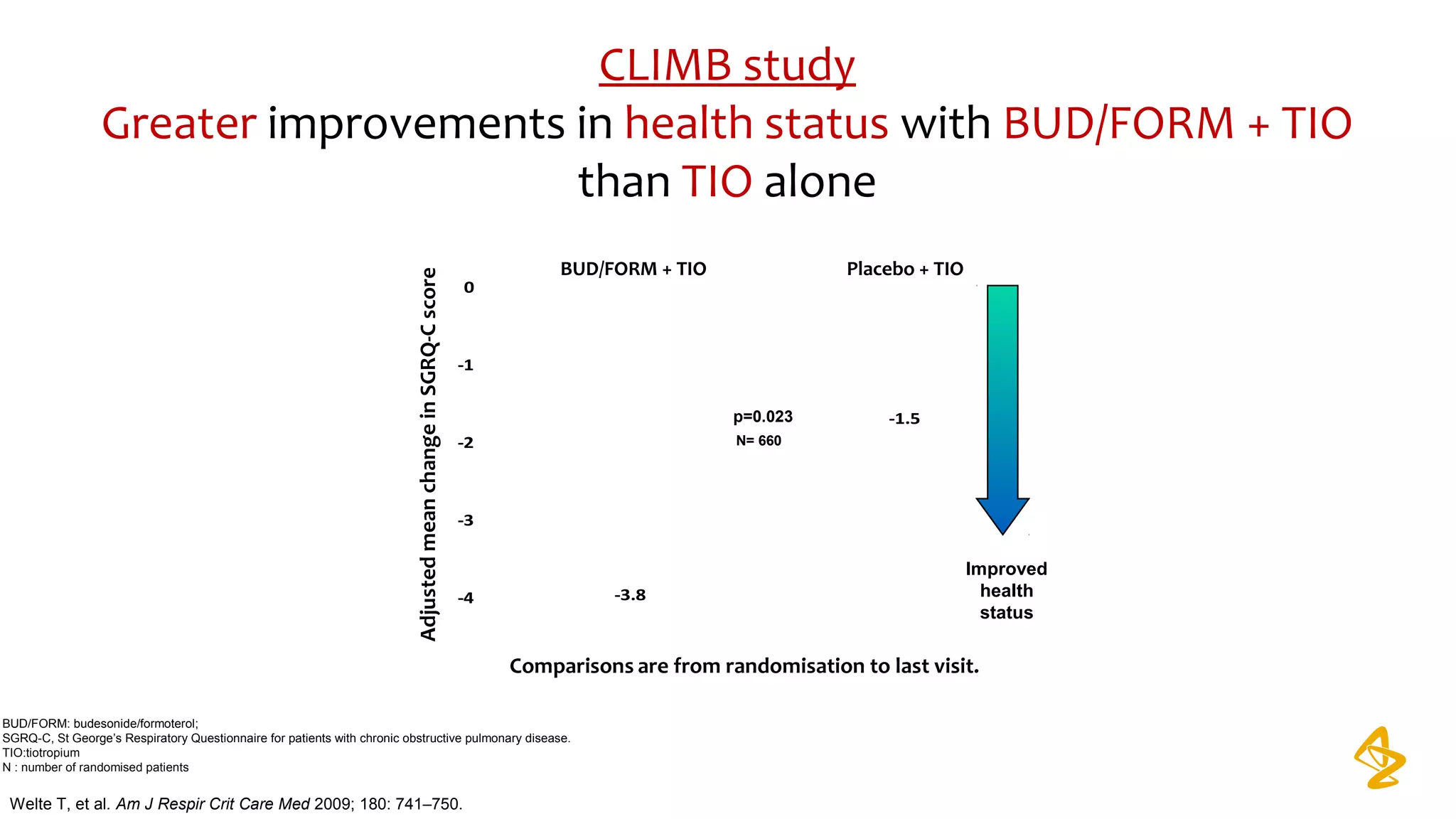
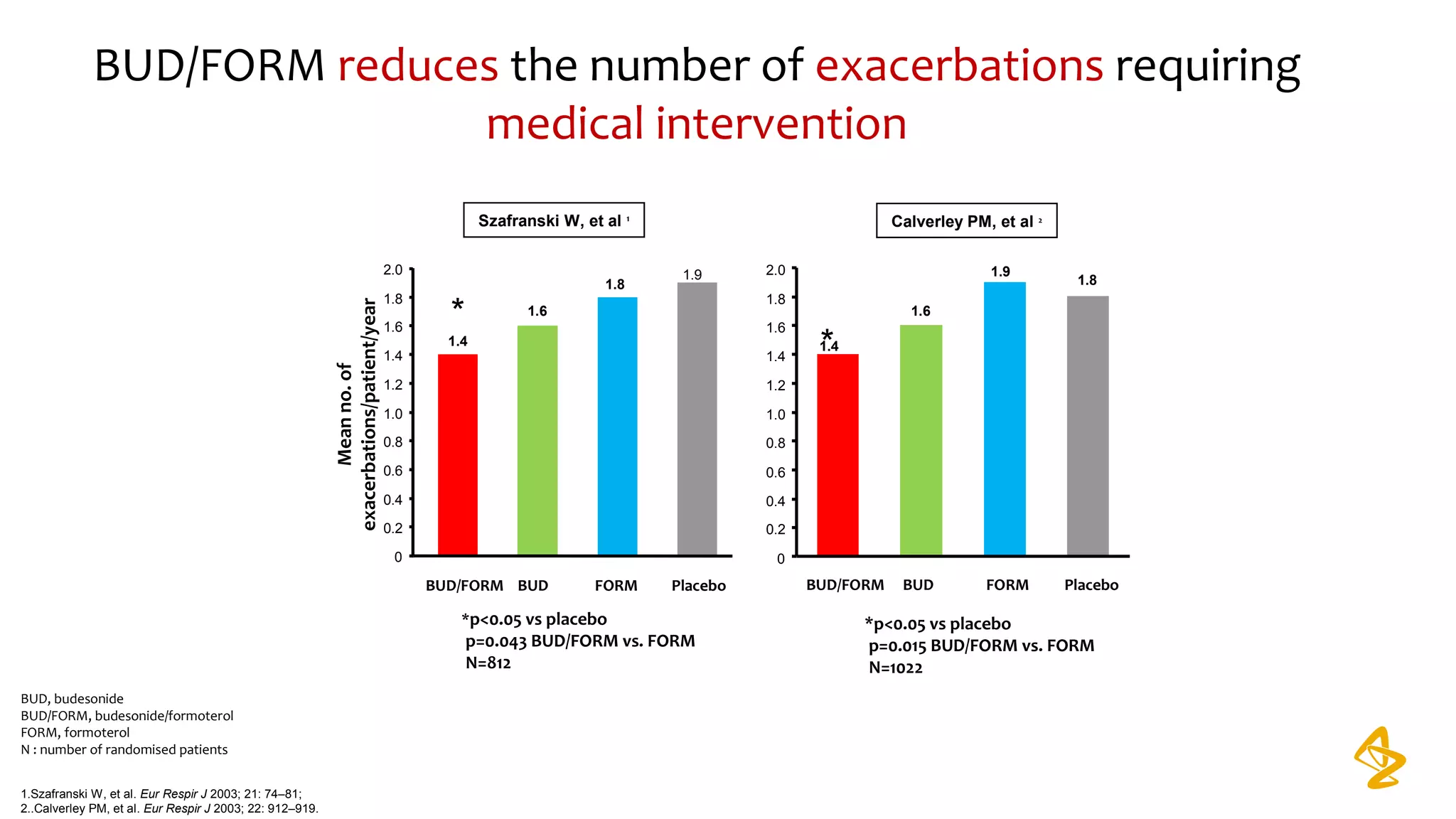
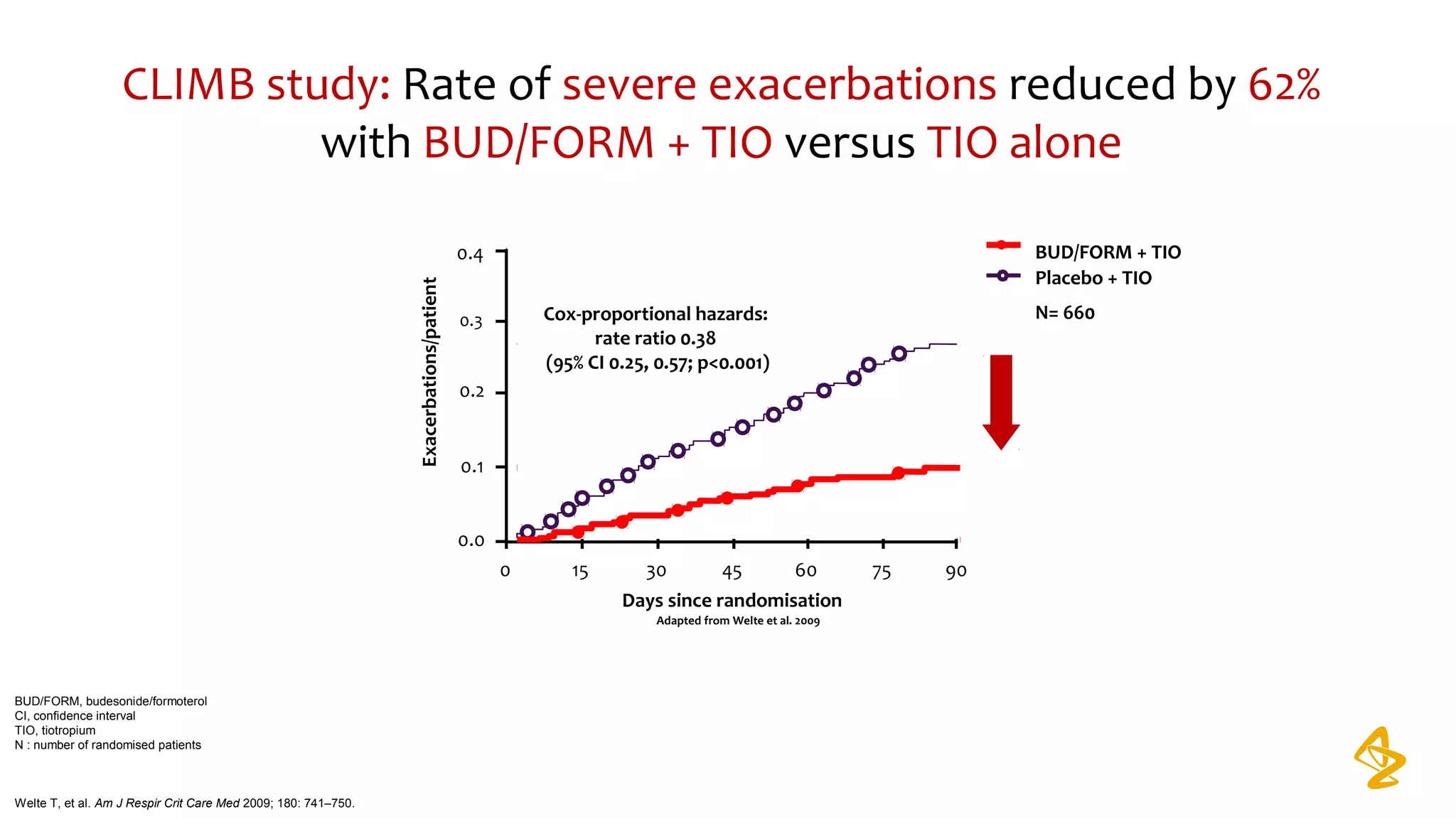
