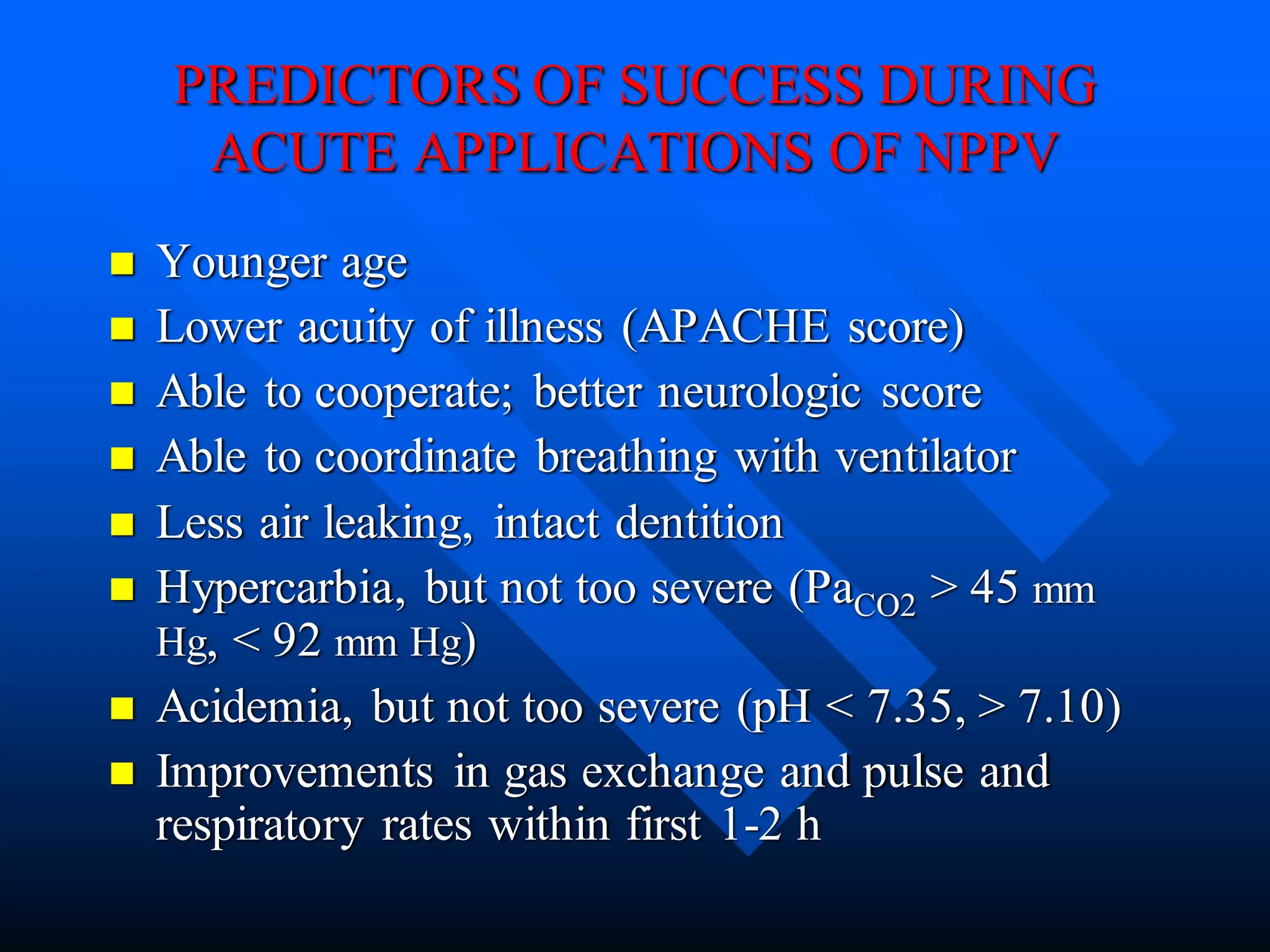
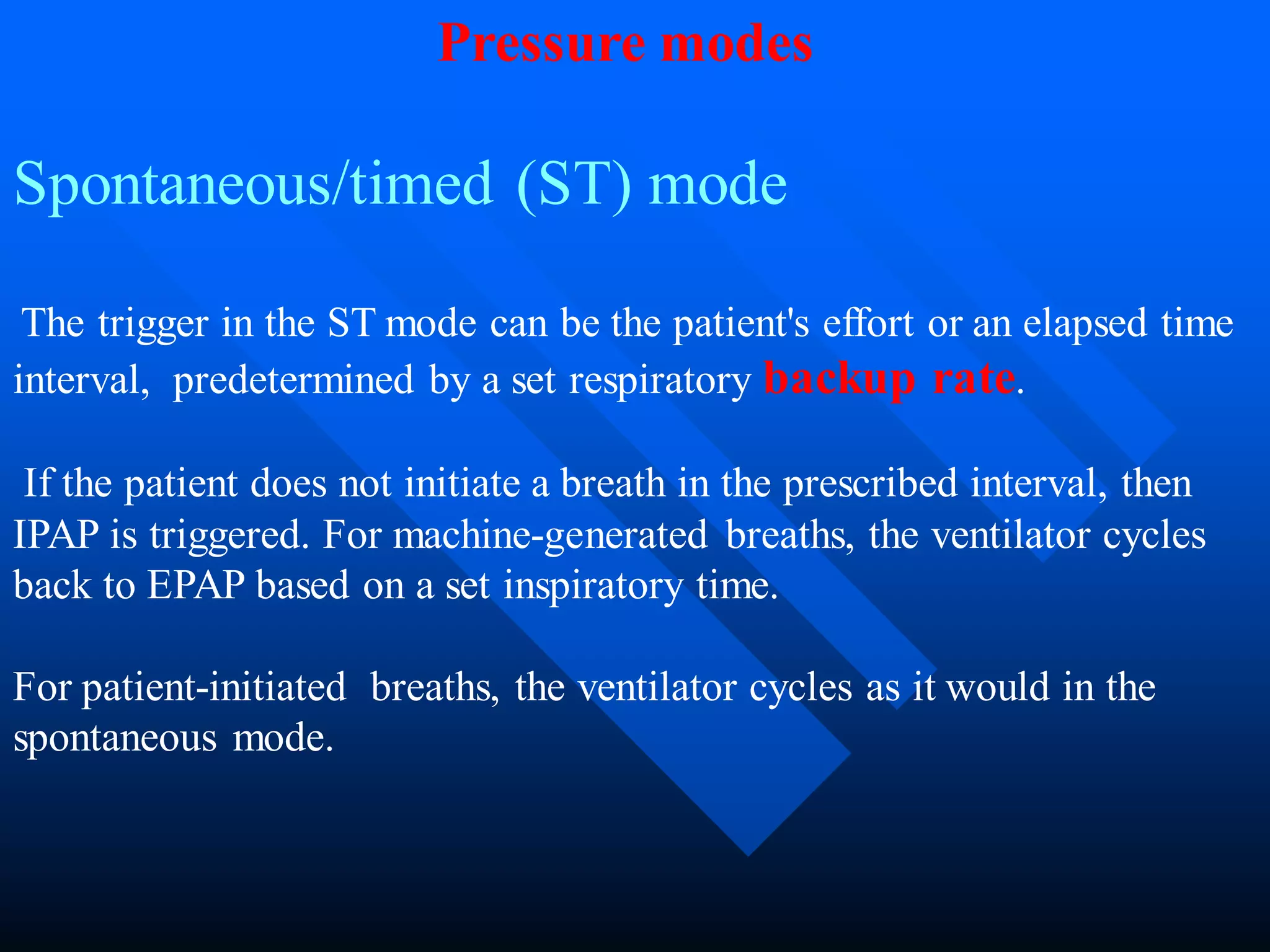
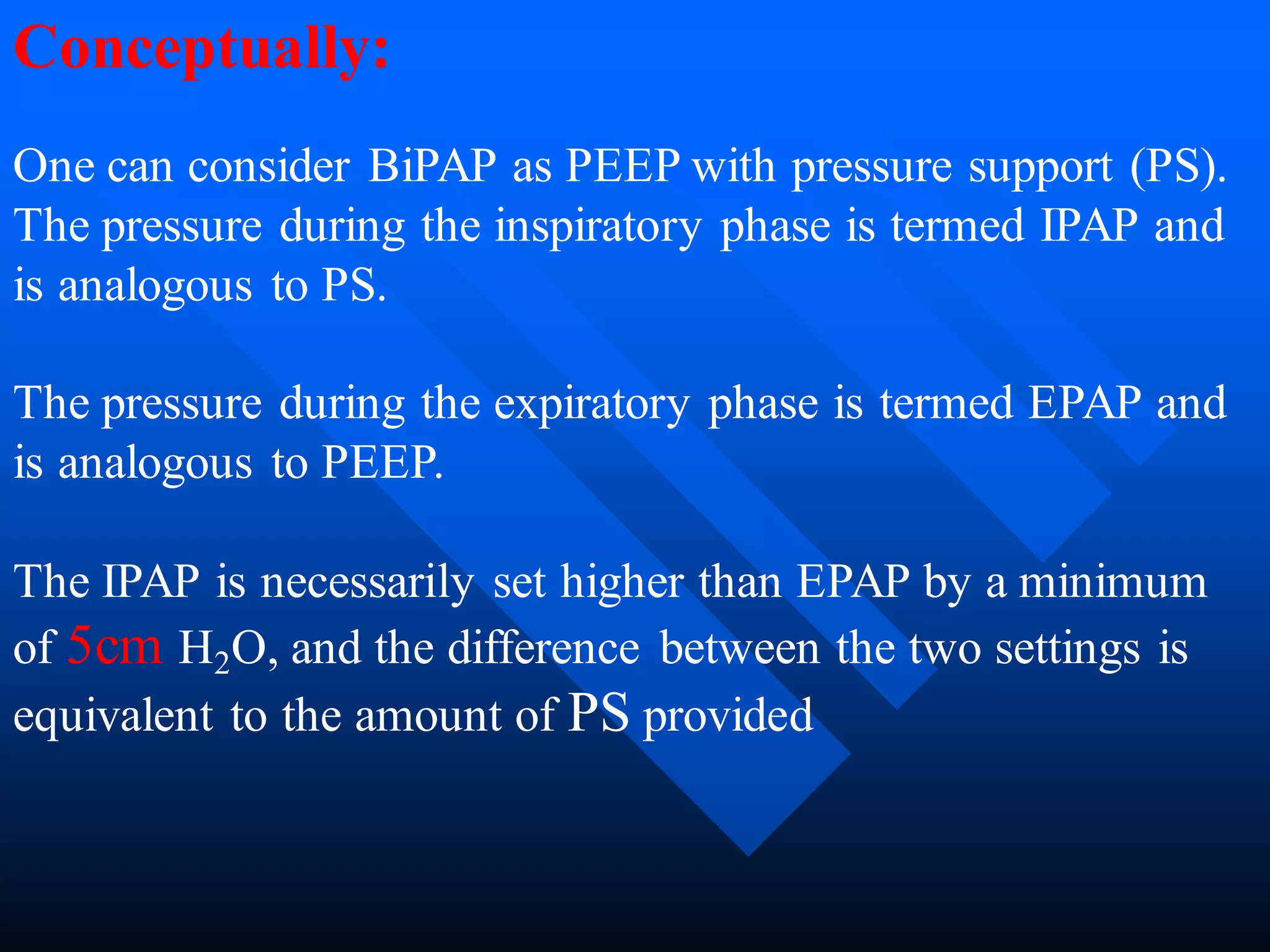
