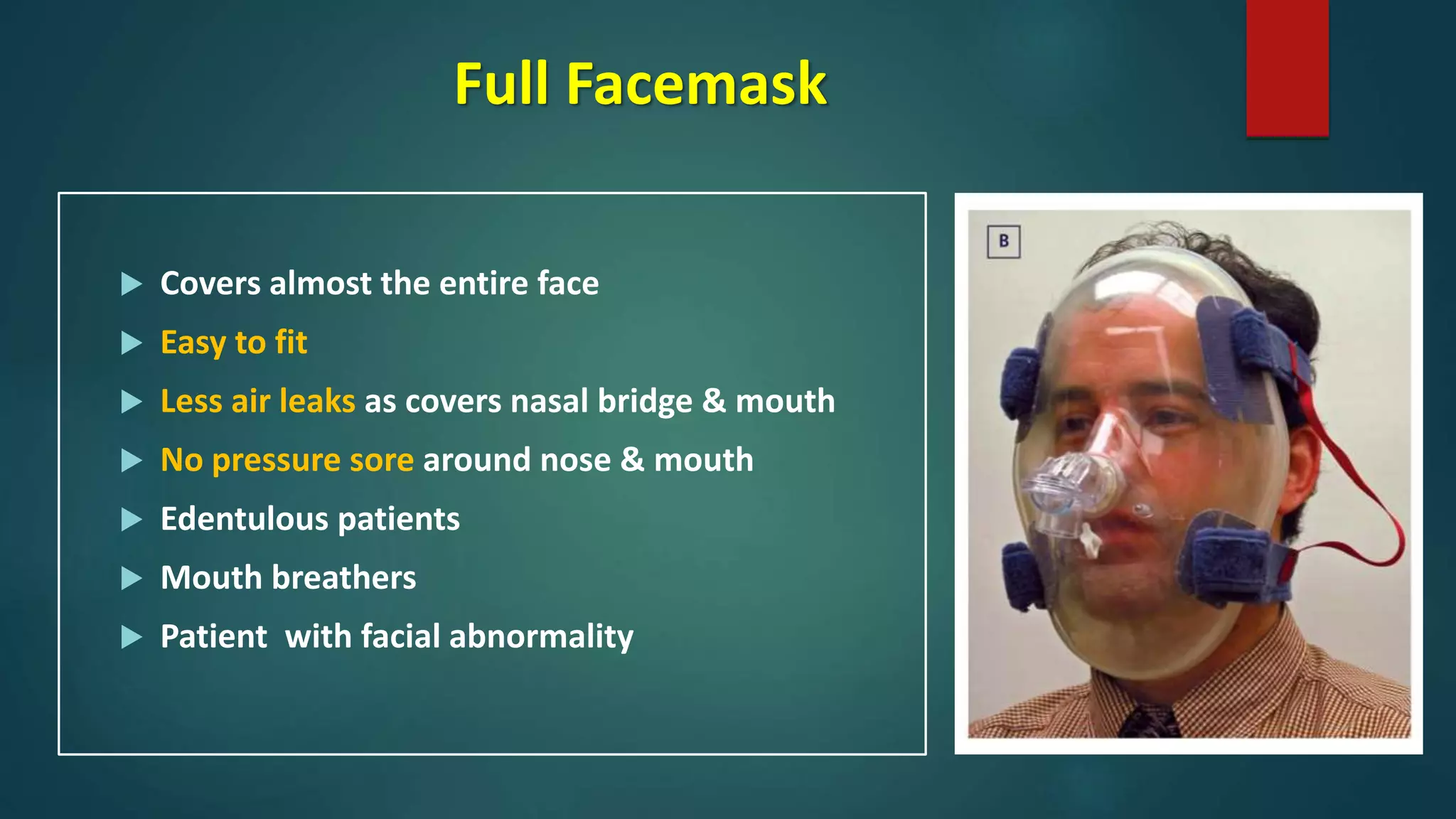
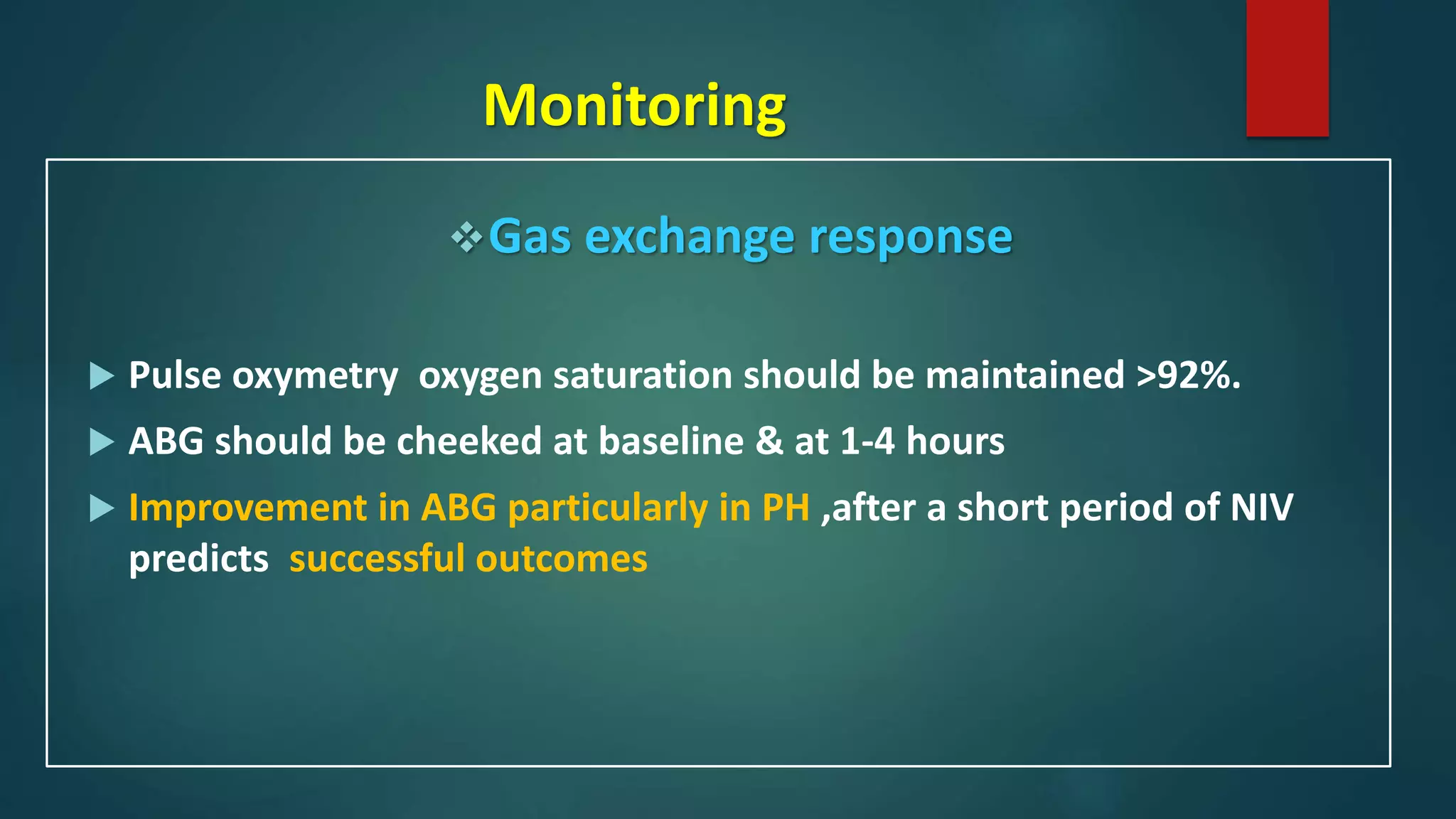
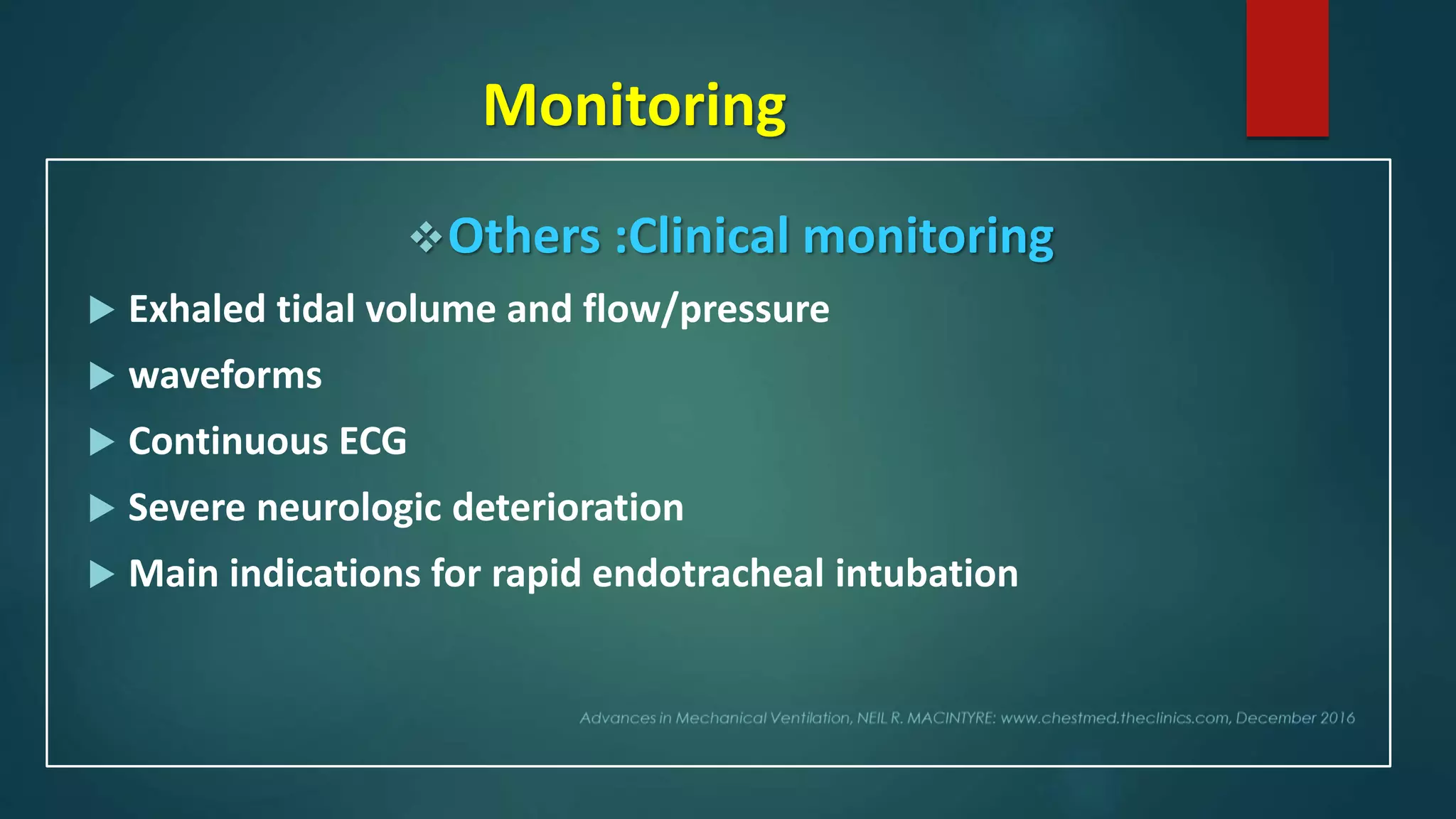