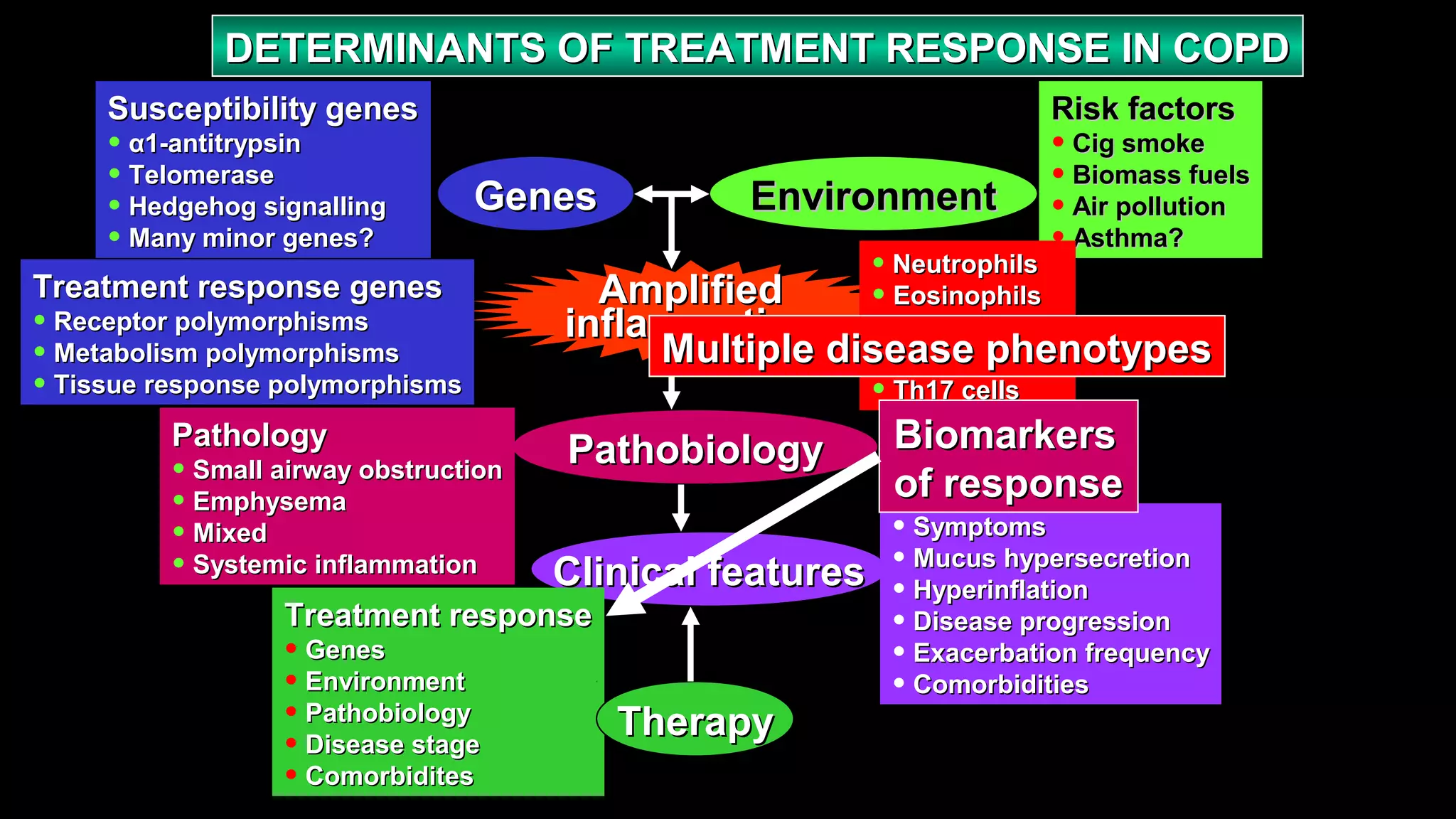
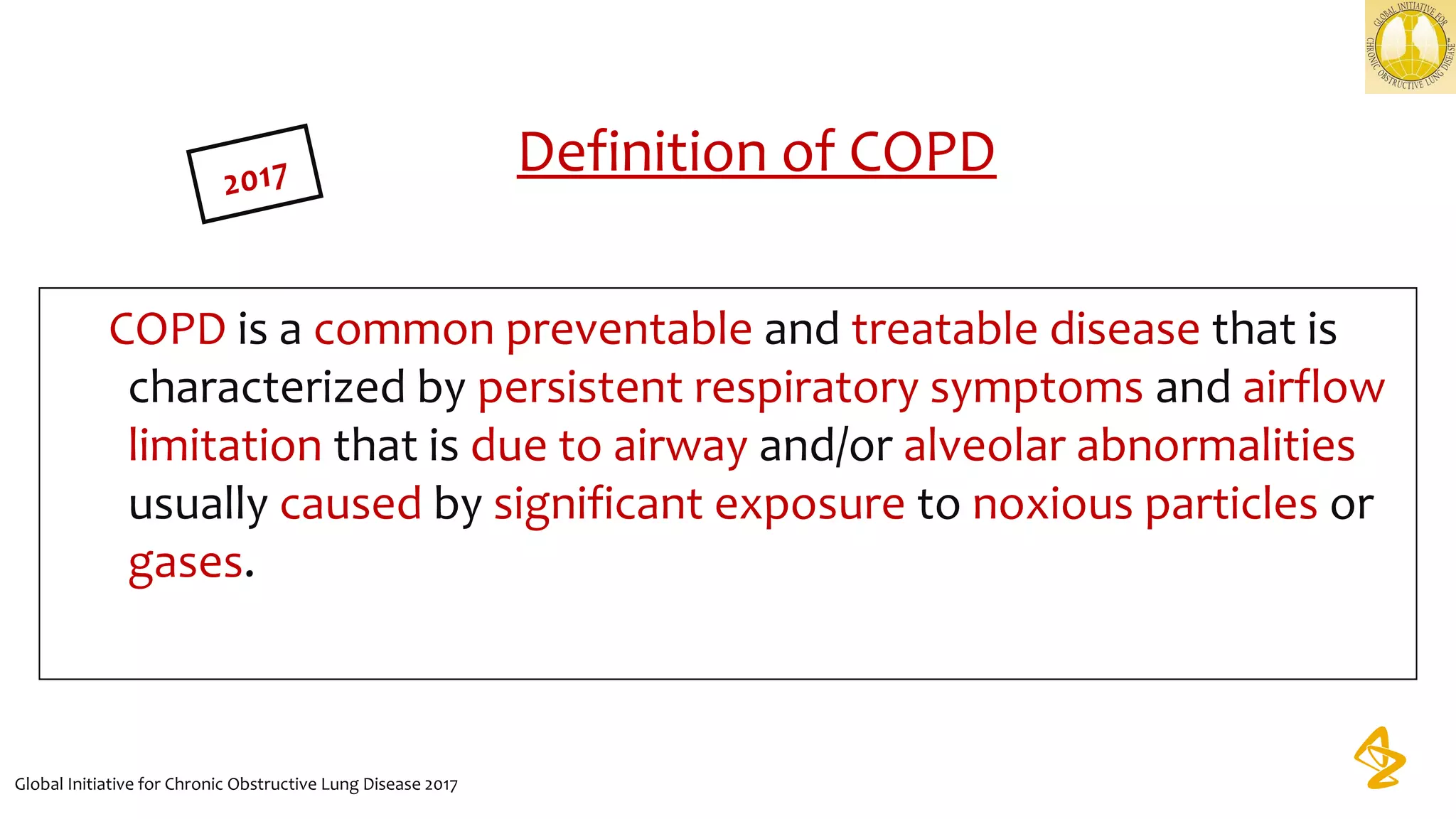
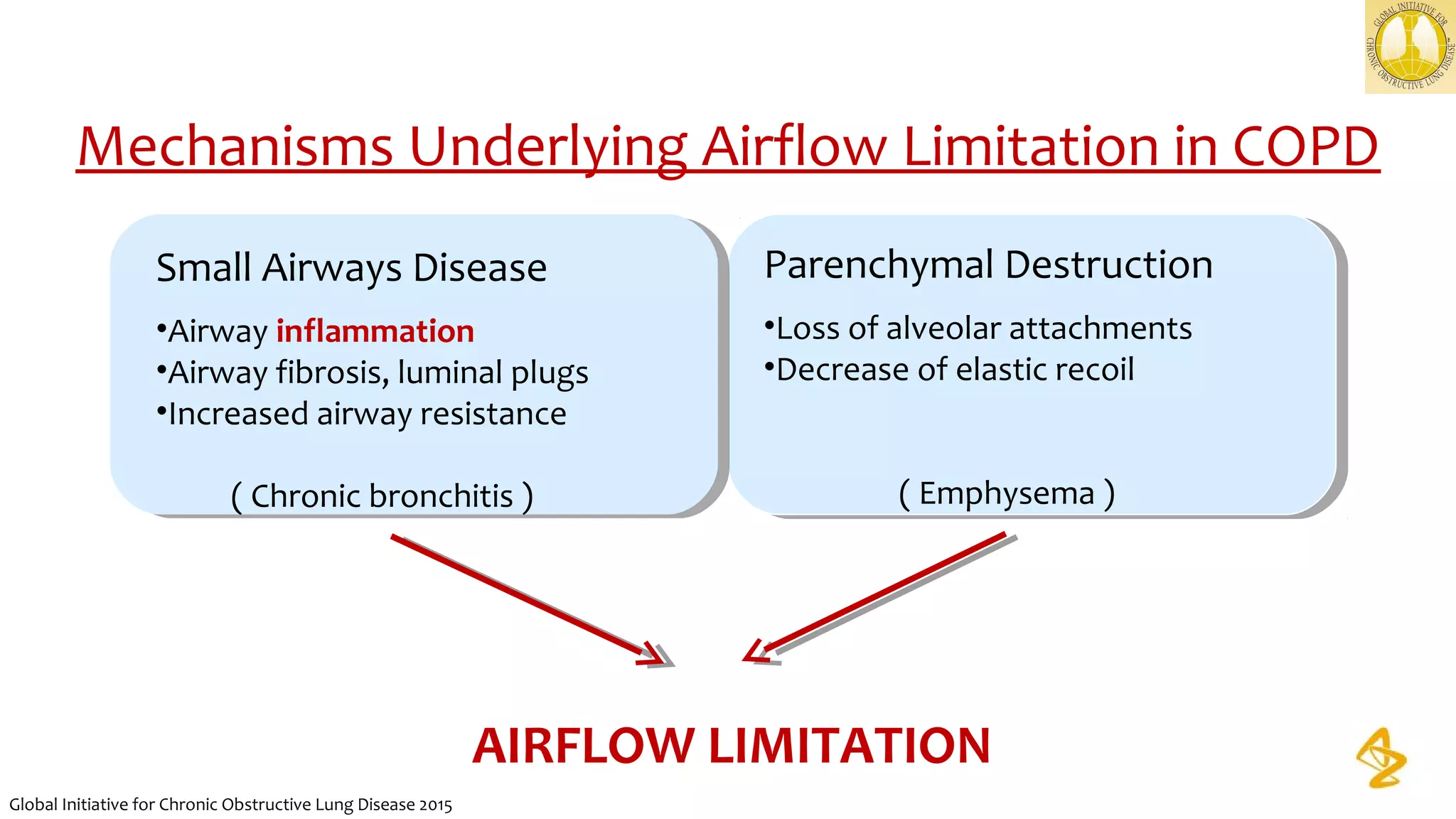
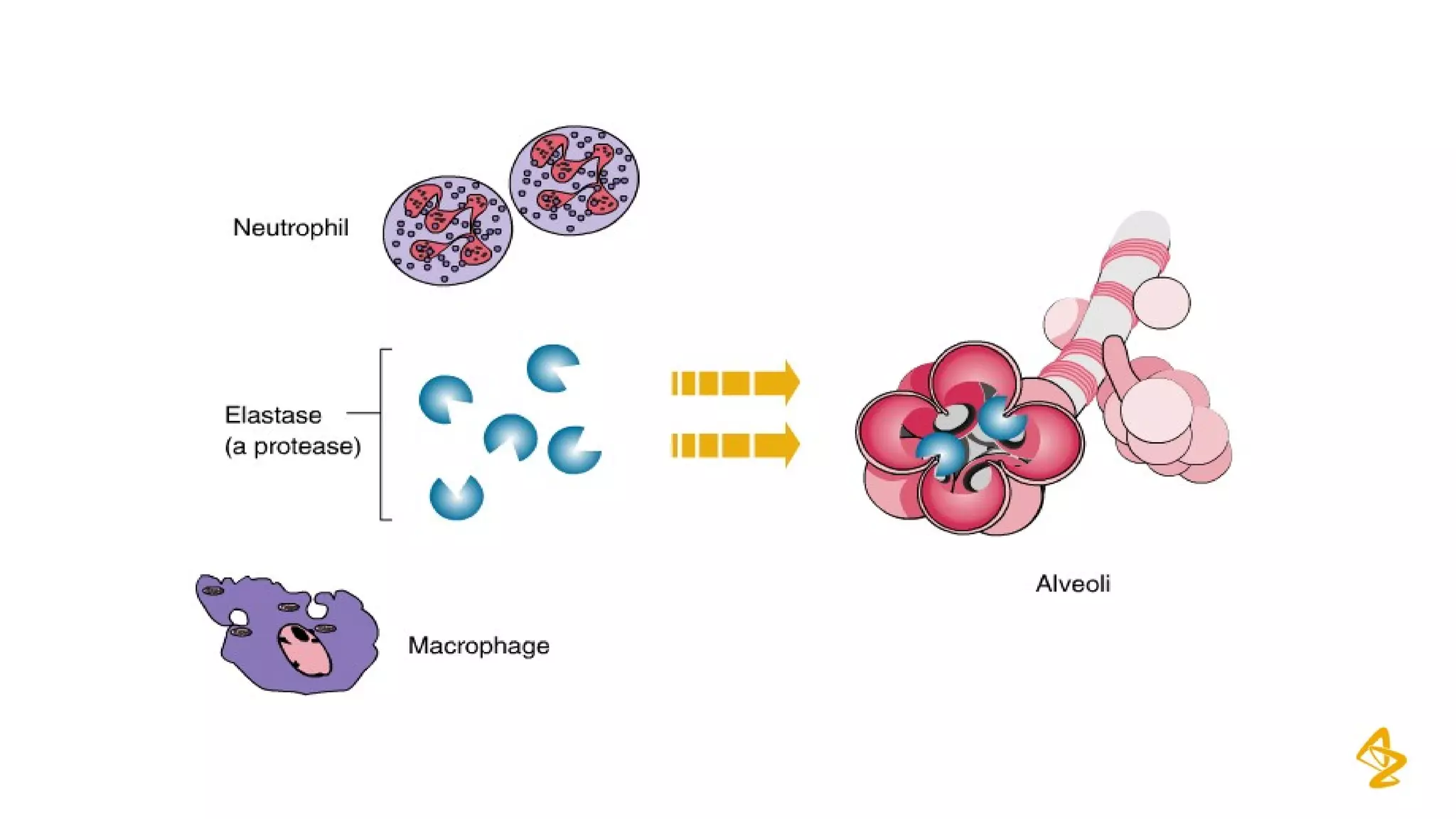