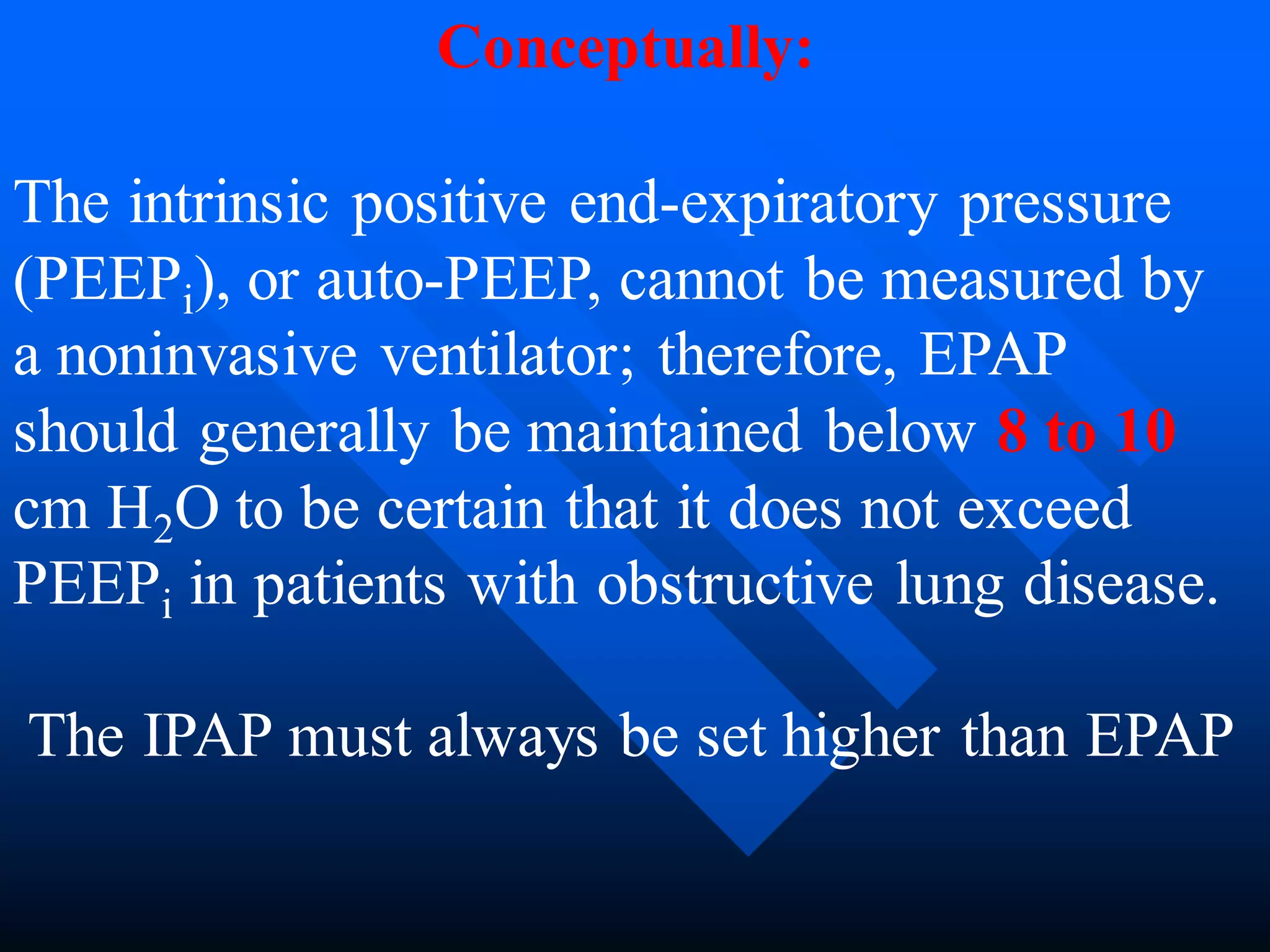
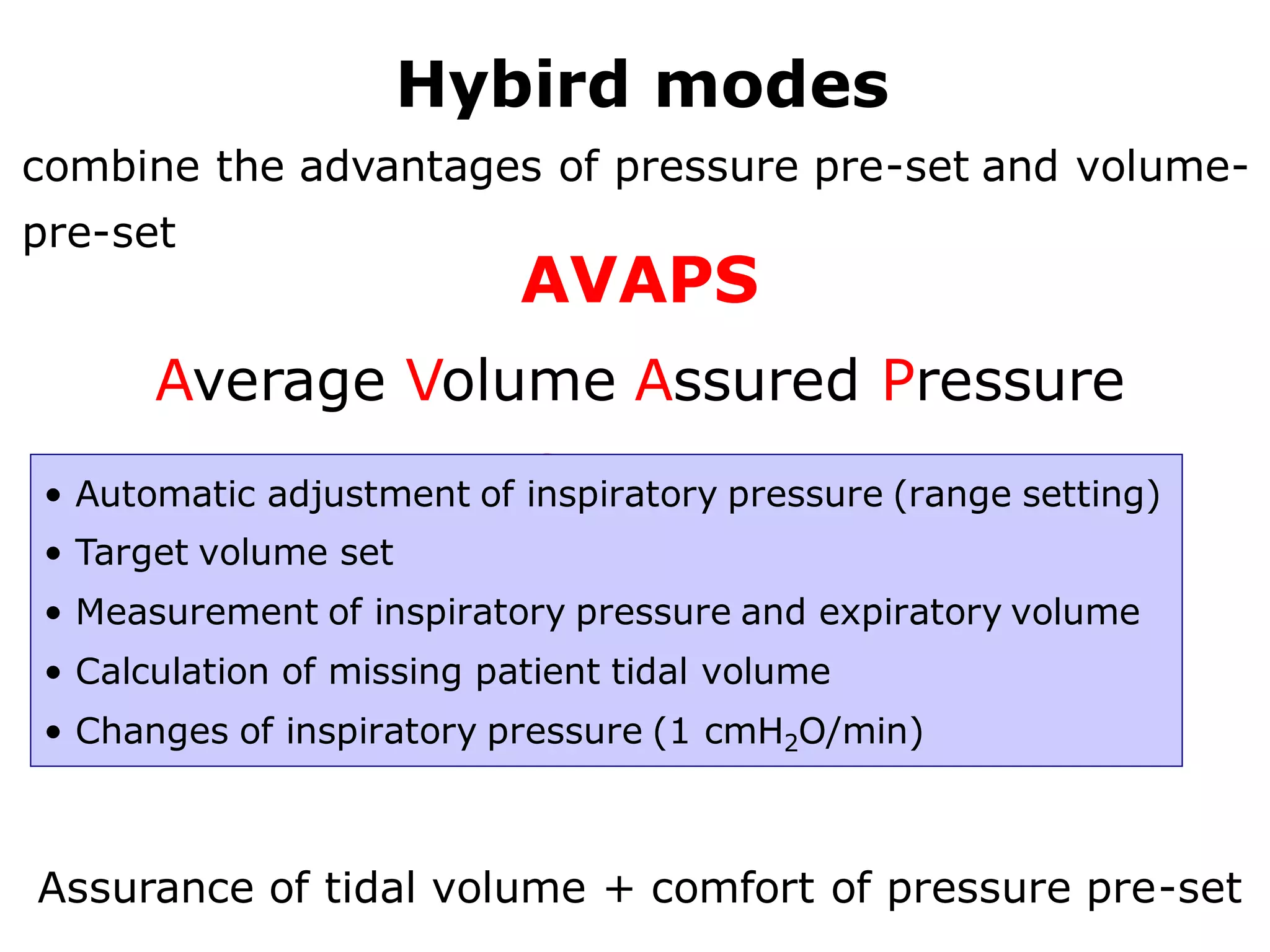
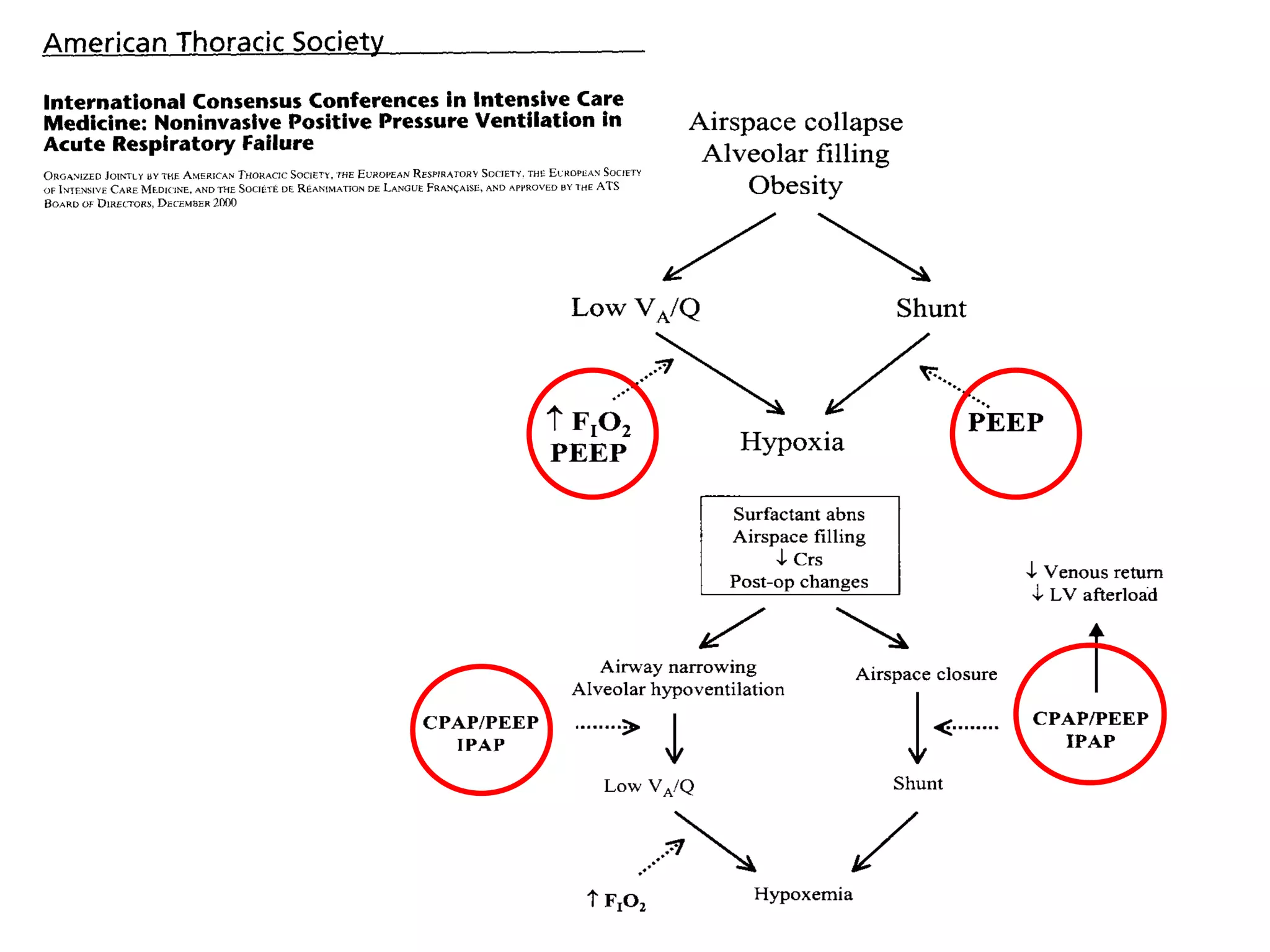