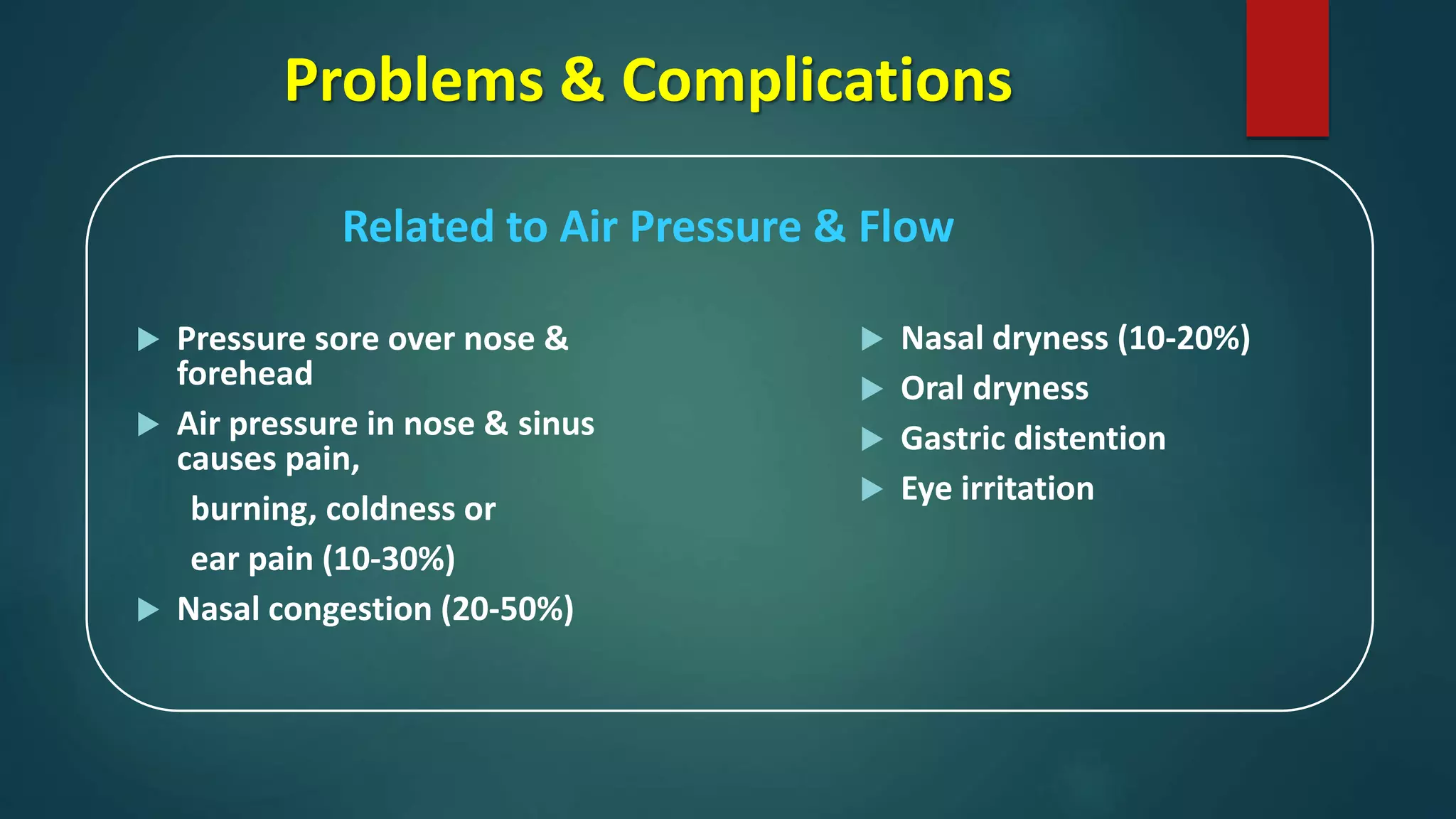
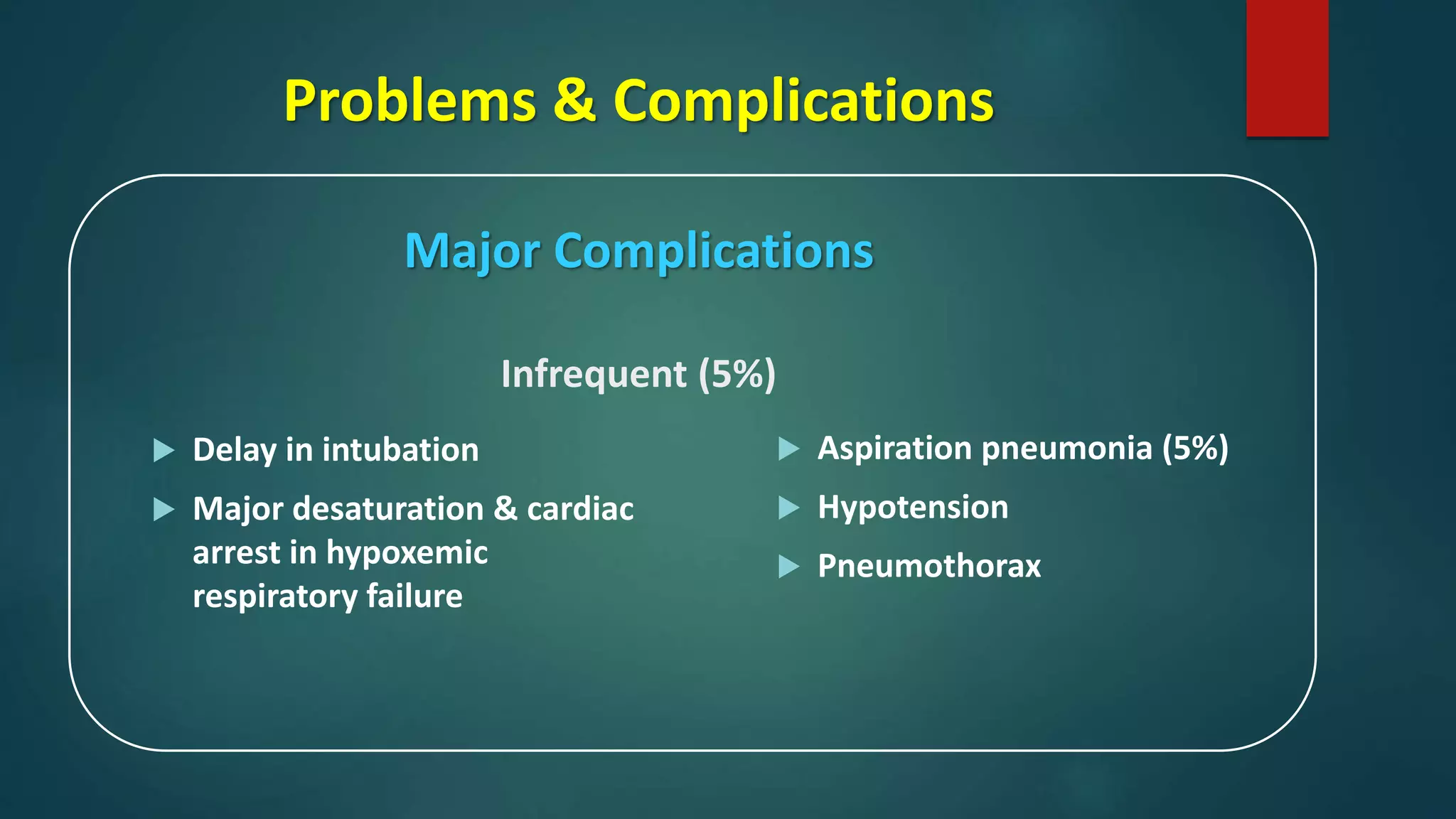
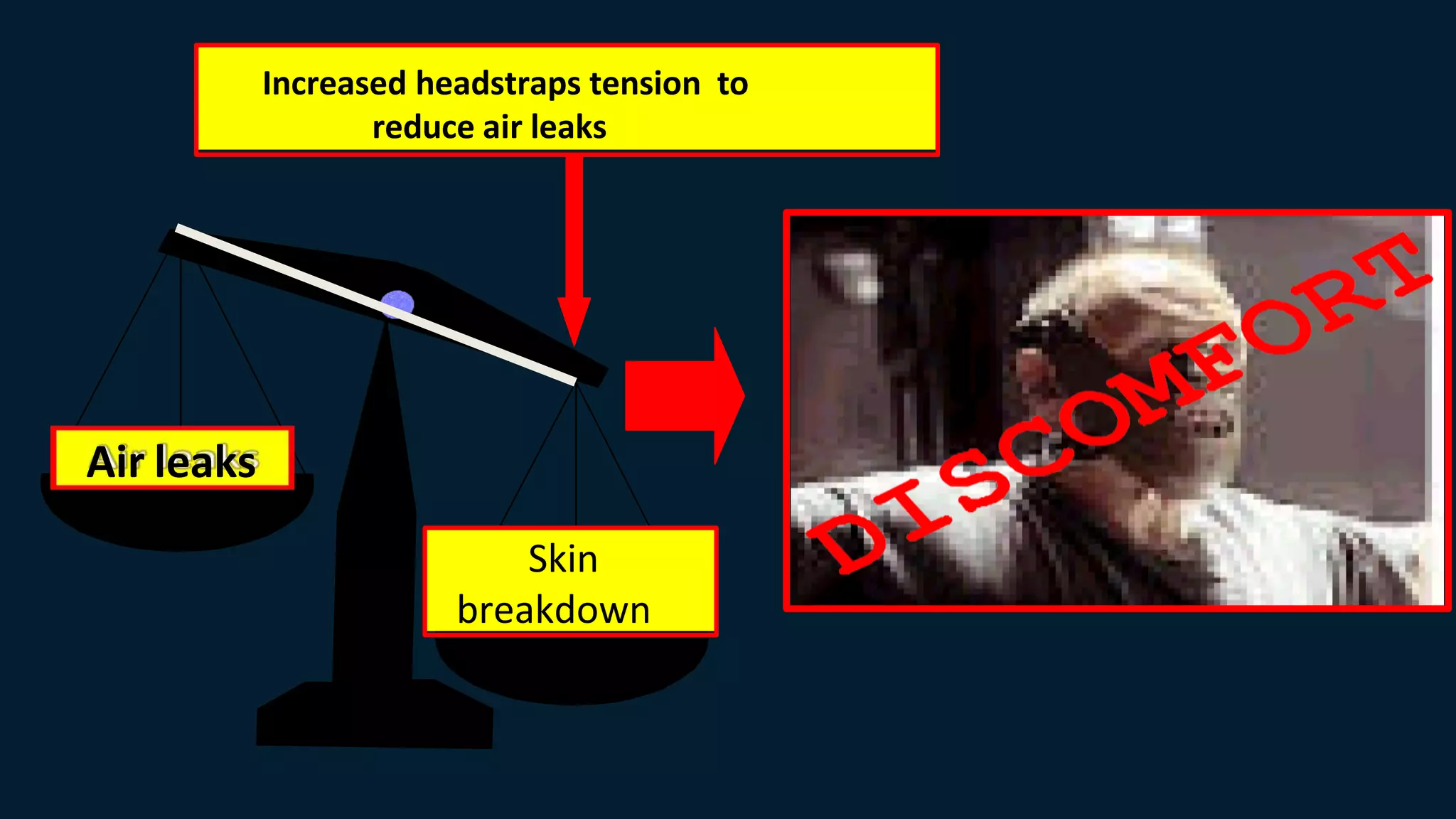
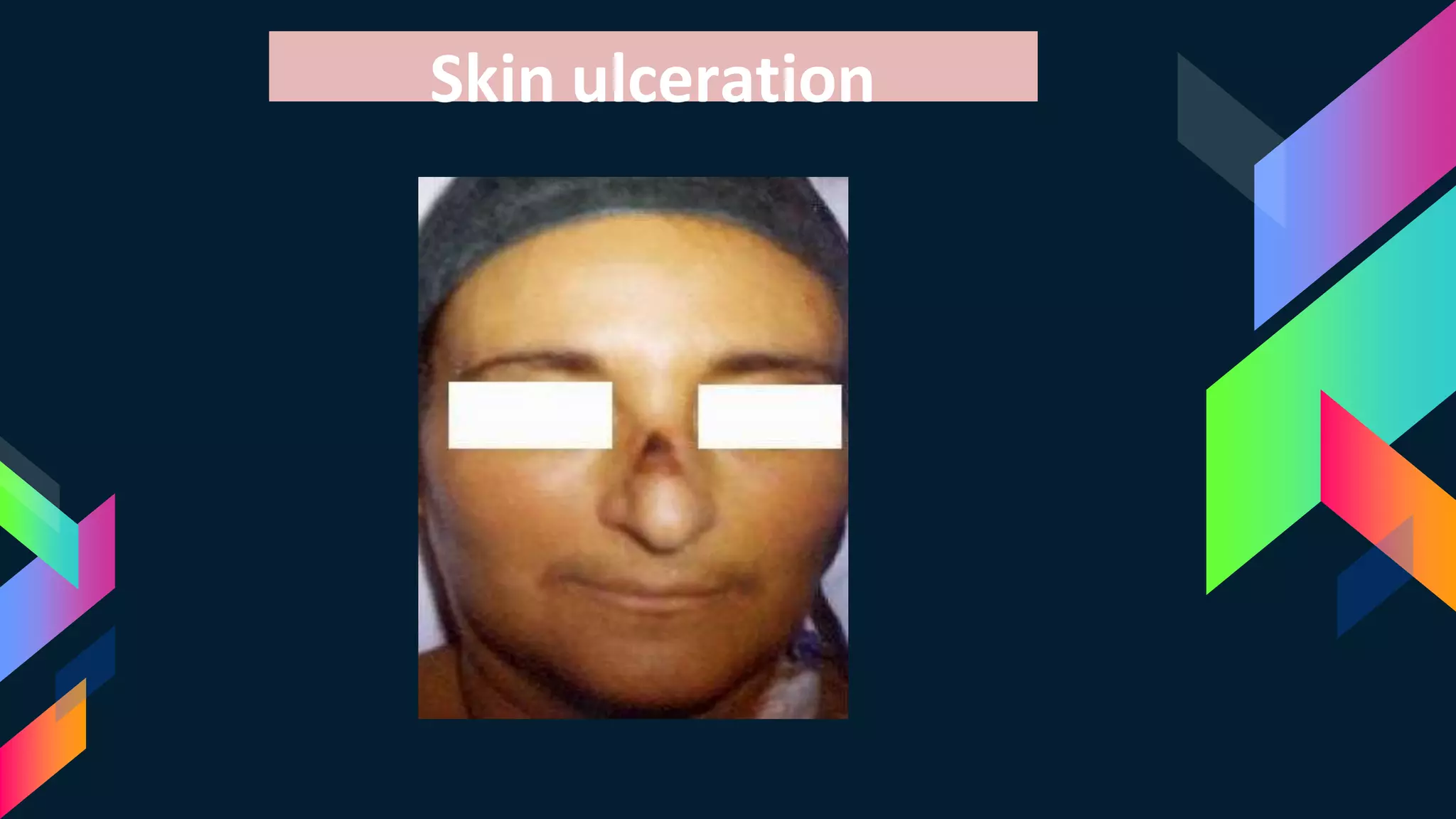
