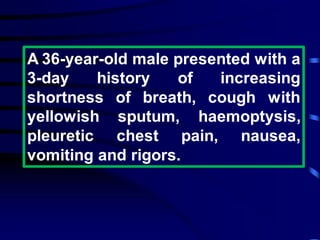
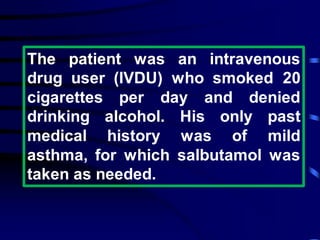
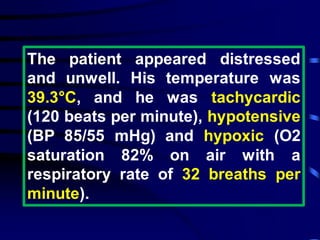
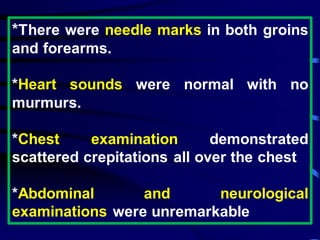
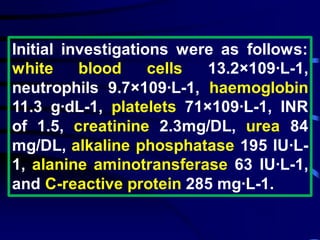
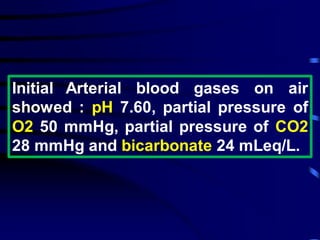
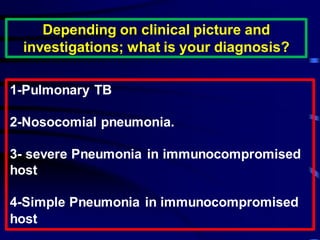
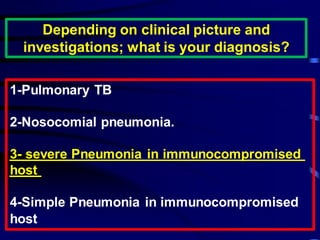
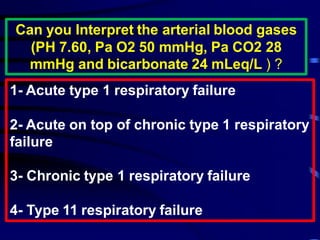
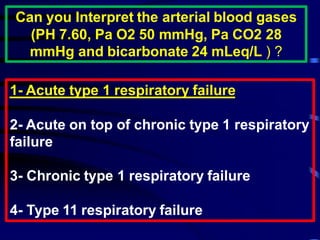
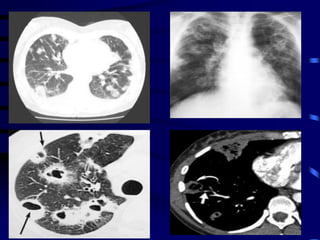
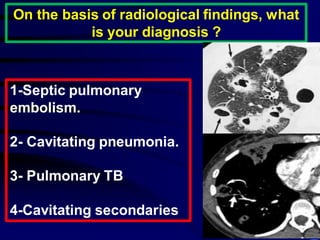
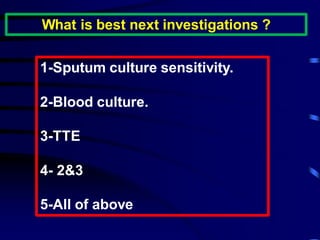
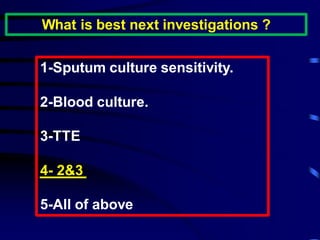
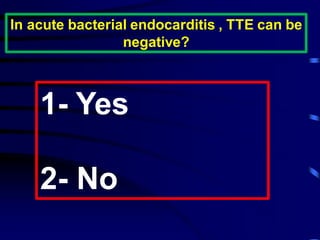
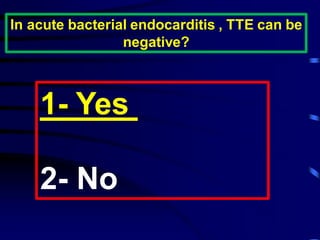
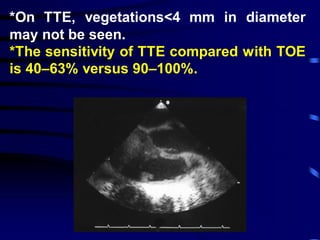
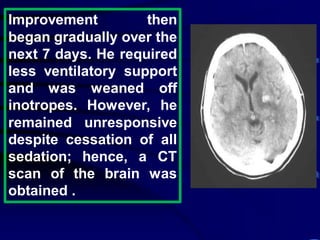
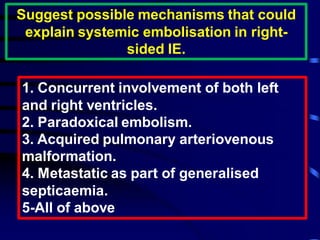
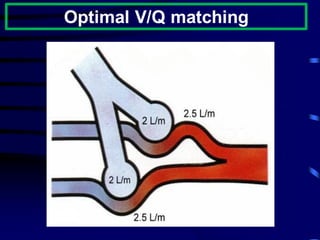
This document describes a case presentation of a 36-year-old male intravenous drug user who presented with shortness of breath, cough, hemoptysis and other symptoms. Clinical exams and tests revealed pneumonia, hypotension and hypoxia. Imaging showed septic pulmonary emboli and infective endocarditis was suspected. Blood cultures grew Staphylococcus aureus. Despite treatment, the patient deteriorated and developed complications including respiratory failure. After several weeks of intensive care, the patient gradually recovered consciousnesss and mobility over several months.