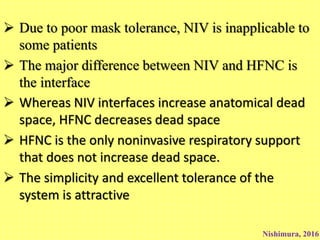
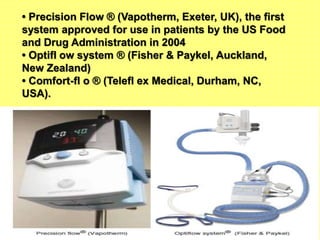
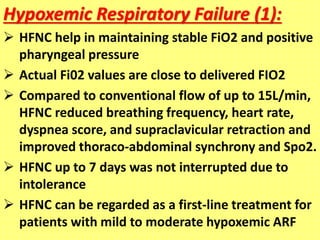
HFNC therapy provides high flow oxygen through a nasal cannula. It has several benefits over traditional oxygen delivery methods, including more accurate oxygen delivery, washout of dead space, and generation of positive end-expiratory pressure. HFNC is a well-tolerated therapy that can be used for hypoxemic respiratory failure, pre-intubation, and post-extubation. While promising, further research is still needed to establish clear guidelines for its use.