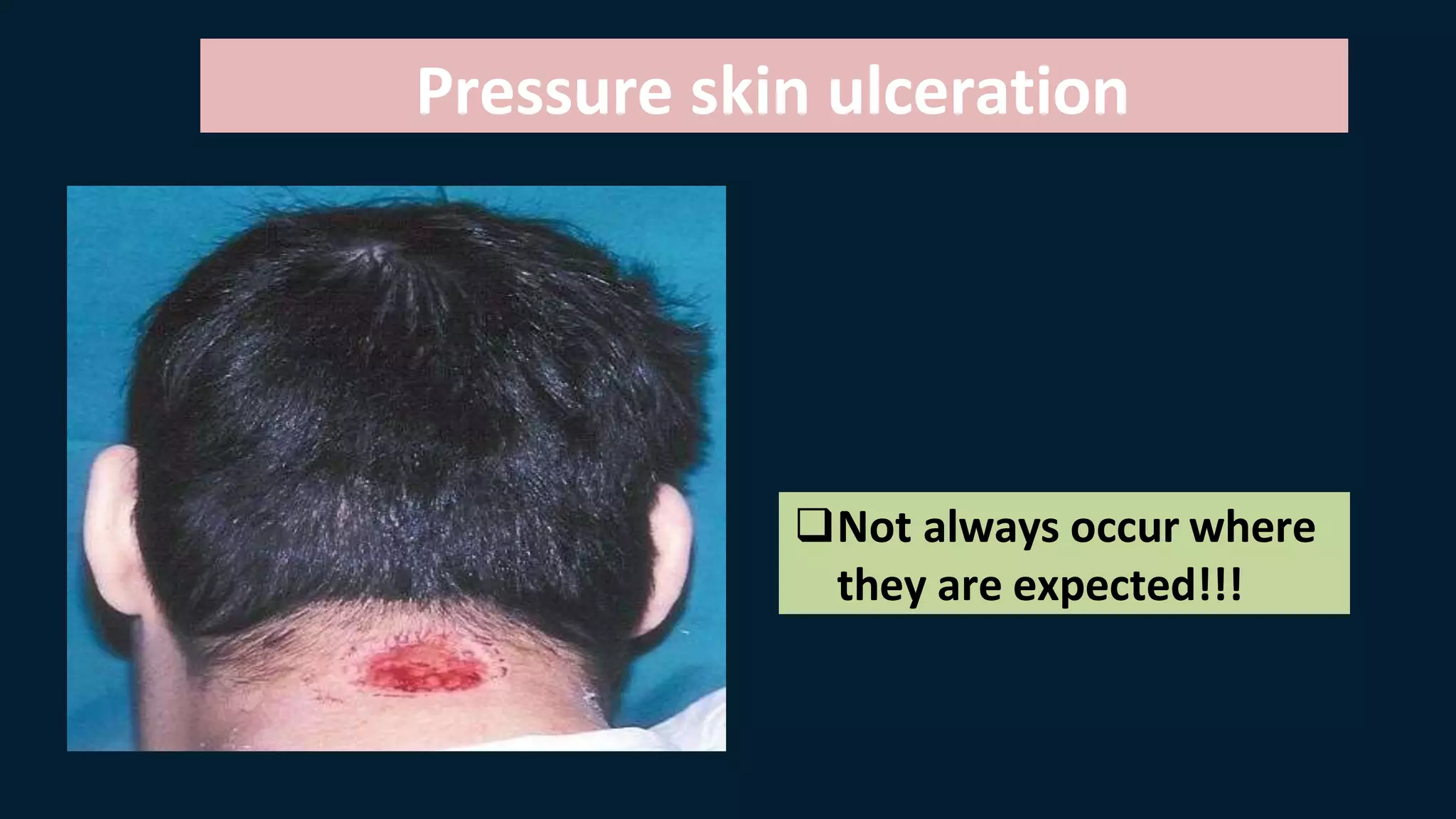
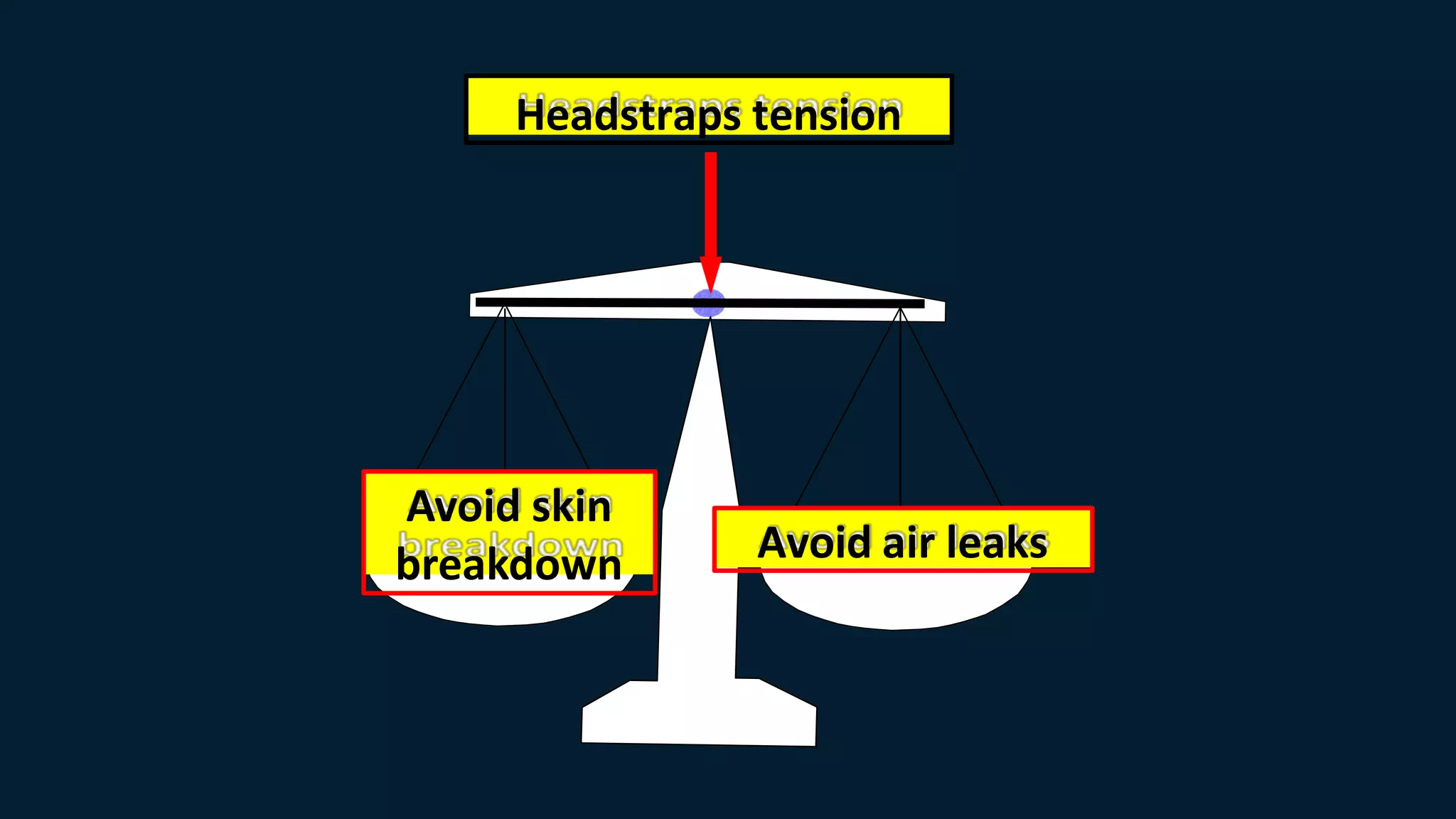
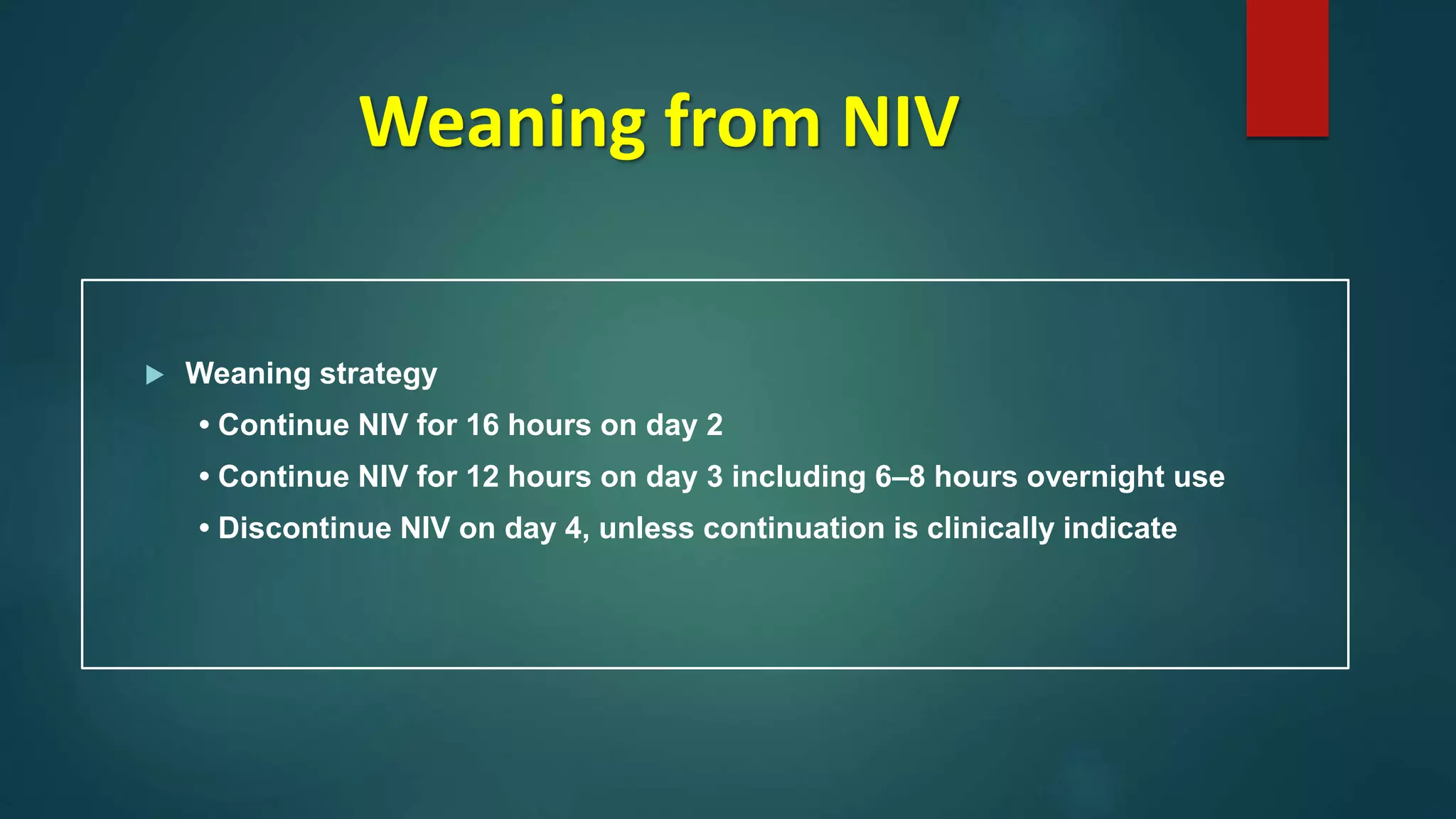
