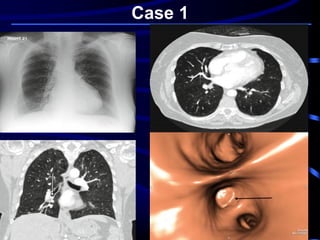
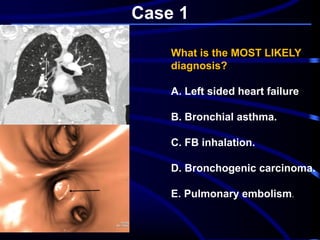
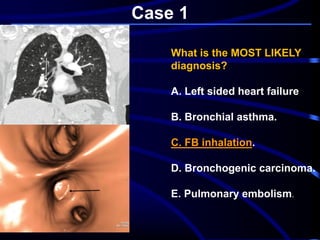
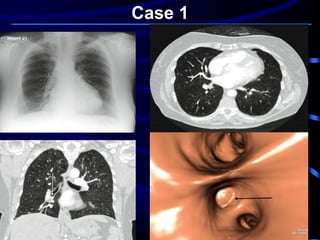
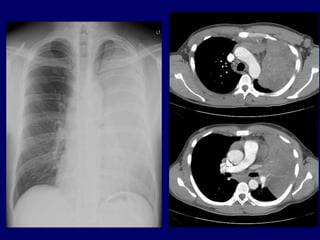
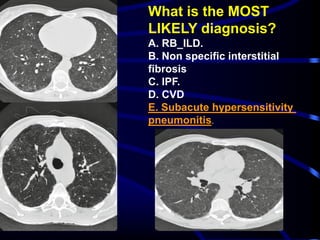
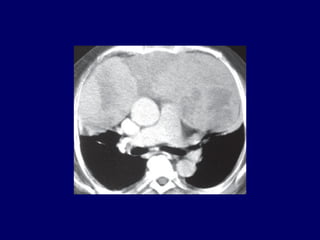
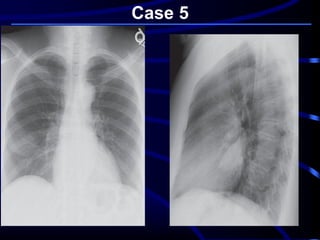
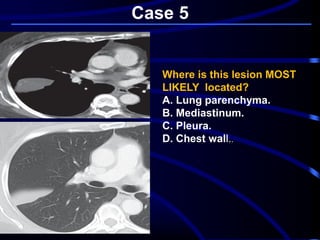
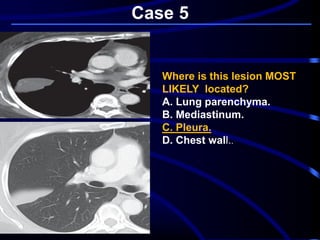
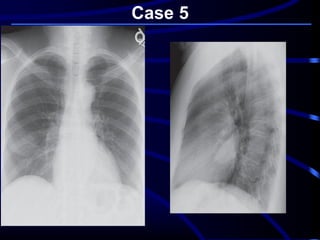
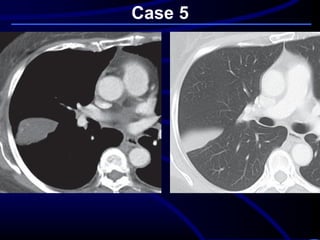
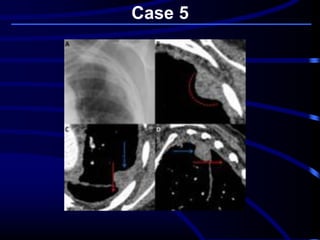
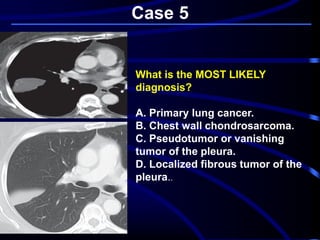
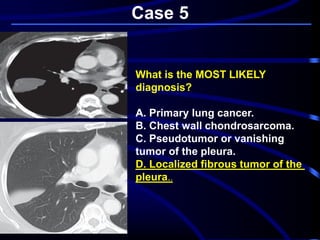
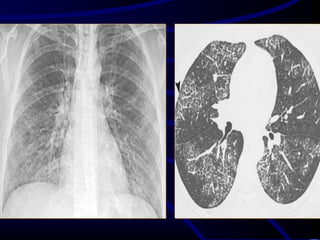
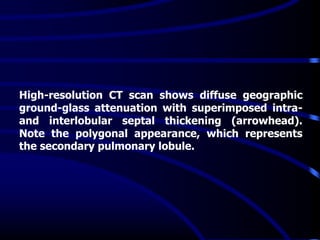
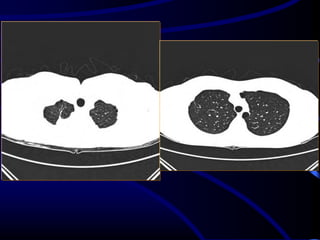
An 81-year-old woman presented with shortness of breath. She had a history of asthma as a child and cardiac bypass surgery 5 years prior. Blood tests were unremarkable. A chest X-ray and CT scan were performed. An X-ray followed by CT scan of a 81-year-old woman with recent onset shortness of breath, history of asthma and cardiac surgery, and normal blood tests showed no concerning findings, making pulmonary embolism the most likely diagnosis.