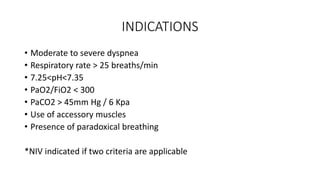
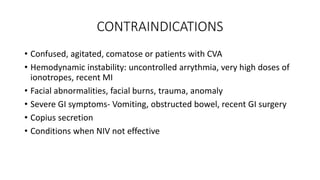
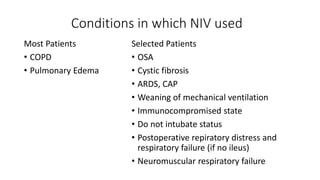
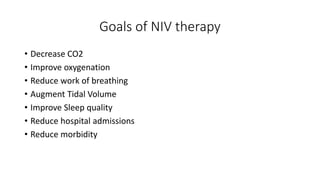
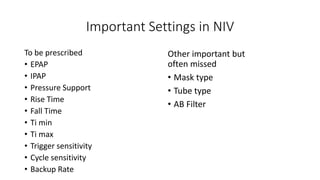
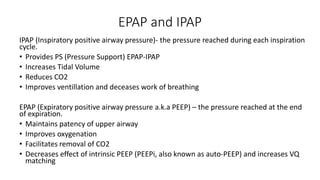
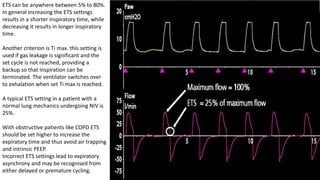
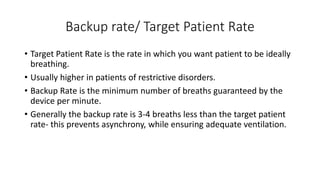
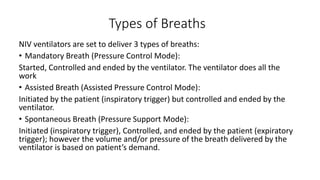
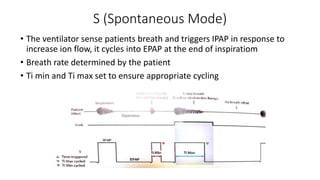
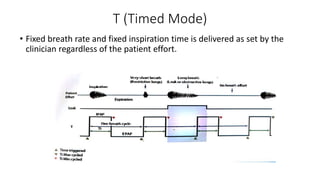
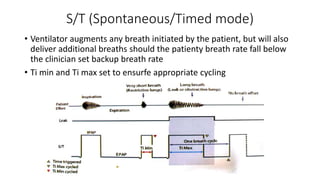
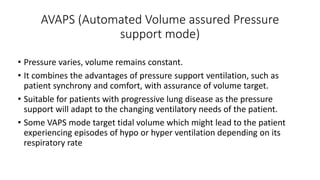
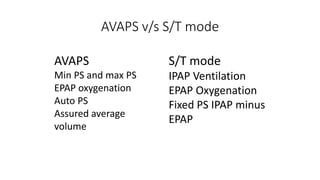
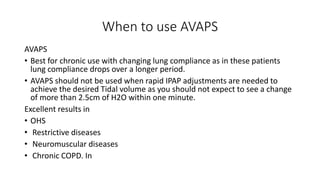
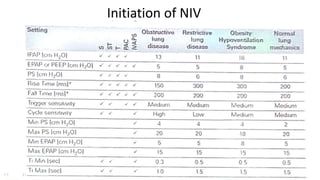
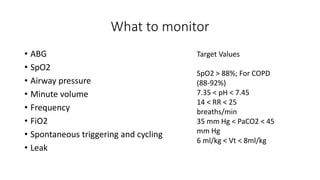
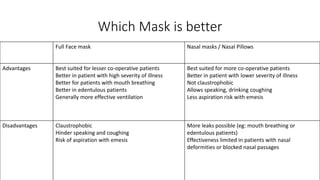
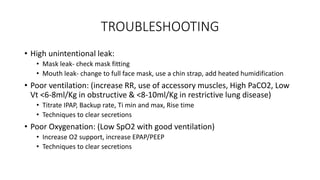
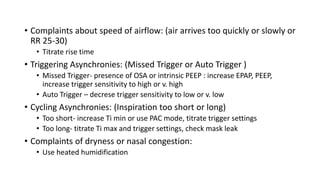
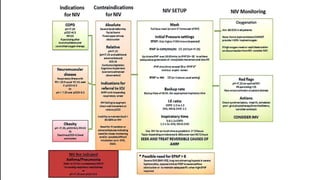
NIV, or non-invasive ventilation, is a form of ventilation therapy that is applied non-invasively through a mask rather than an endotracheal tube. It is commonly used to treat conditions like COPD exacerbations, pulmonary edema, and respiratory failure. Key settings that must be adjusted include IPAP, EPAP, Ti min/max, trigger sensitivity, and backup rate. Modes include spontaneous, timed, and bi-level positive airway pressure. Proper mask fitting and troubleshooting issues like leaks are important for ensuring effective ventilation. Regular monitoring of parameters like ABGs, SpO2, and ventilation is needed to optimize NIV therapy.