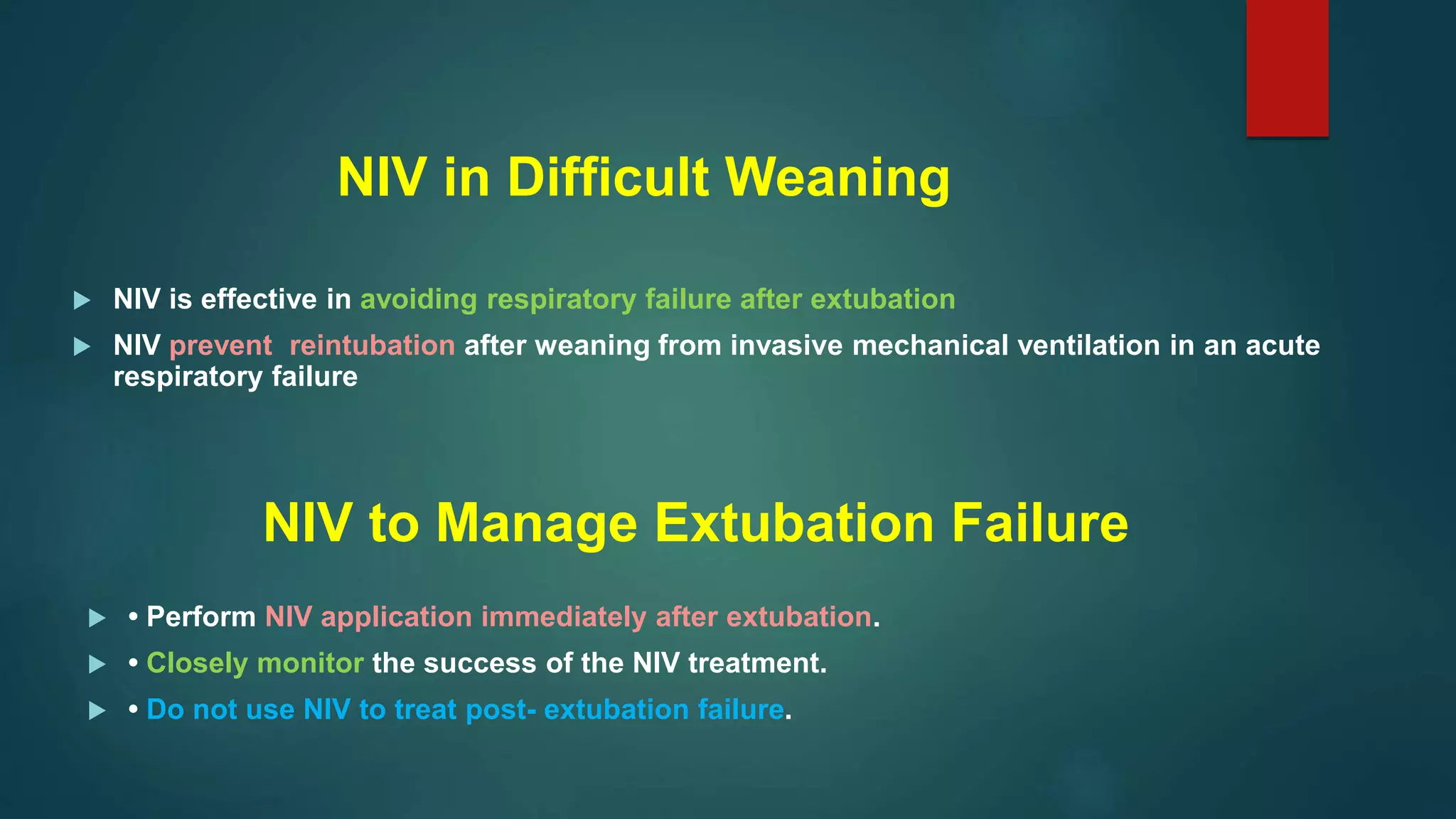
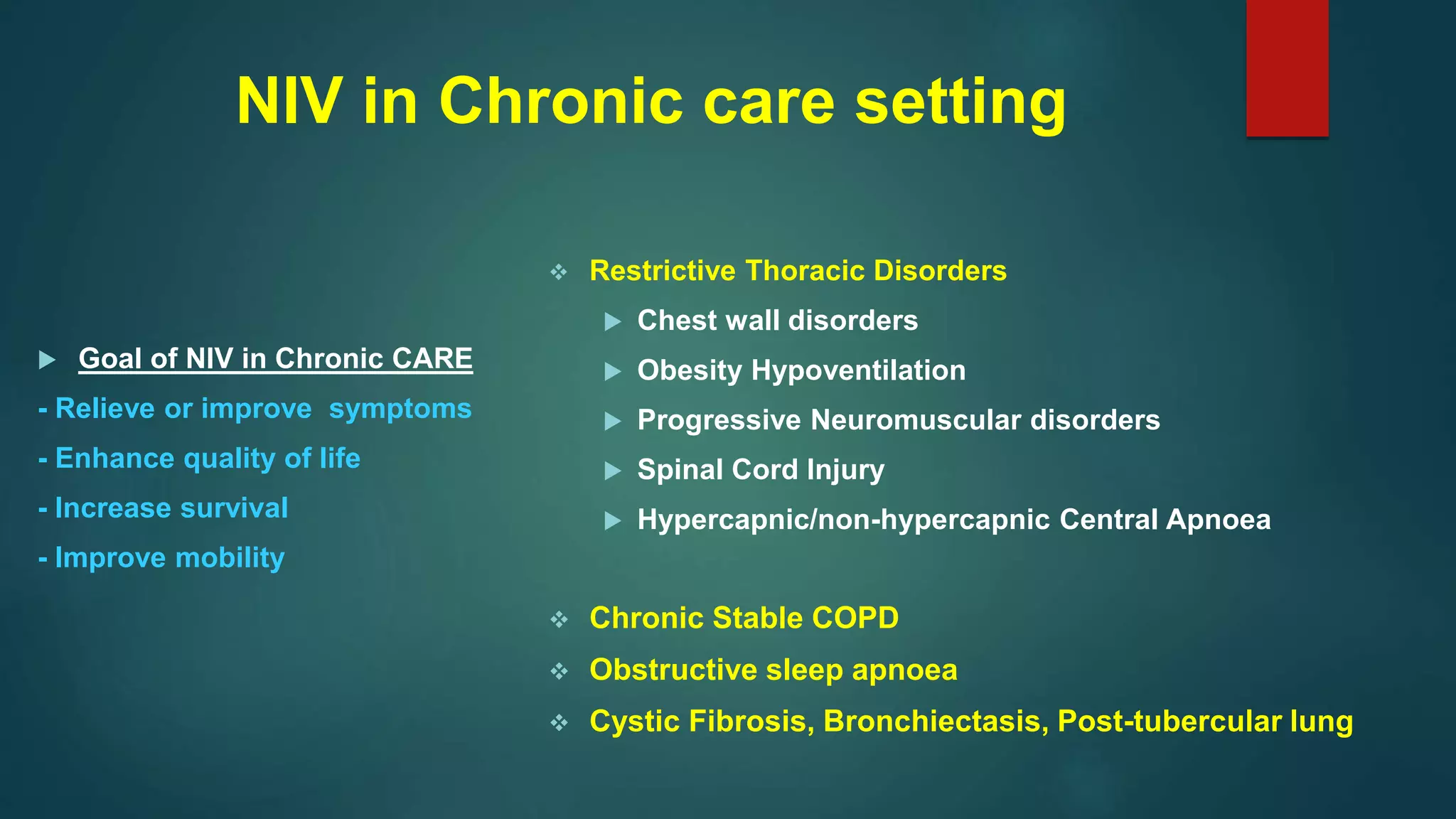
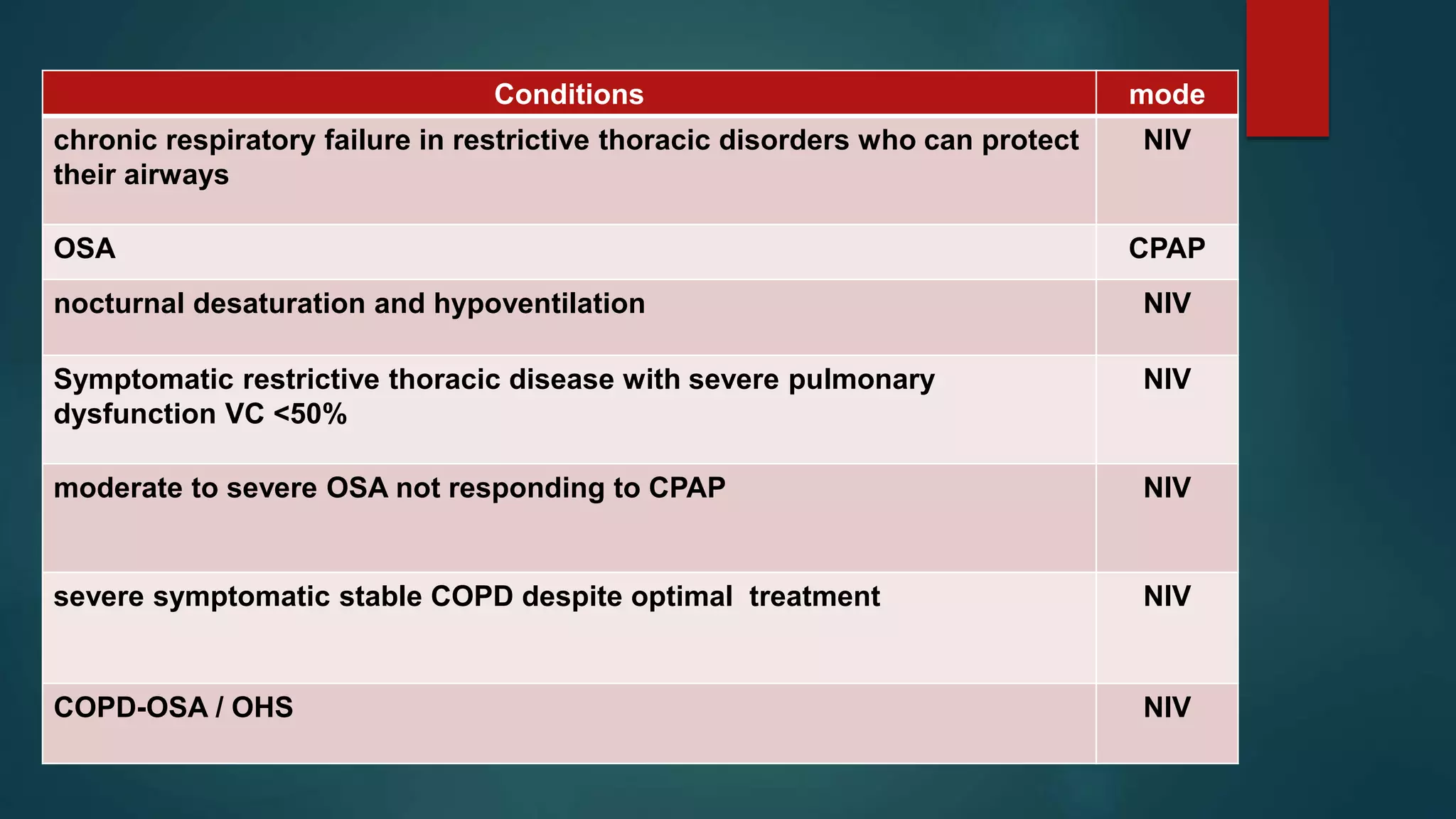
