Recent Advances in NIV
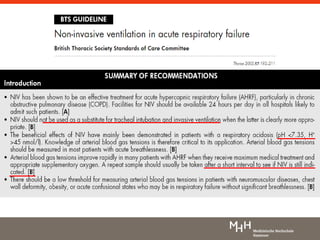
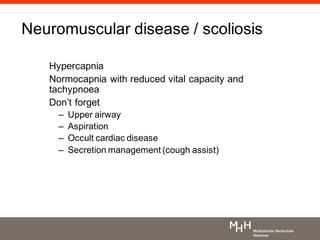
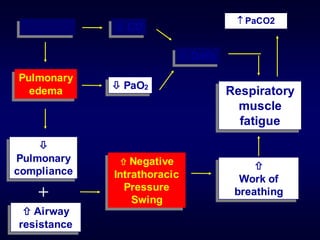
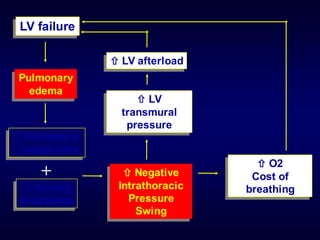
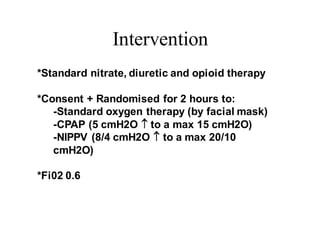
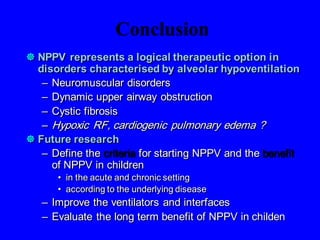
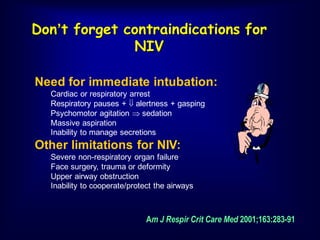
1) Non-invasive positive pressure ventilation (NIPPV) can effectively treat acute respiratory failure without the need for intubation in conditions like COPD, obesity, and neuromuscular diseases.
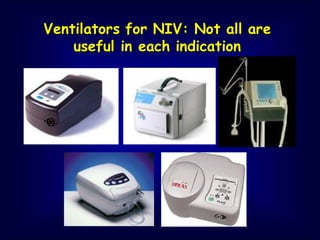
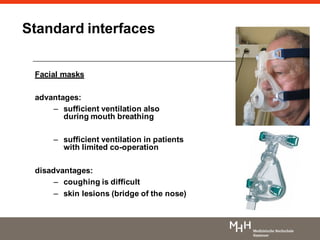
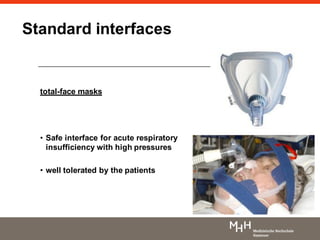
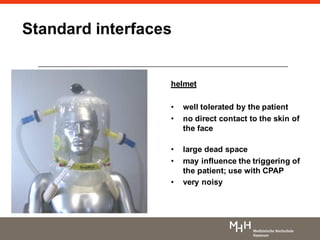
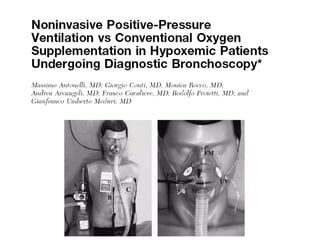
2) Different interfaces like facial masks, nasal masks, and helmets can be used for NIPPV, with nasal masks generally better tolerated than other options.
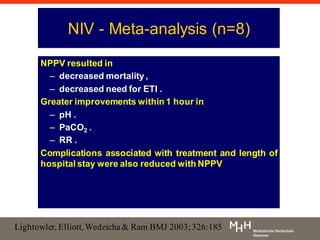
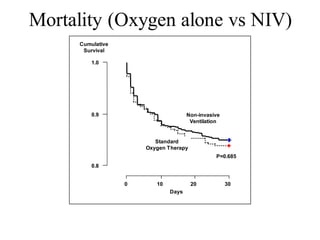
3) NIPPV reduces mortality and need for intubation compared to standard oxygen therapy alone in acute exacerbations of COPD and cardiogenic pulmonary edema.
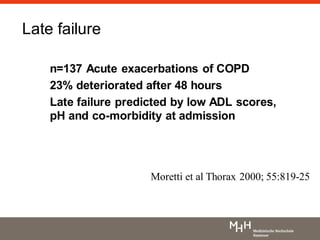
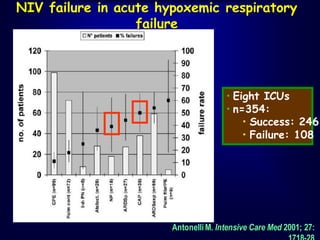
4) Factors like pH, comorbidities, respiratory rate and effort predict success or failure of NIPPV. Close monitoring is needed in cases with higher