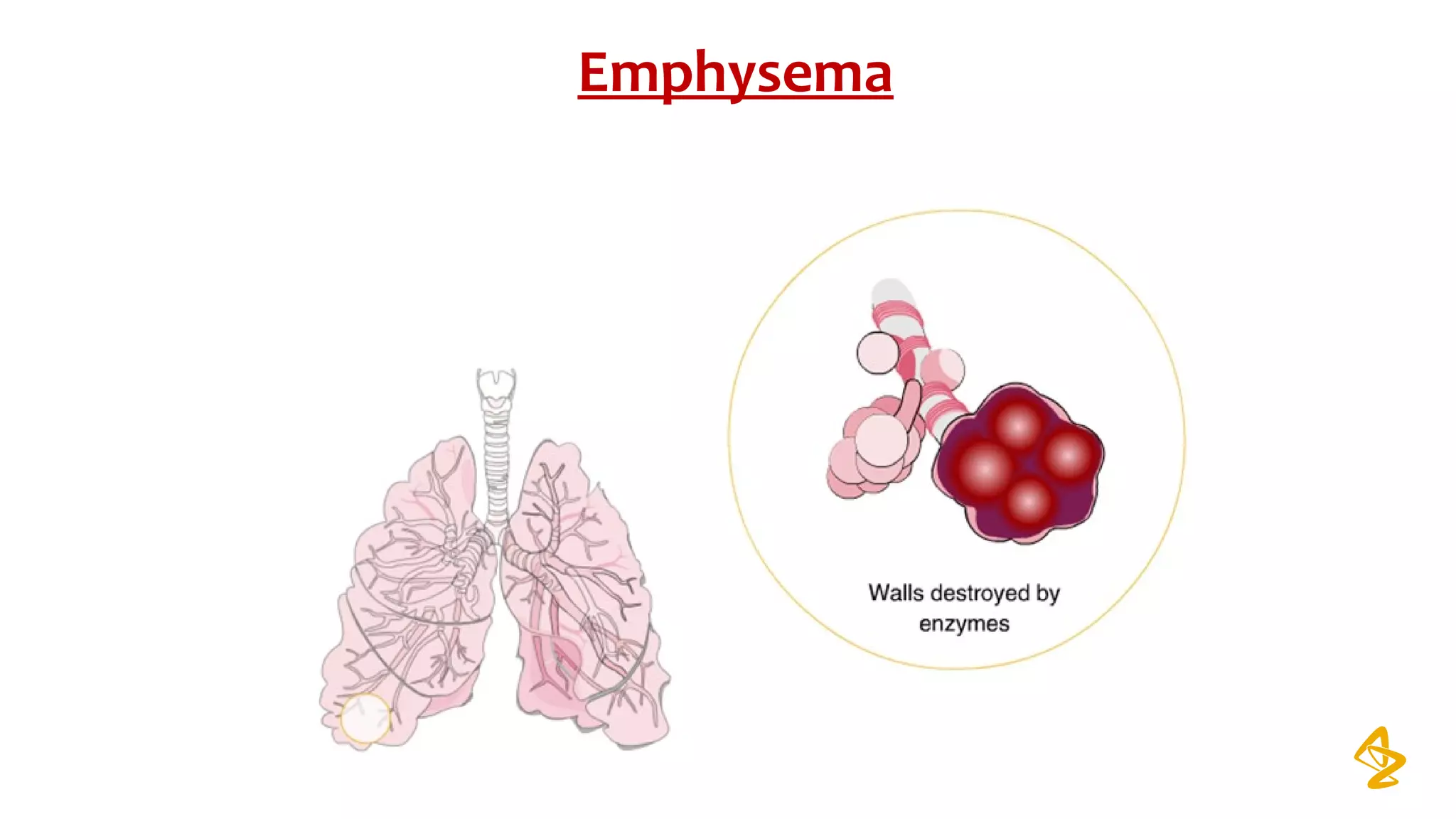
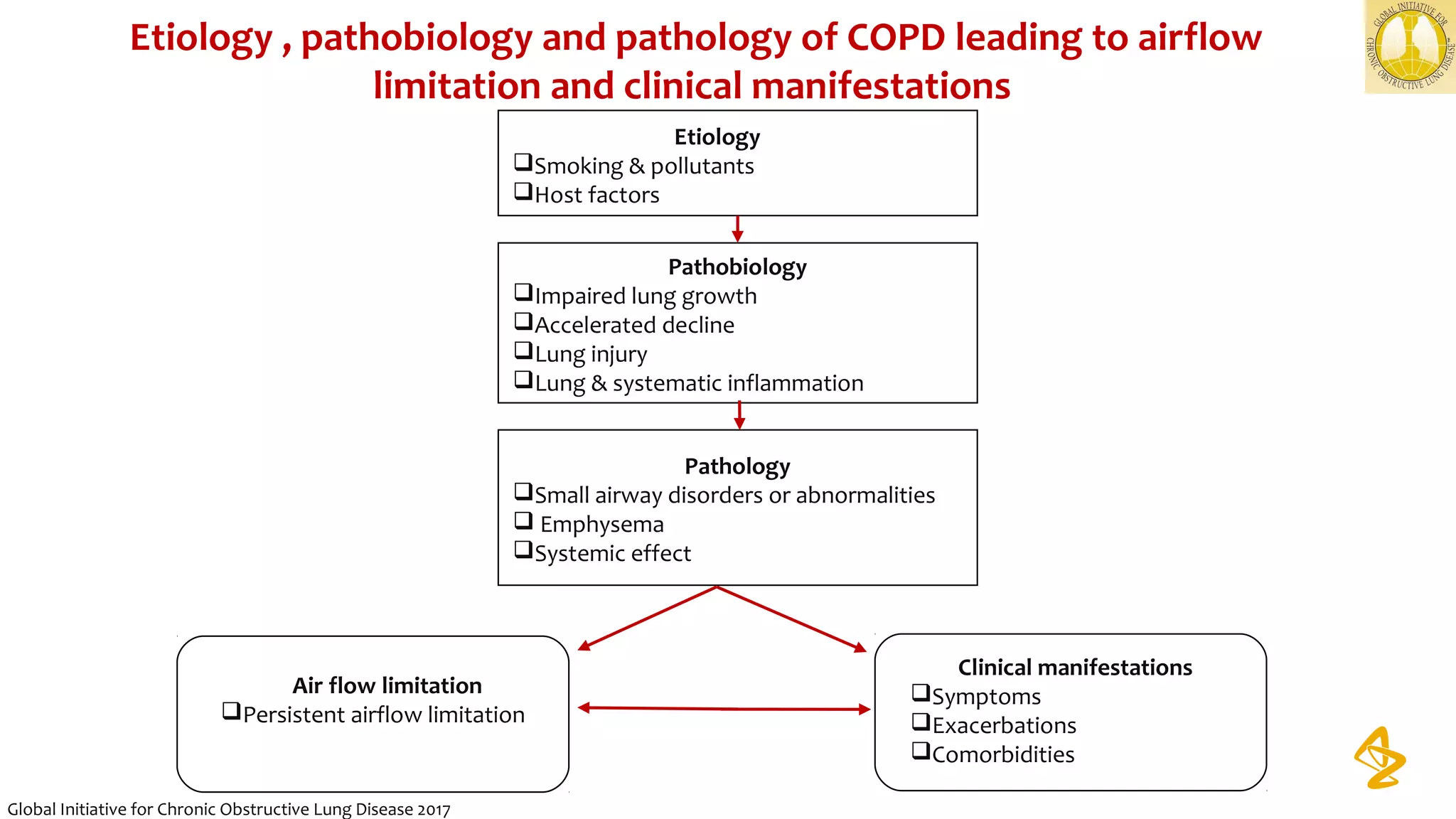
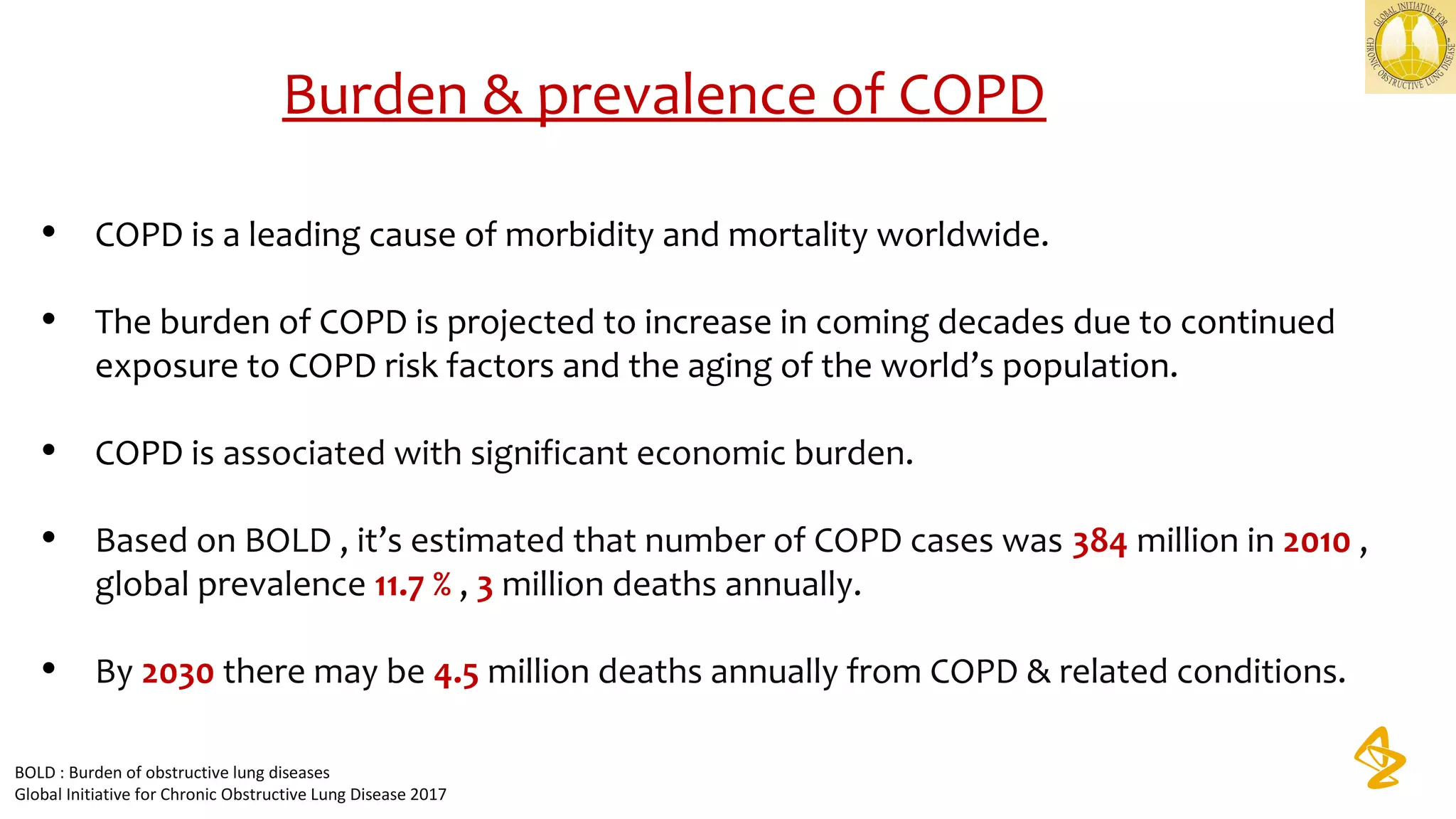
