1. Non-invasive ventilation (NIV) delivers ventilatory support without the need for an invasive airway. It has been increasingly used since the 1980s with the development of positive pressure ventilation delivered by masks.
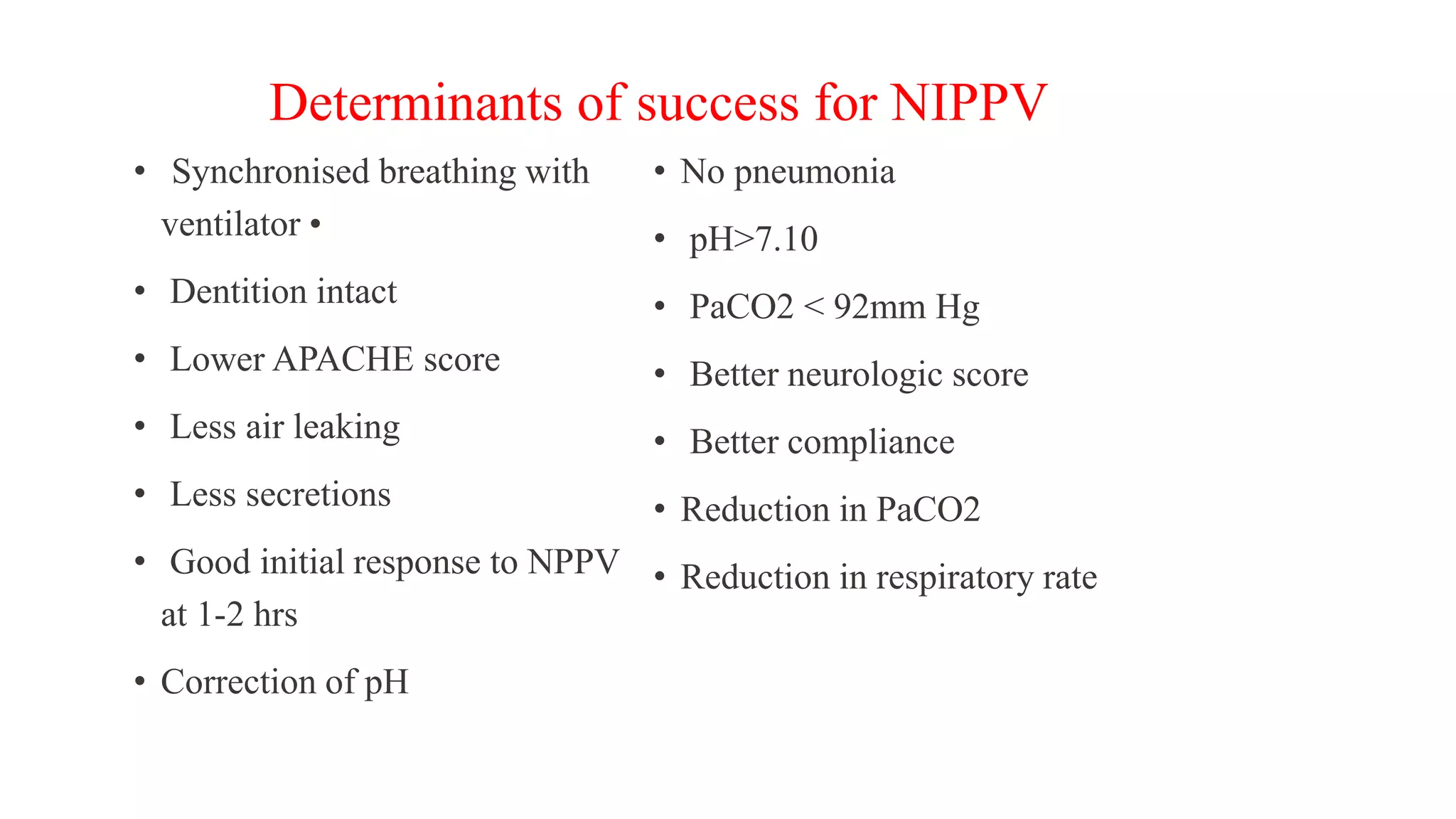
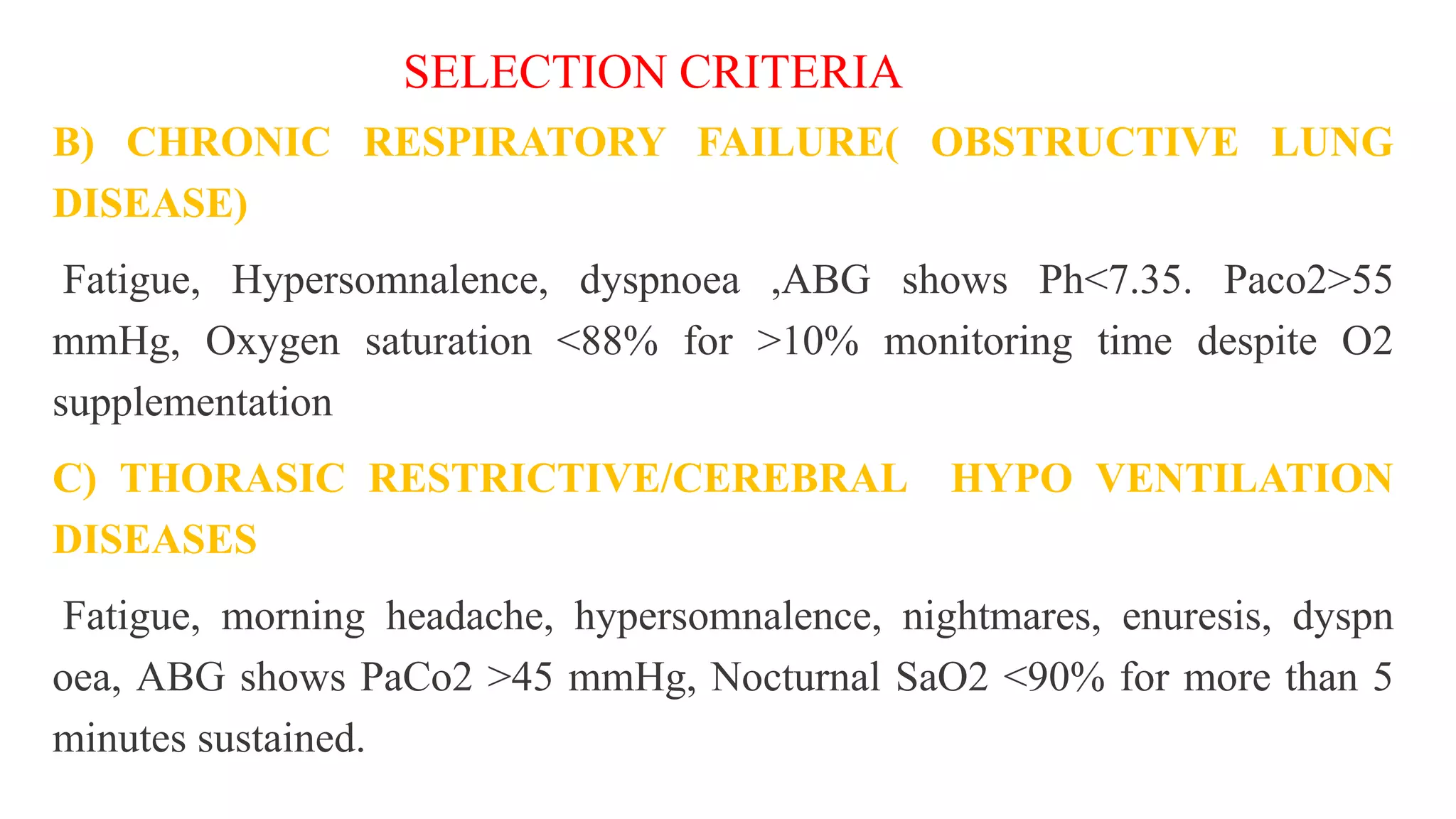
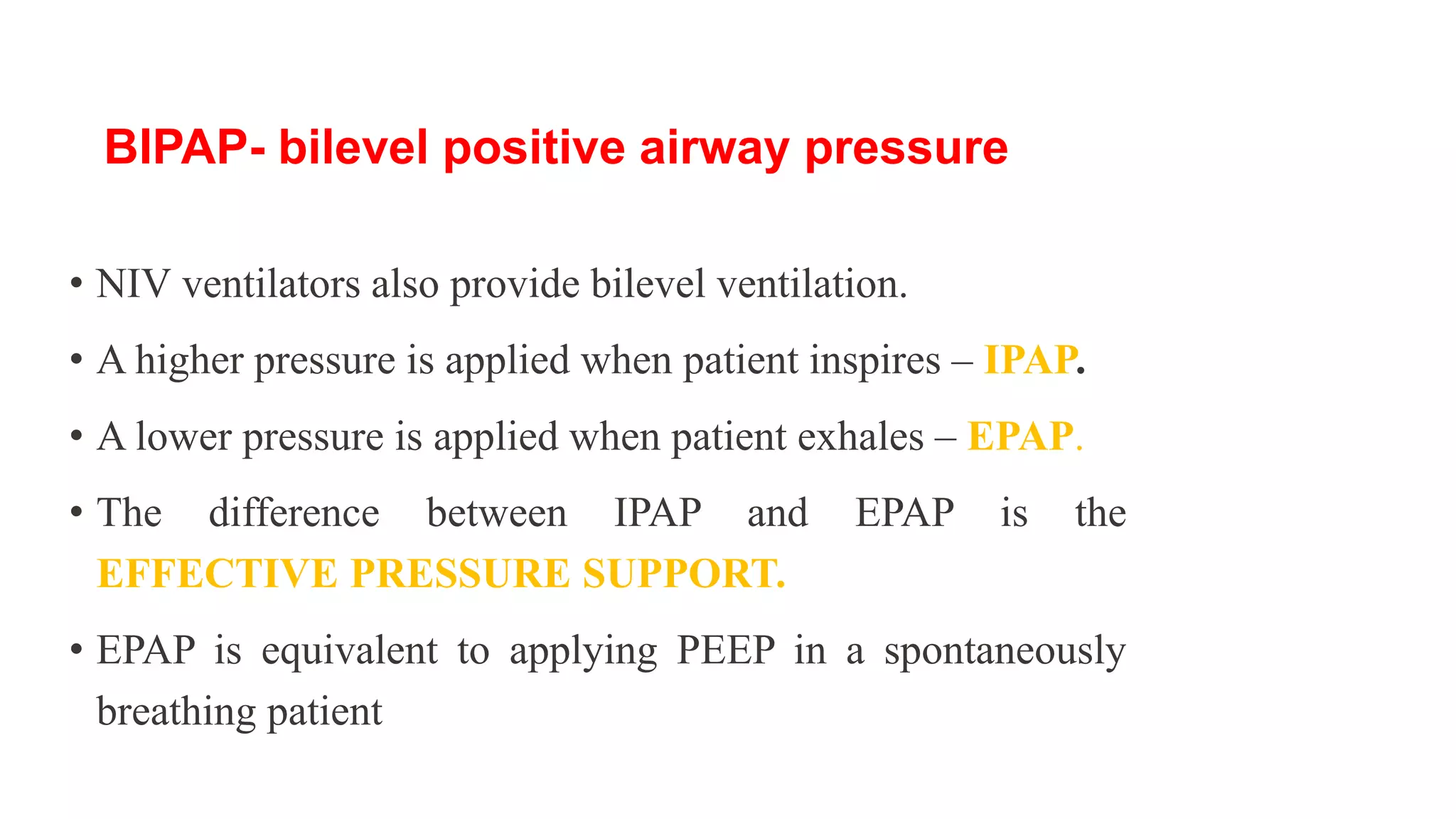
2. NIV can be delivered via nasal or facial masks connected to ventilators. It works by partially unloading the respiratory muscles and improving oxygenation. Common indications include acute or chronic respiratory failure.
