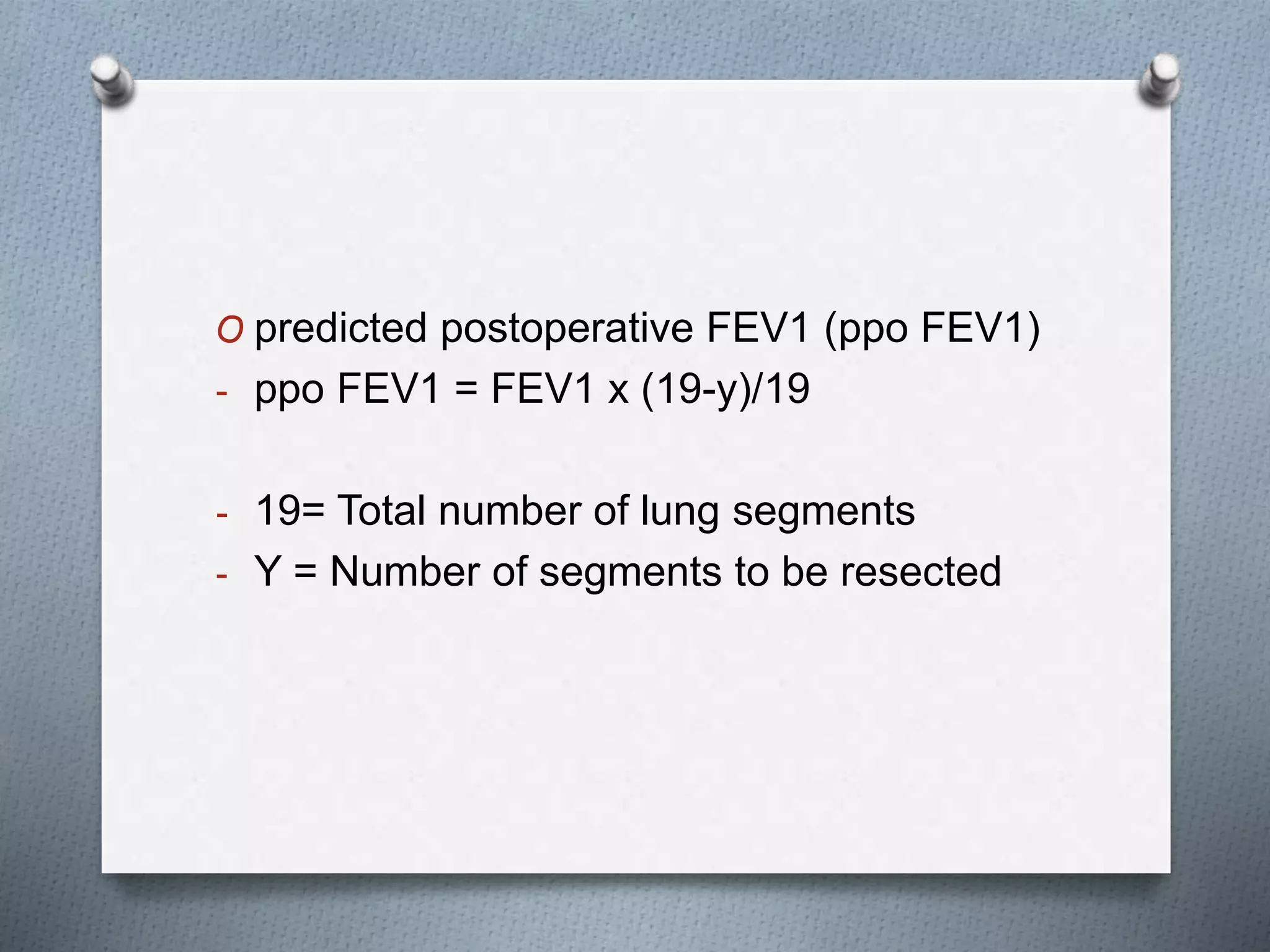
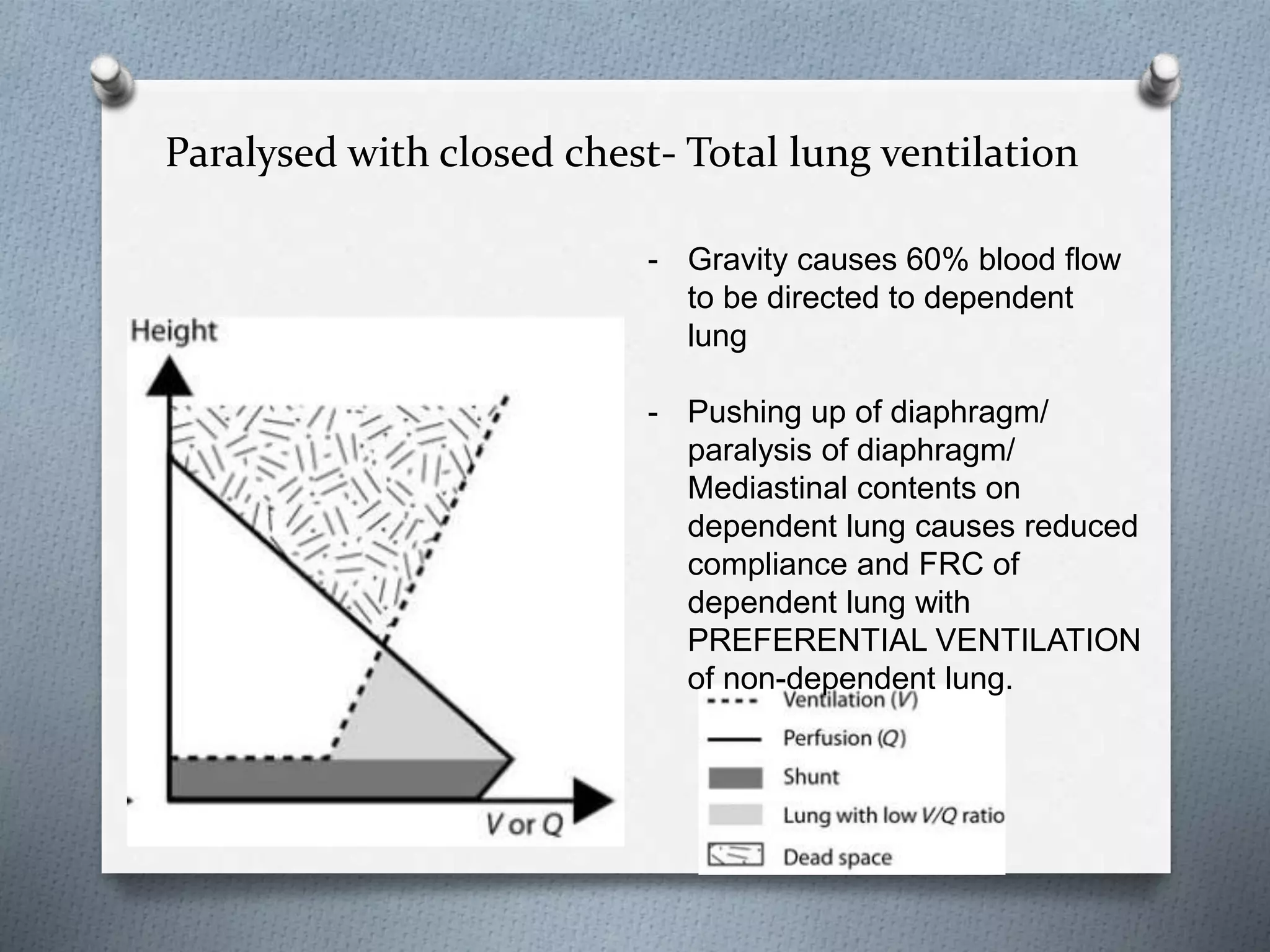
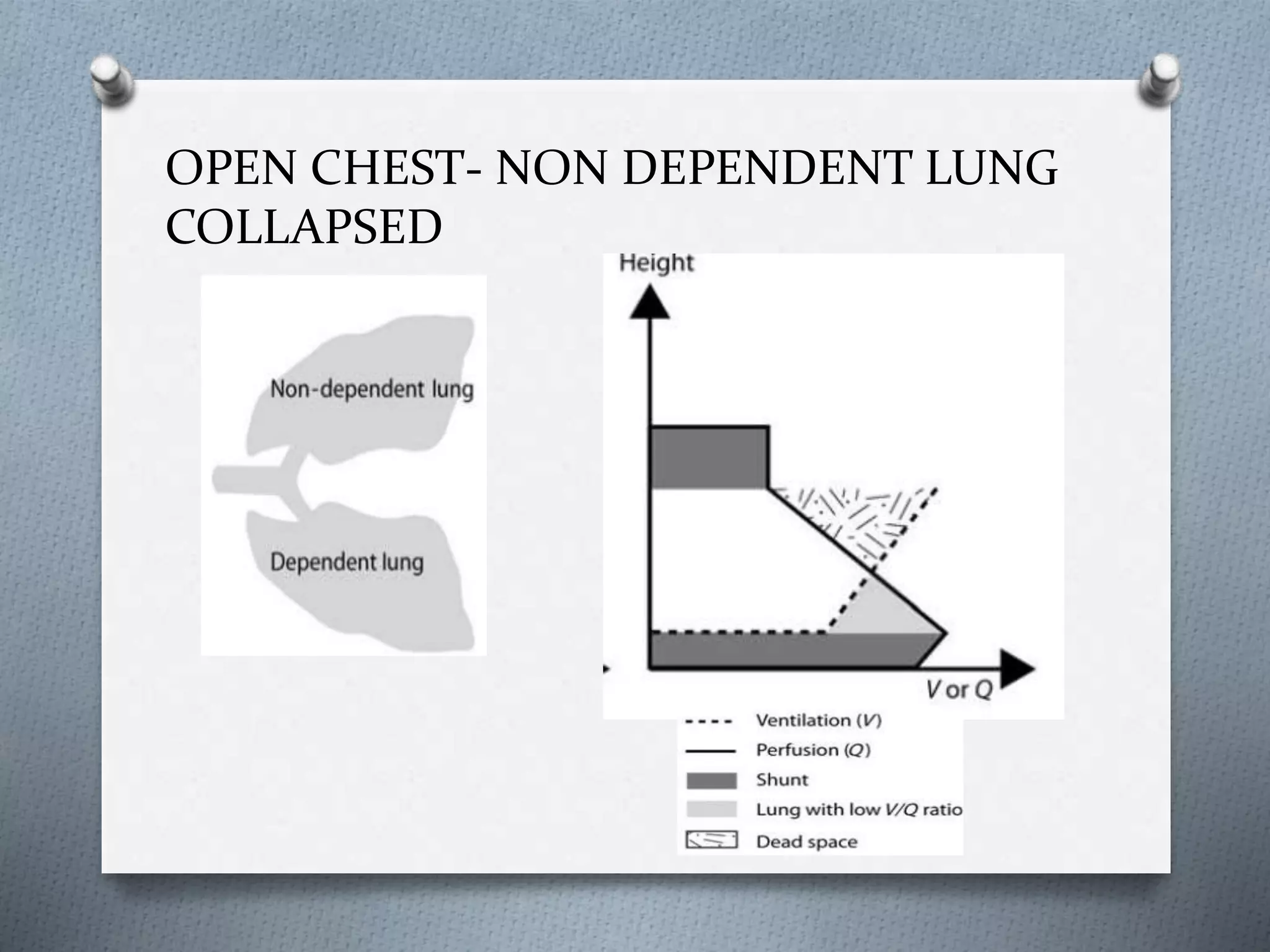
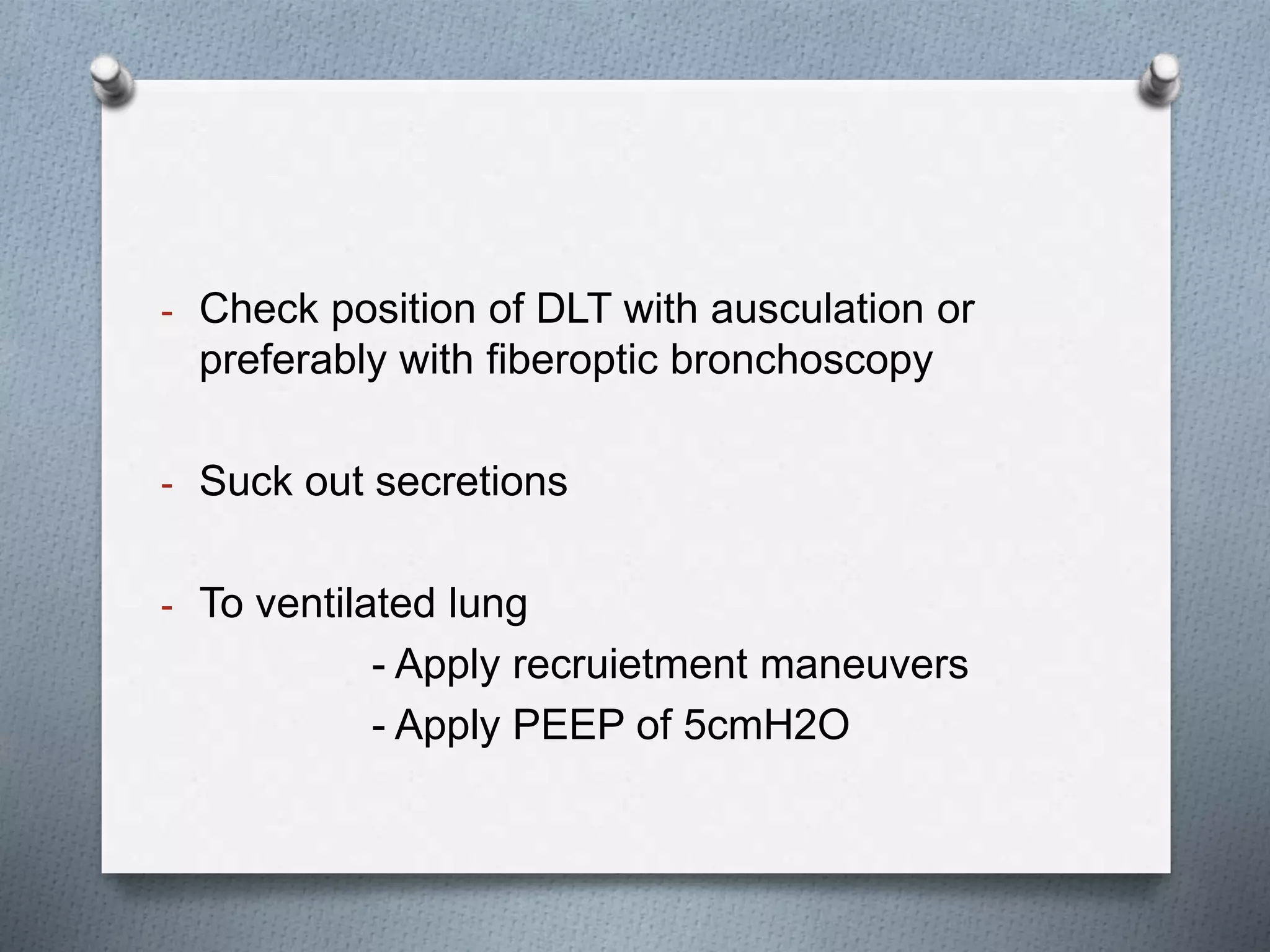
One Lung Ventilation (OLV) is a technique that isolates ventilation to one lung during surgery using double lumen tubes (DLTs) or bronchial blockers. DLTs allow control of ventilation to each lung and switching between single and dual lung ventilation. Placement is confirmed with fiberoptic bronchoscopy. OLV reduces the risk of cross contamination during certain procedures. Preoperative pulmonary function tests assess risk, with an FEV1 <40% or DLCO <40% indicating high risk. During OLV, hypoxic pulmonary vasoconstriction and gravity divert blood flow away from the non-ventilated lung to reduce shunting. Anesthesia aims to maintain cardiovascular stability and minimize inhibition of hypo