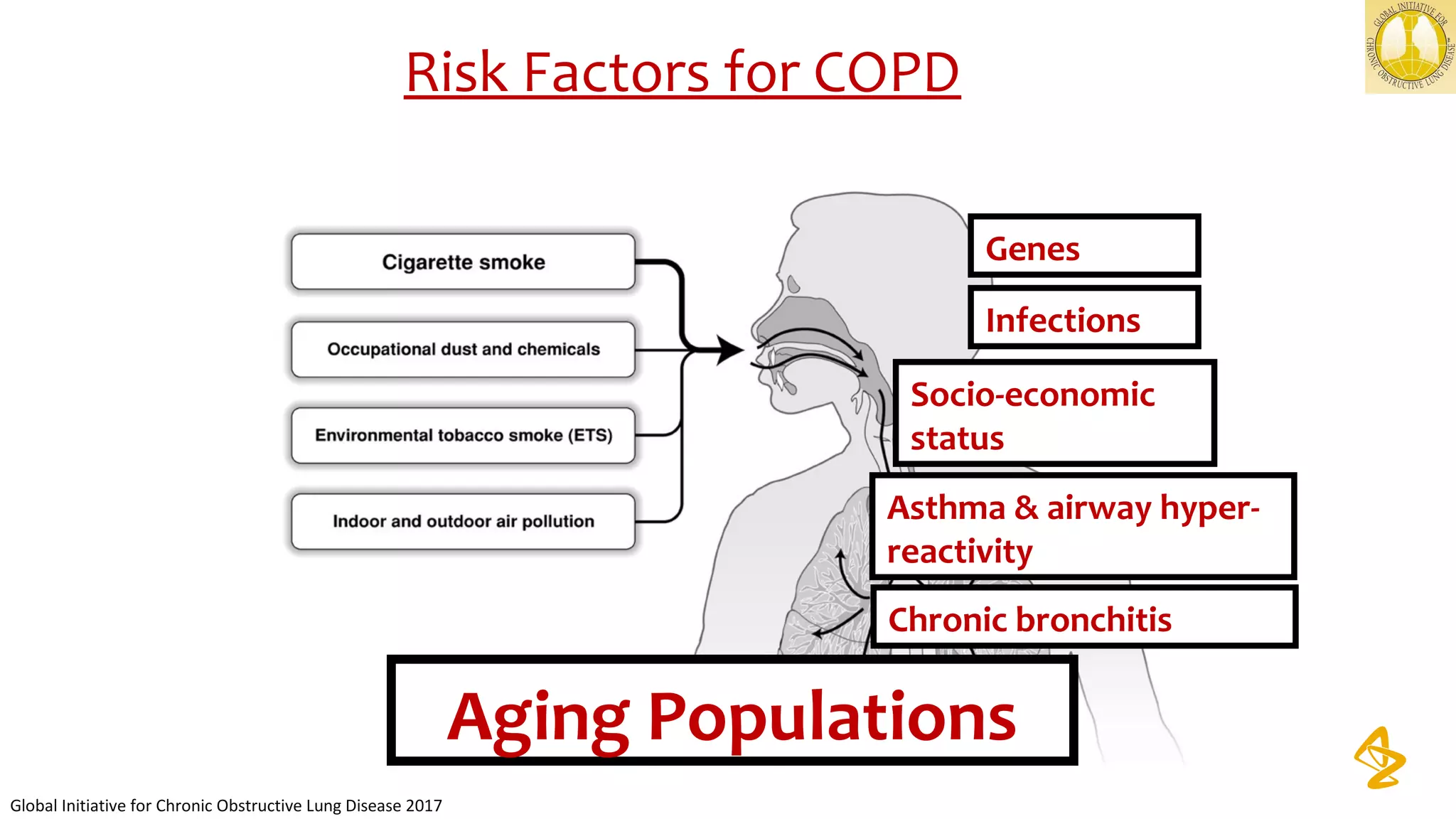
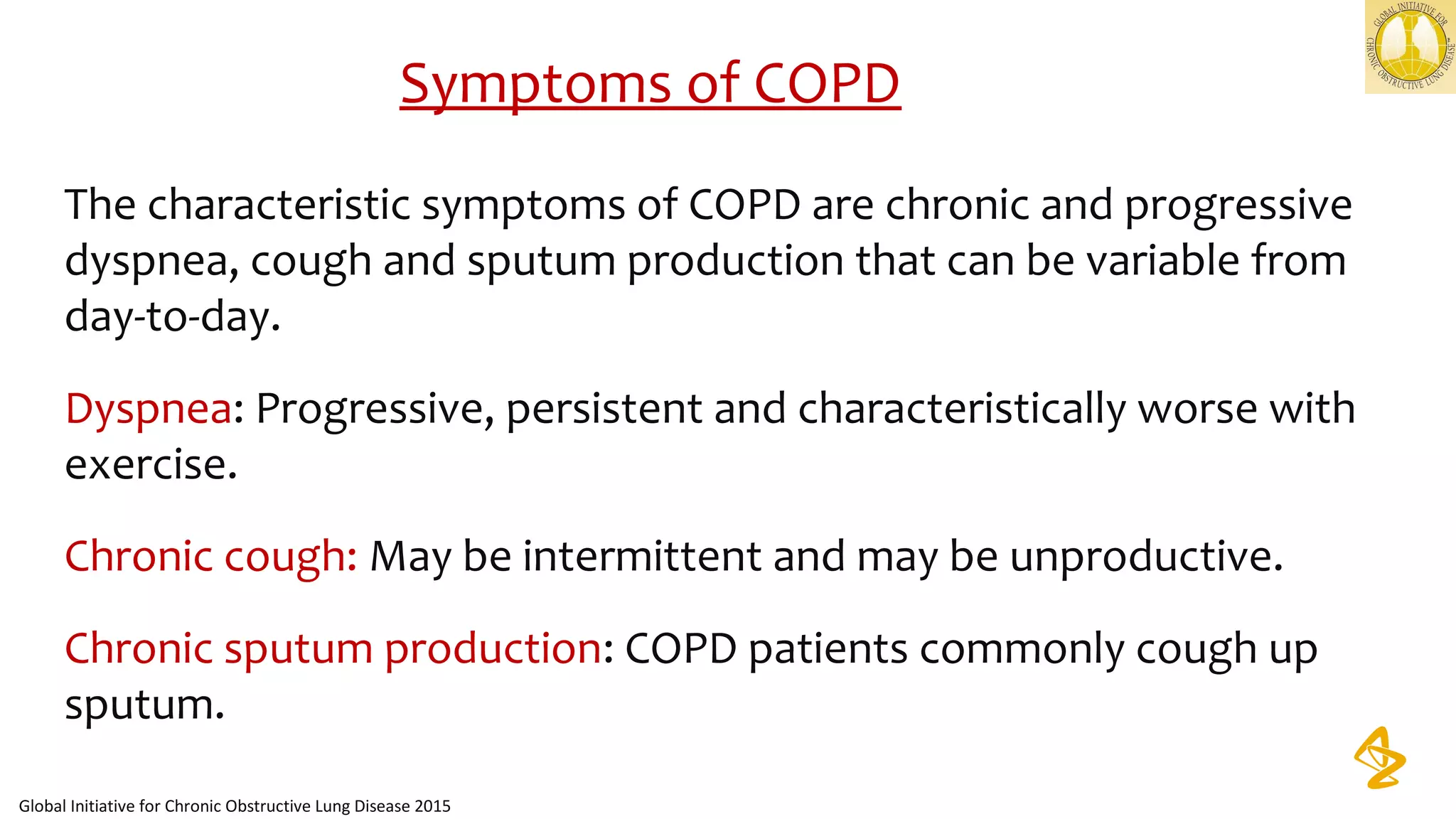
1) The document discusses the role of inhaled corticosteroids