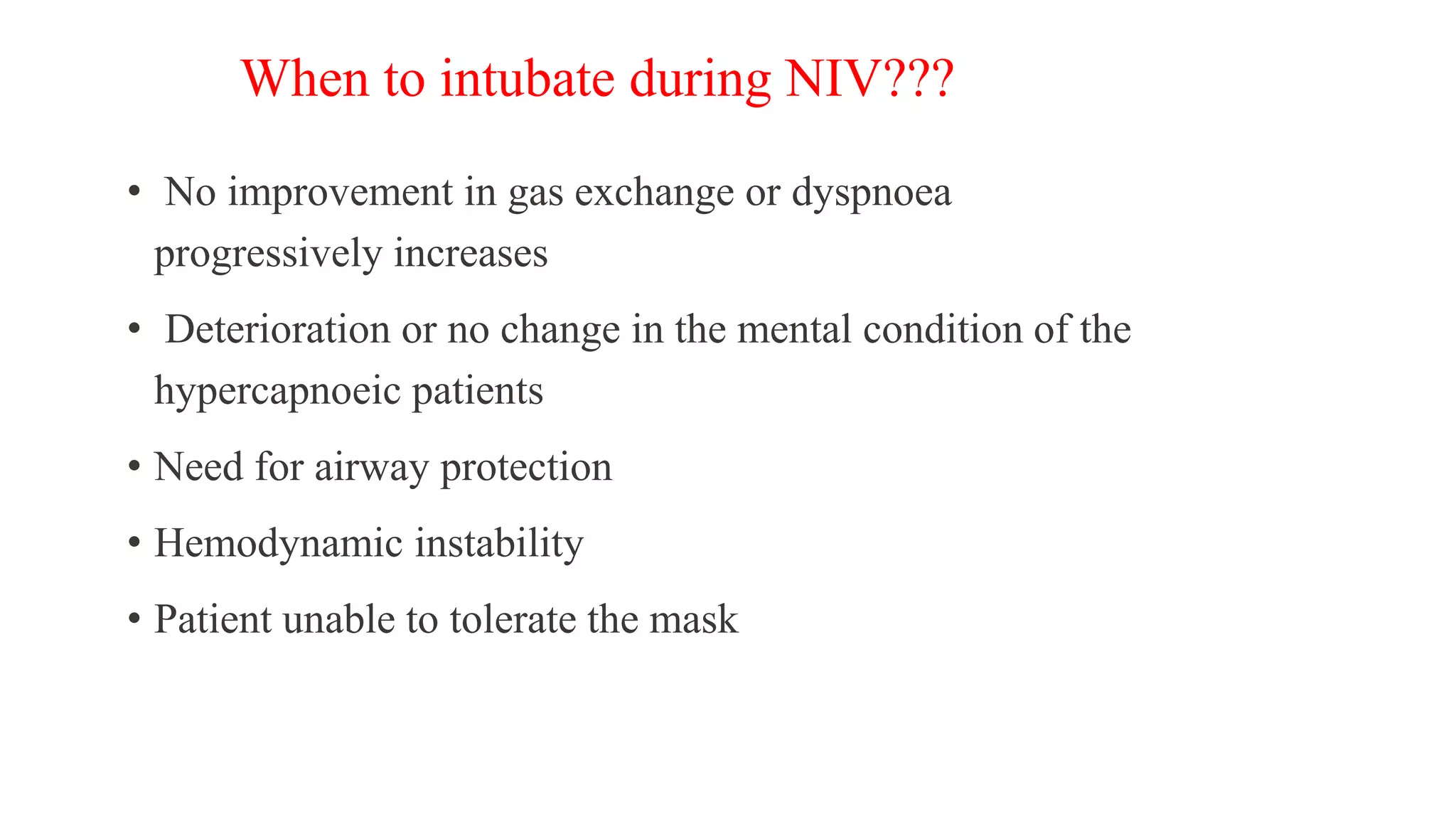
3. The main advantages of NIV are avoiding complications of invasive ventilation while preserving airway defenses and patient comfort. However, NIV may not be suitable for severely ill patients and improper fitting of masks can cause skin damage or air leaks. Patient monitoring is important to assess response and determine