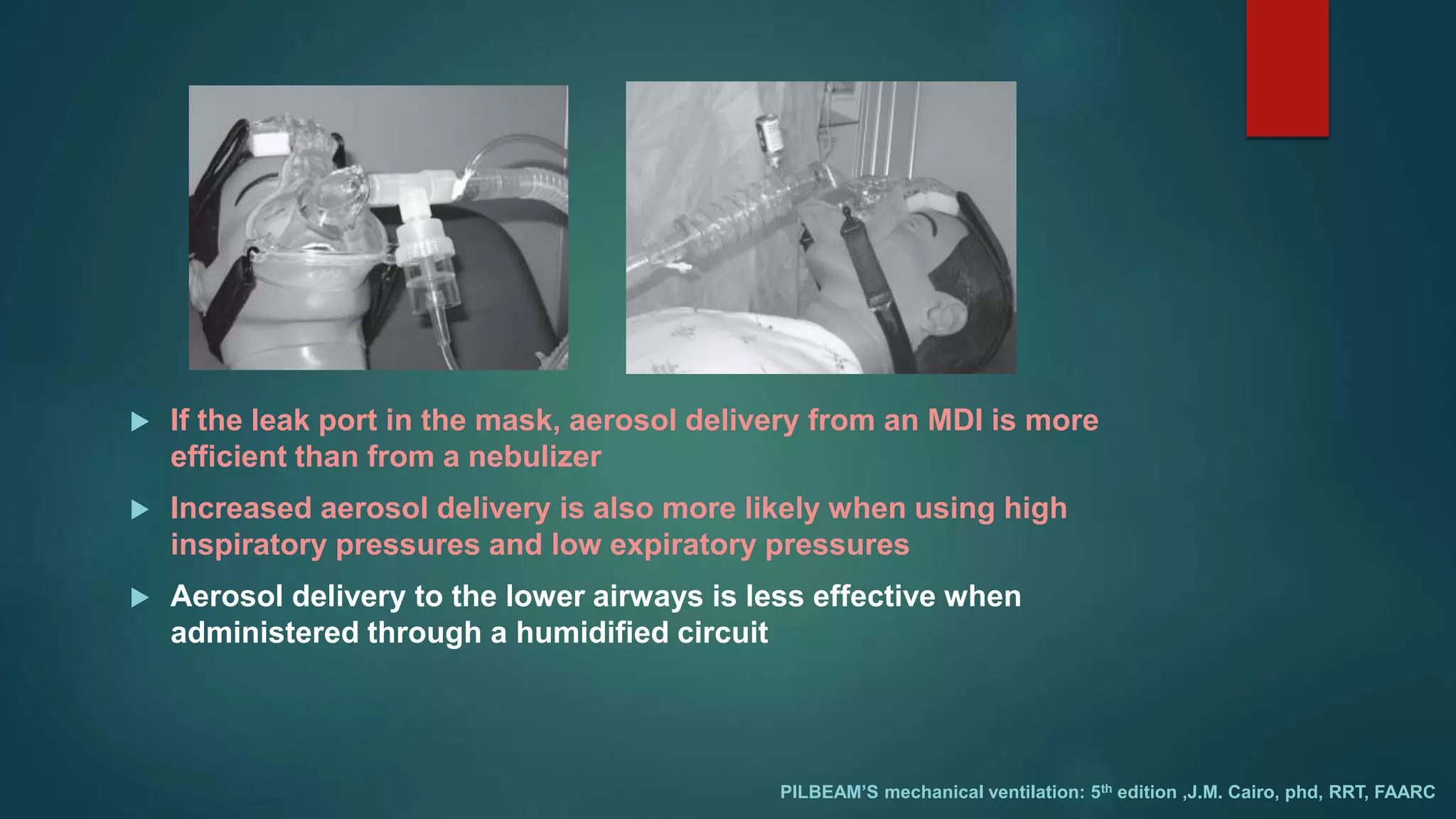
The document outlines various aspects of non-invasive ventilation (NIV) managed by Dr. Chandan Kumar Sheet, covering key topics such as NIV waveforms, interfaces, monitoring, and newer modes of NIV. It provides insights into terminology like positive pressure ventilation and emphasizes the importance of patient comfort, trigger sensitivity, and potential complications associated with NIV use. It also discusses monitoring parameters, weaning strategies, and advancements in NIV techniques for chronic respiratory issues.