in the management of COPD. It provides an overview of COPD definitions, mechanisms, diagnosis, assessment, and treatment options.
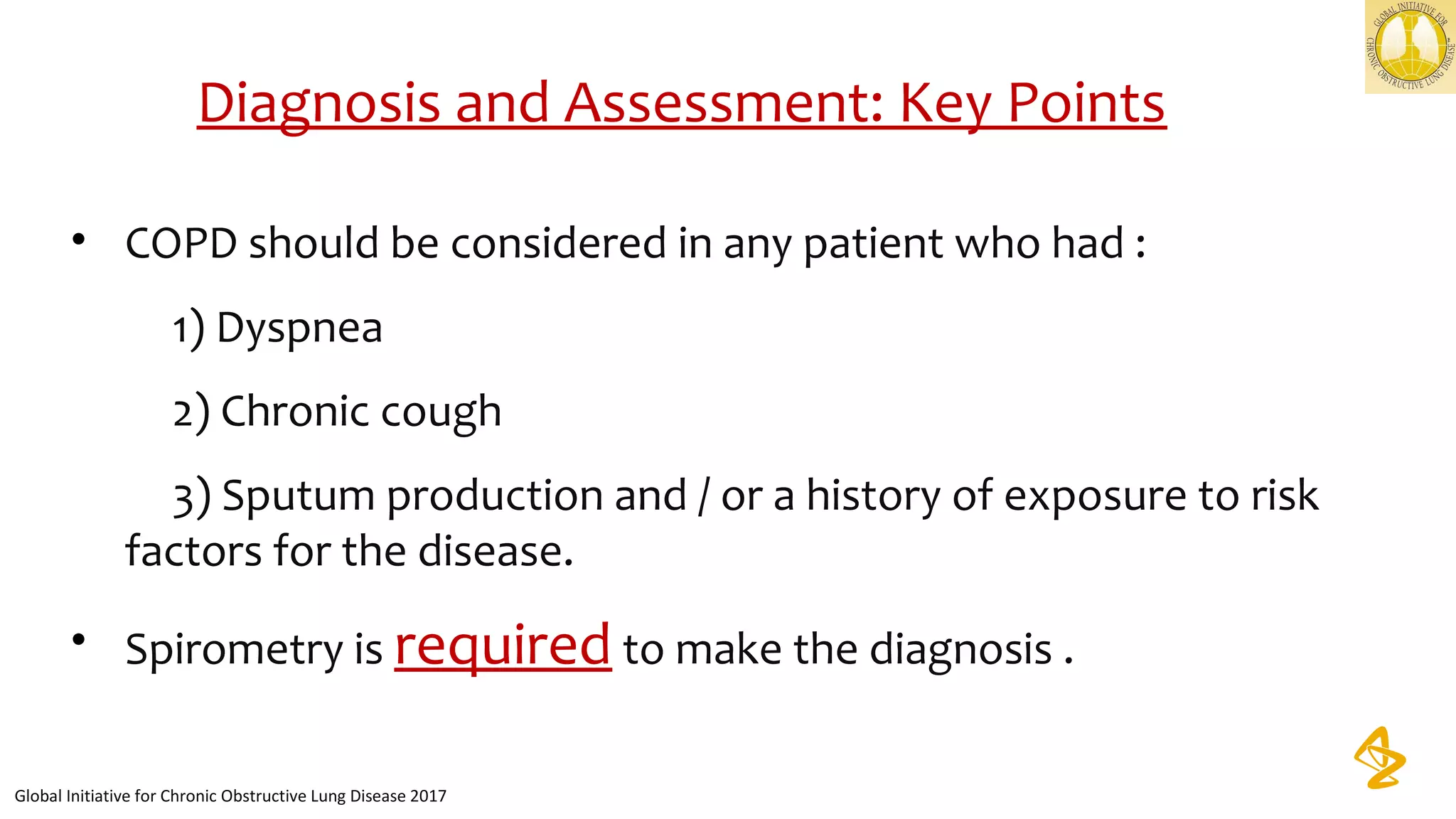
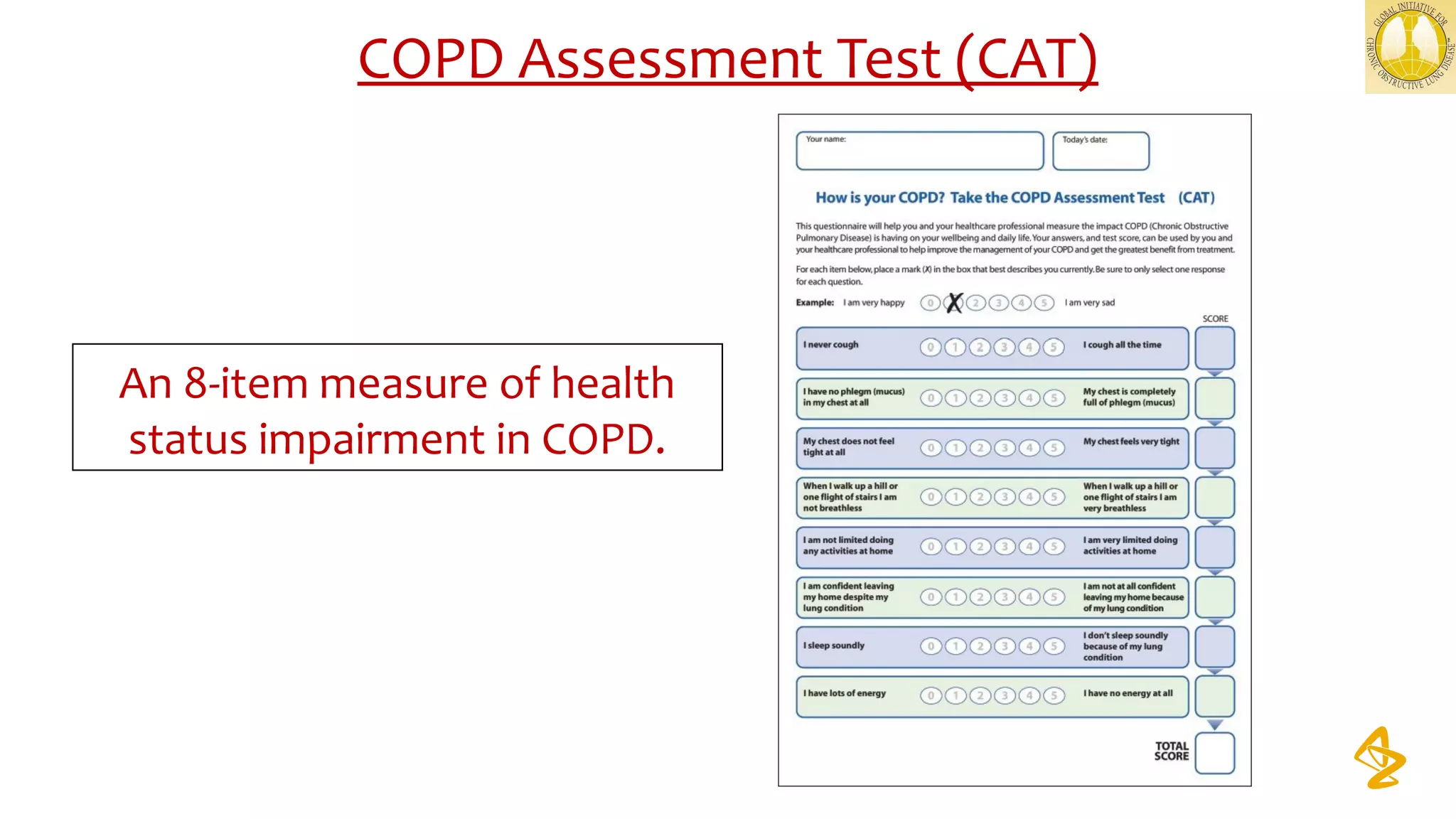
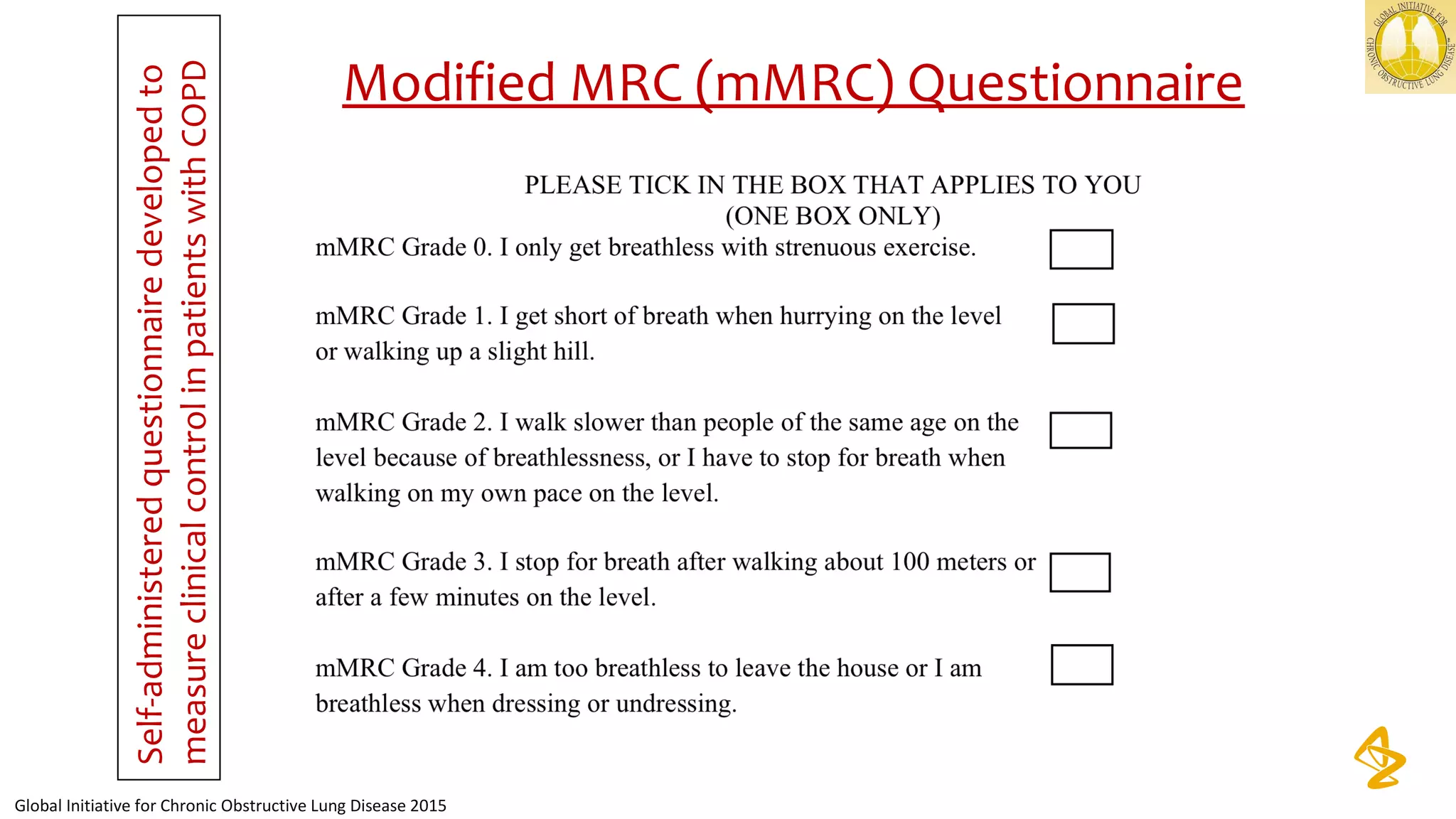