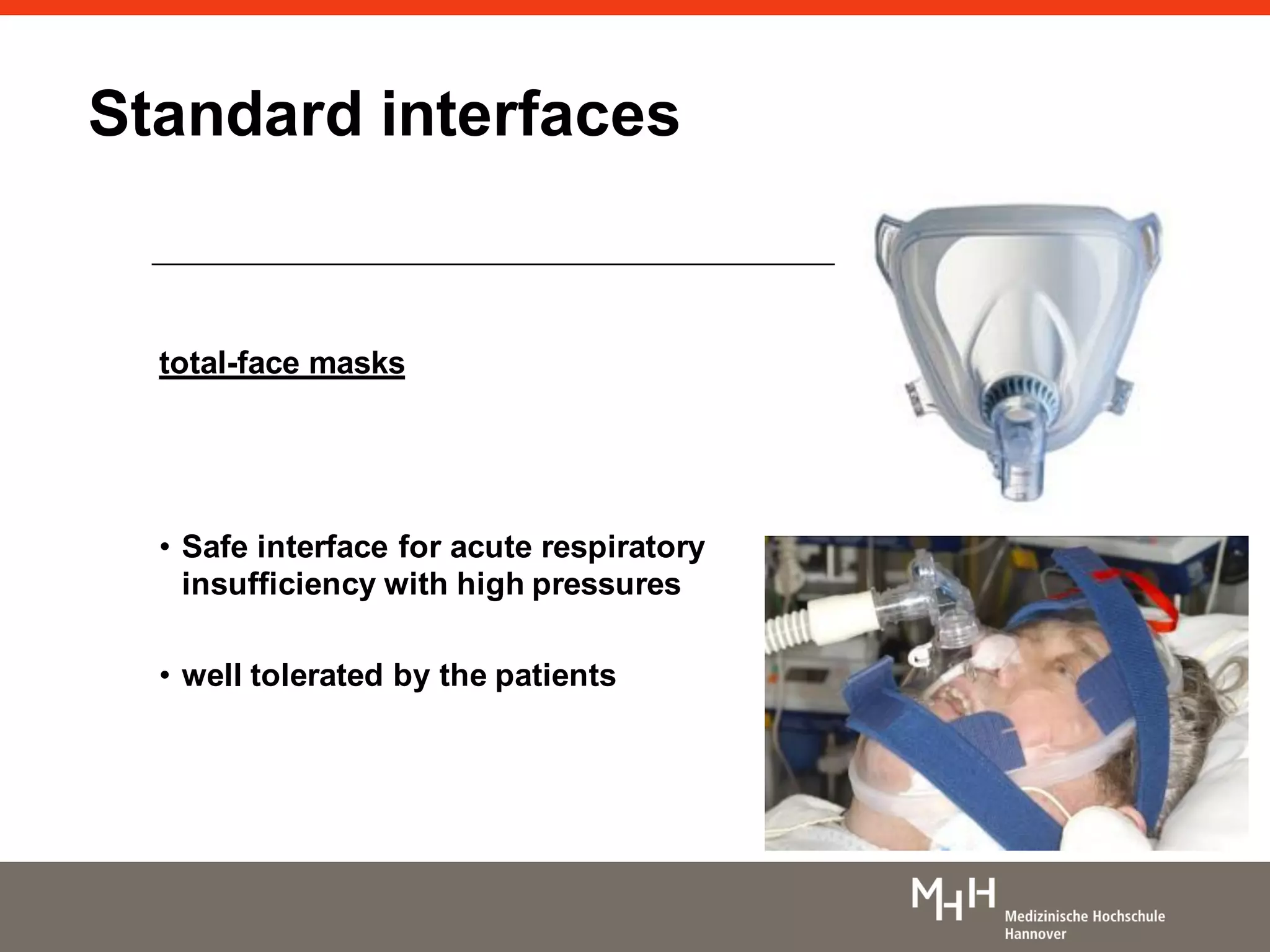
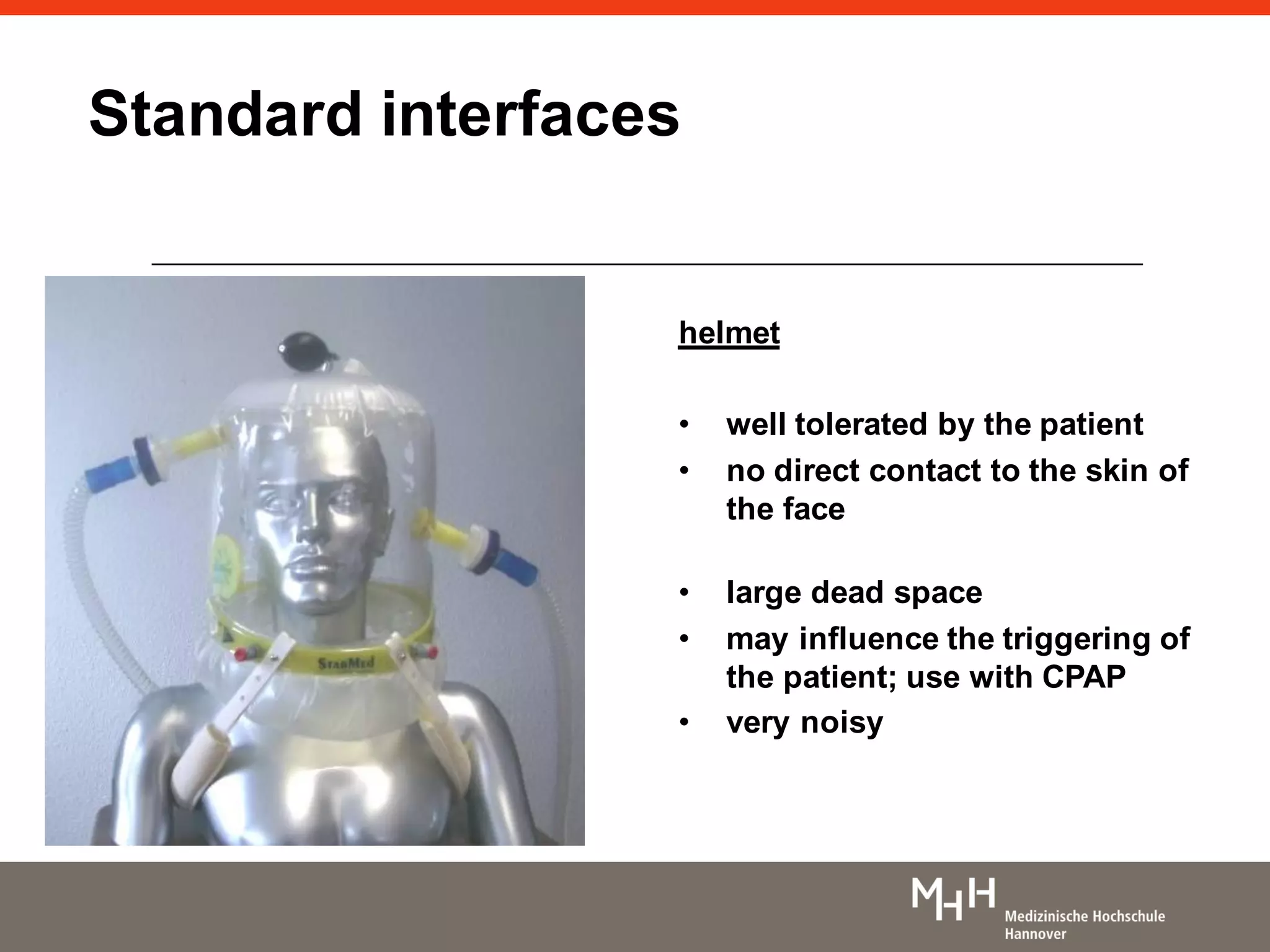
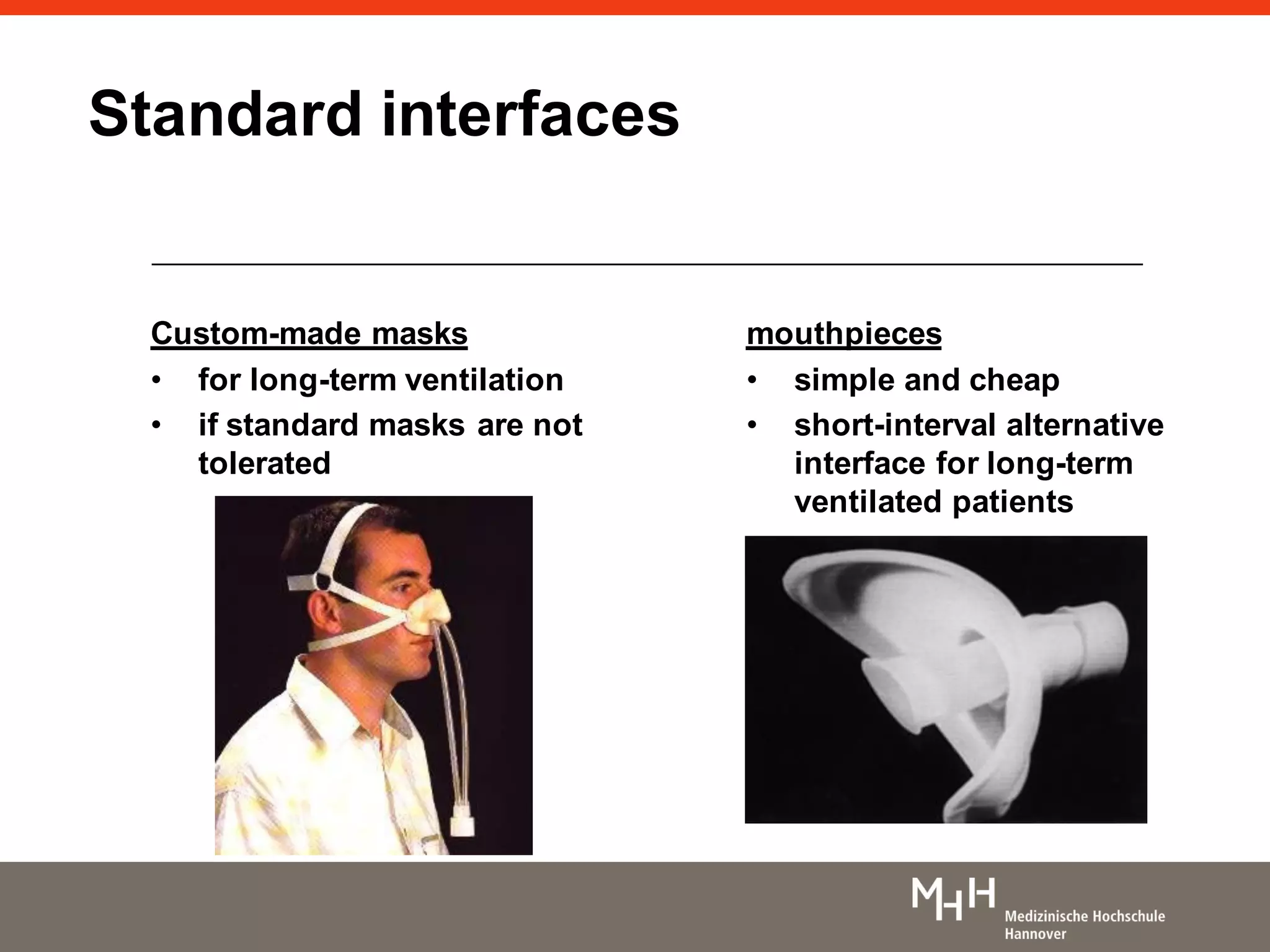
This document discusses non-invasive positive pressure ventilation (NIPPV). It defines NIPPV as ventilation without an invasive airway and notes its increasing use for acute respiratory failure. The document covers the history of NIPPV, indications, goals, advantages, patient selection criteria, initiation procedures, modes (including CPAP, BiPAP, volume vs pressure), and settings. NIPPV can effectively treat various conditions like COPD, heart failure, and respiratory infections while avoiding intubation. Careful patient selection and monitoring are important for successful NIPPV.