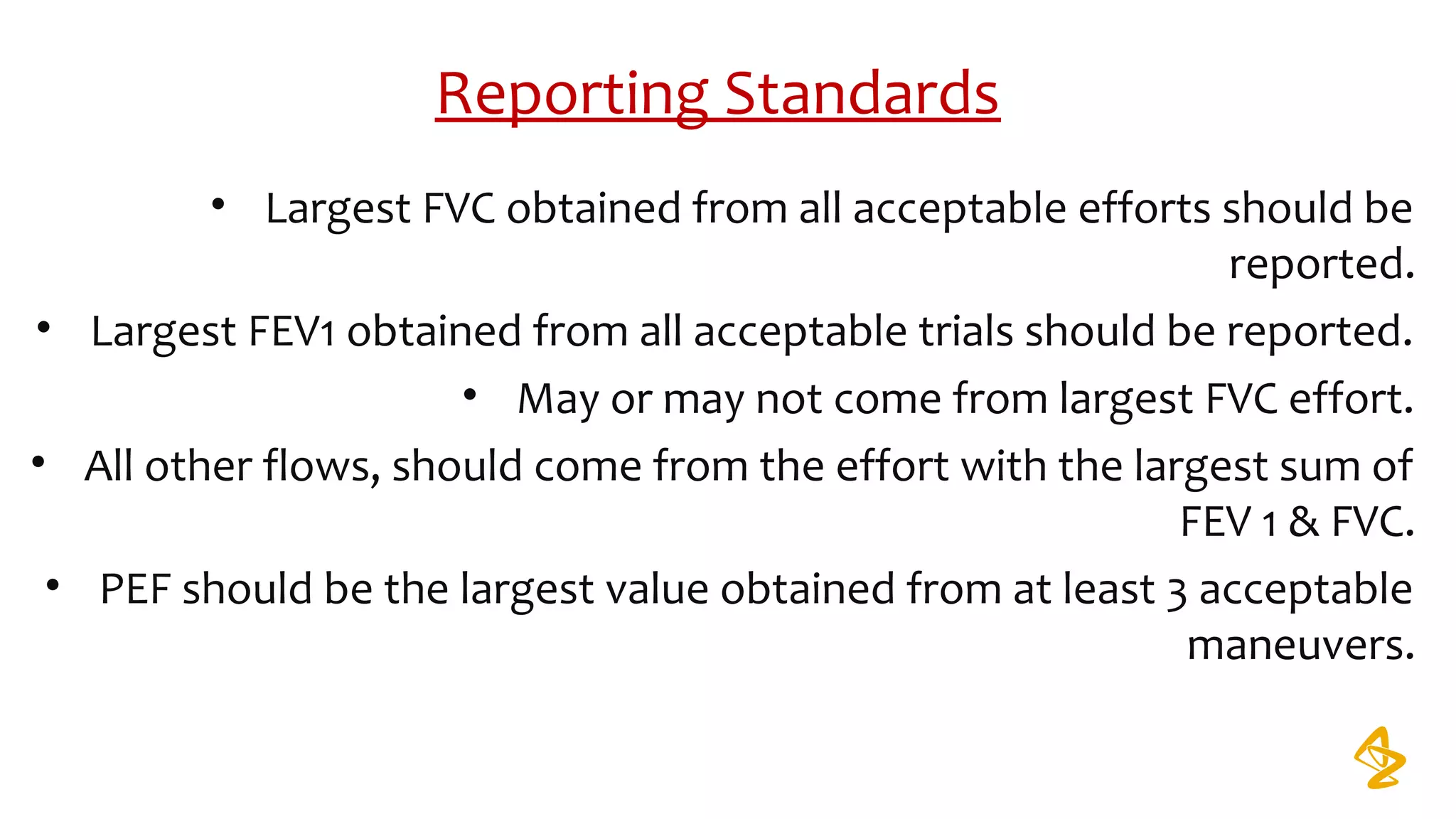
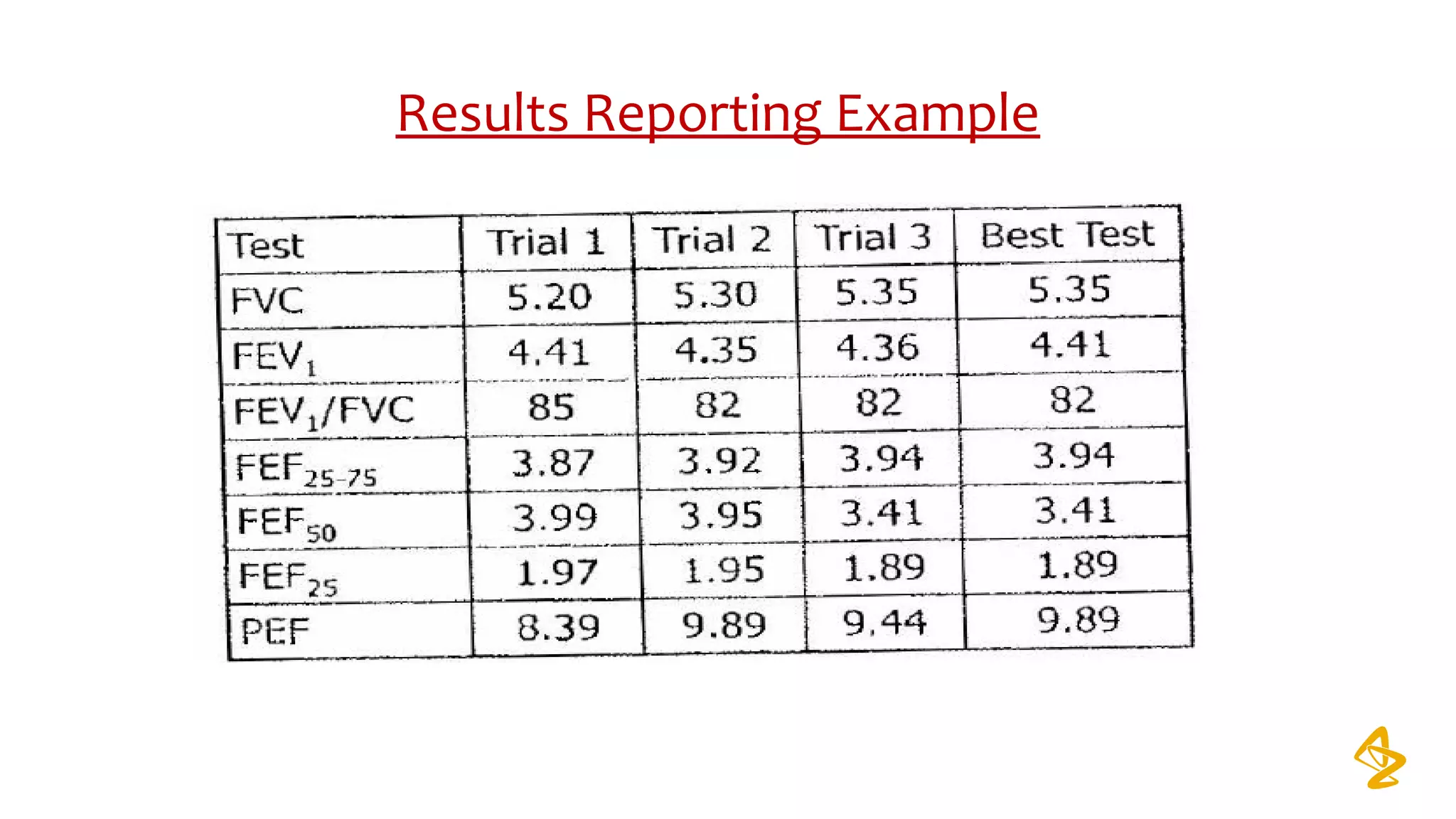
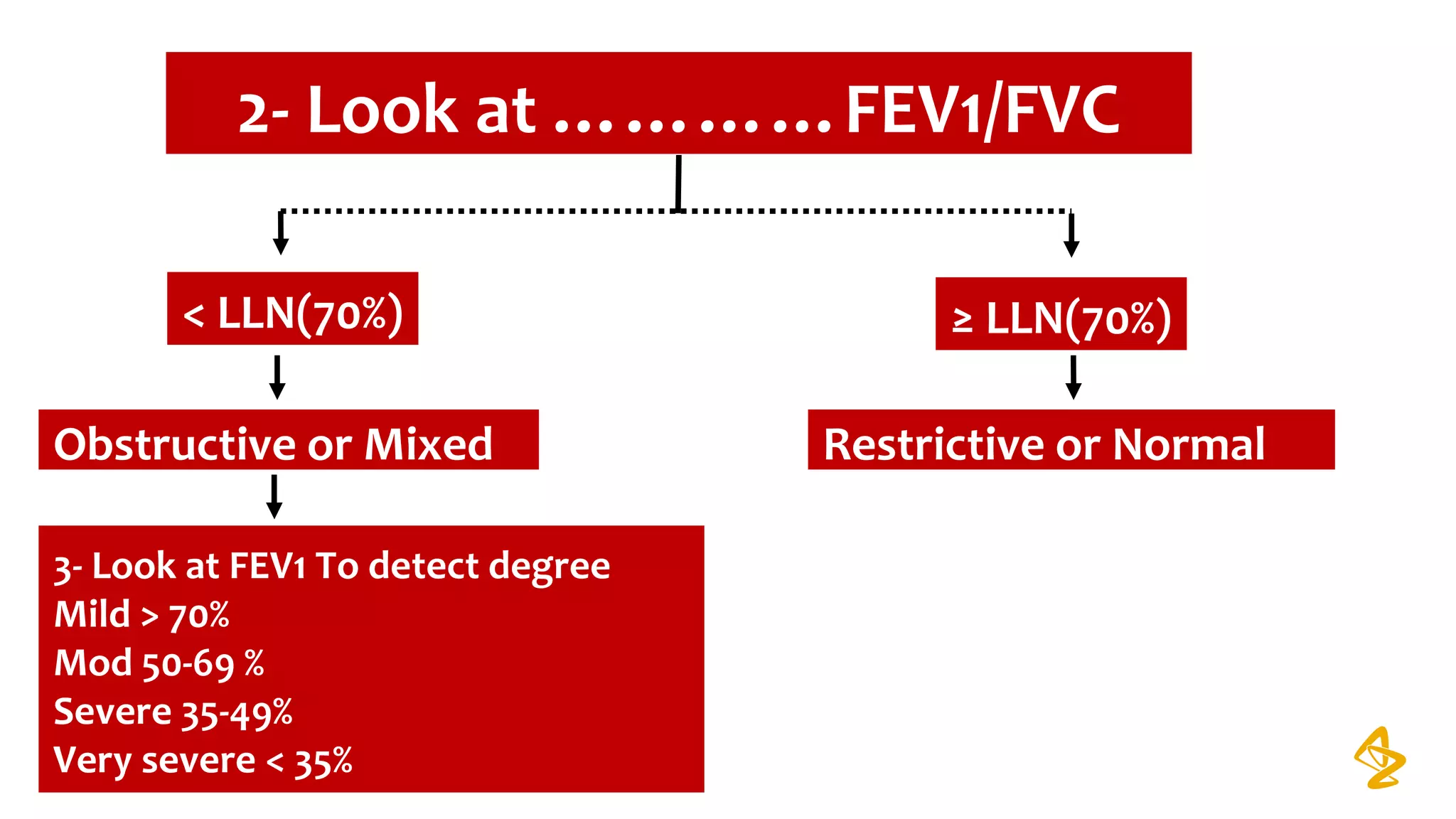
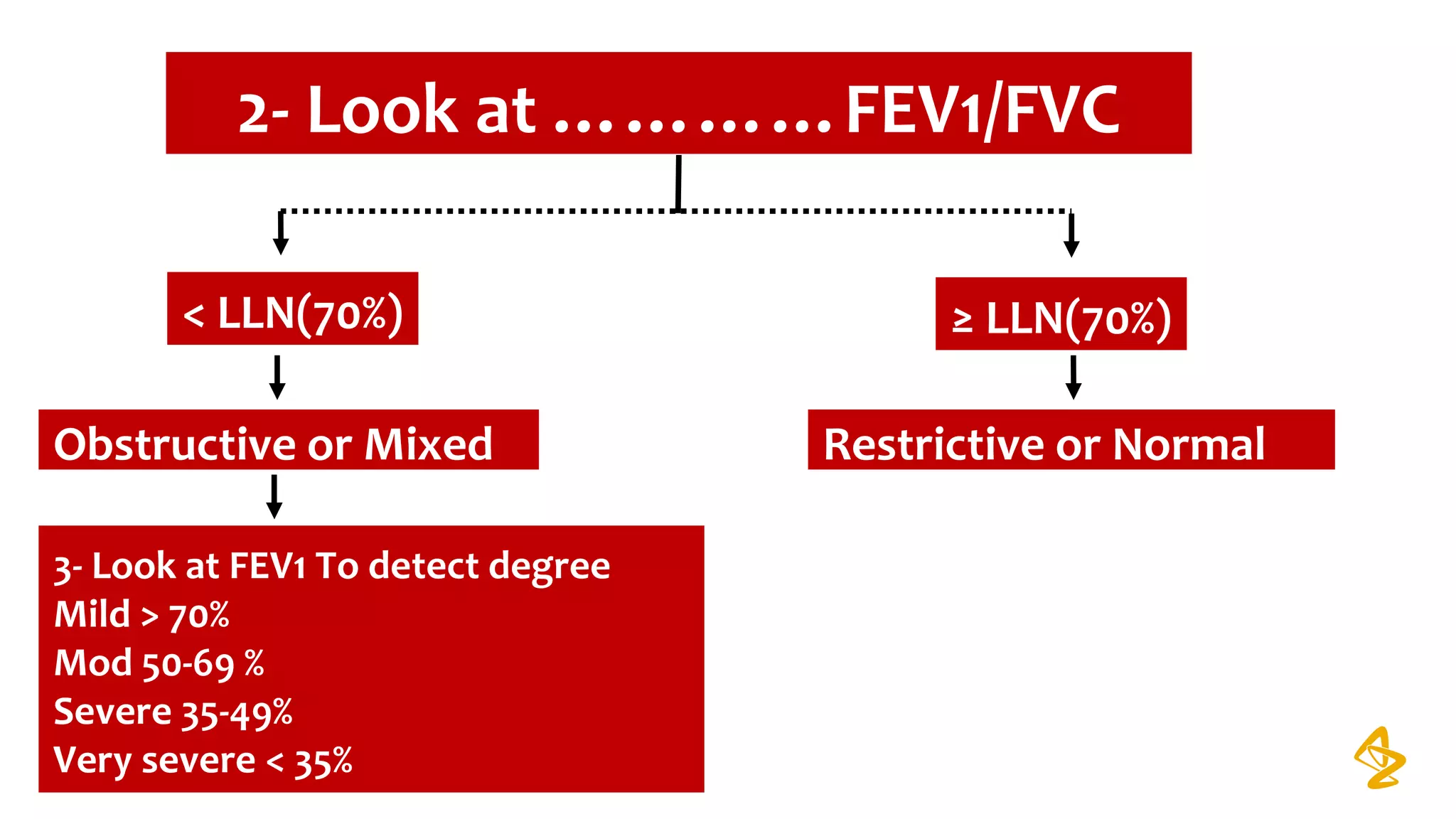
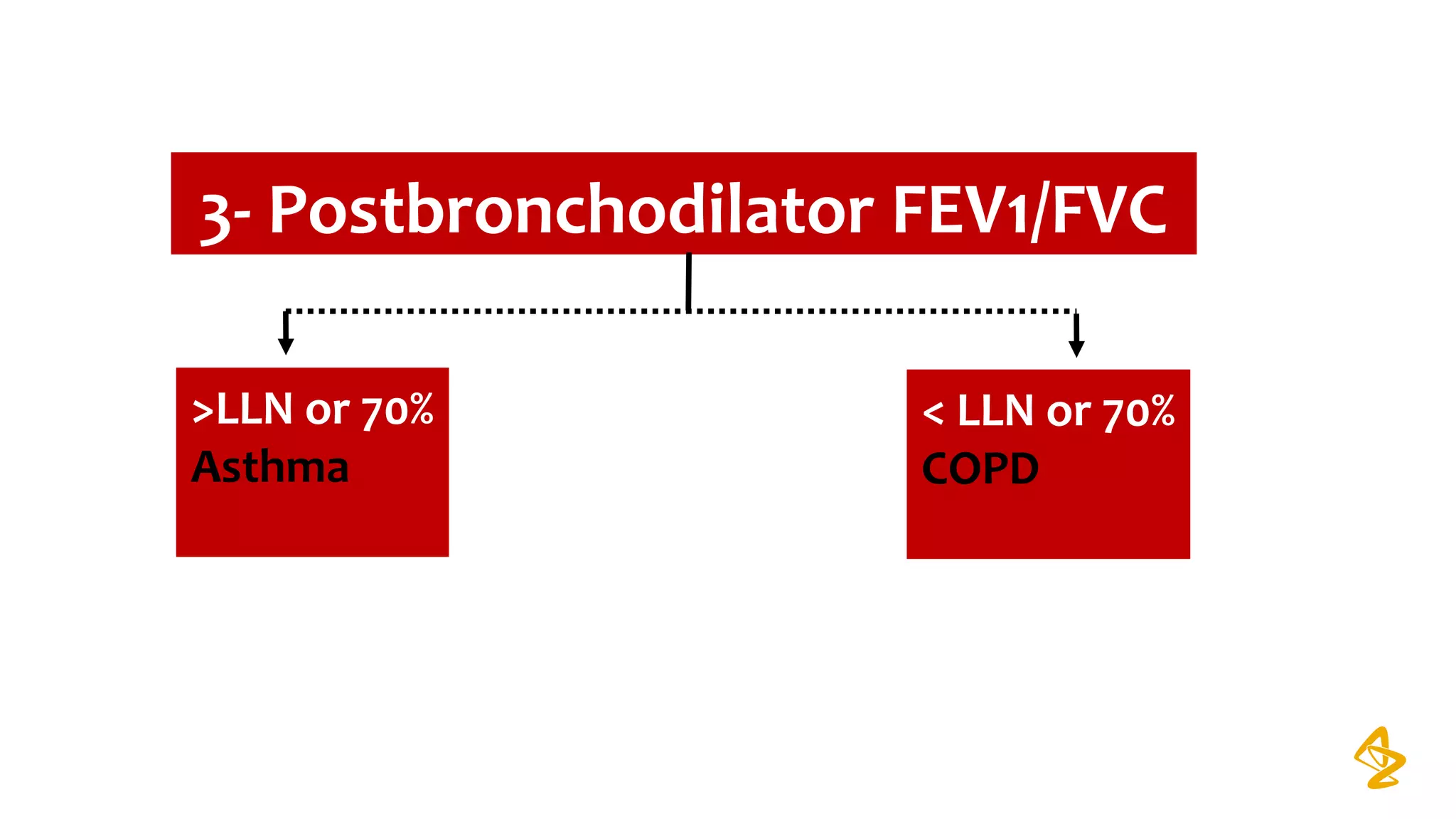
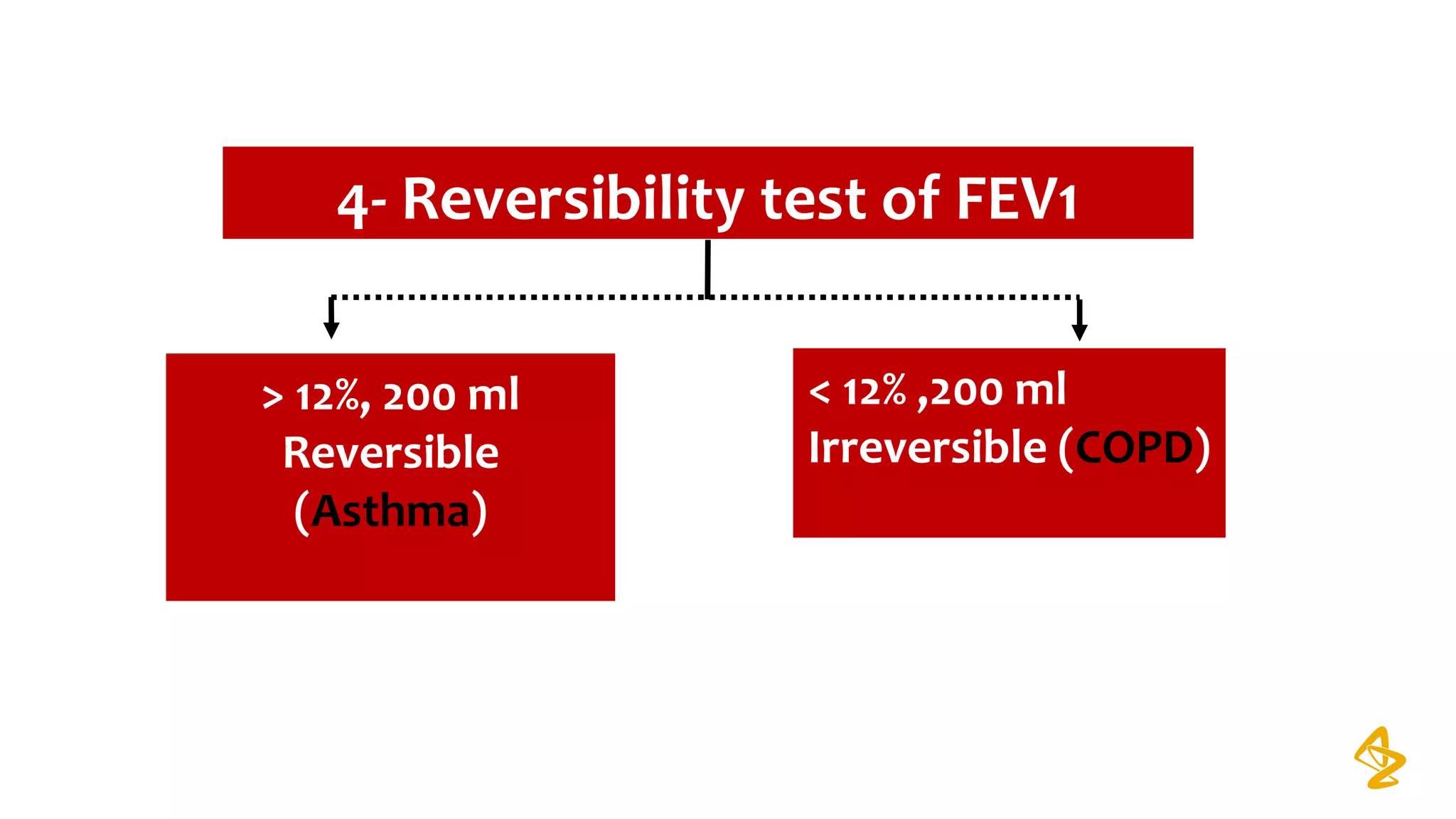
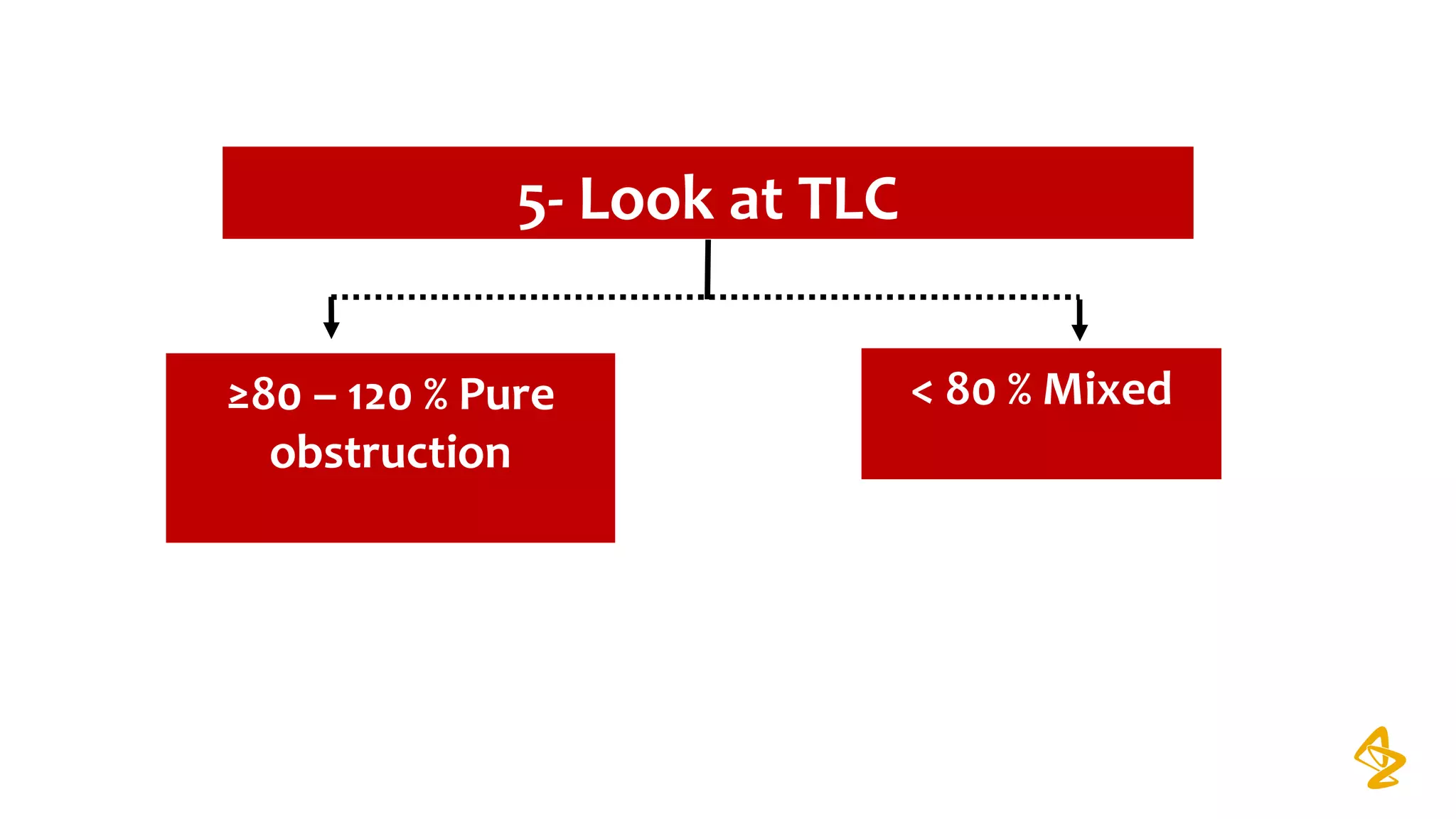
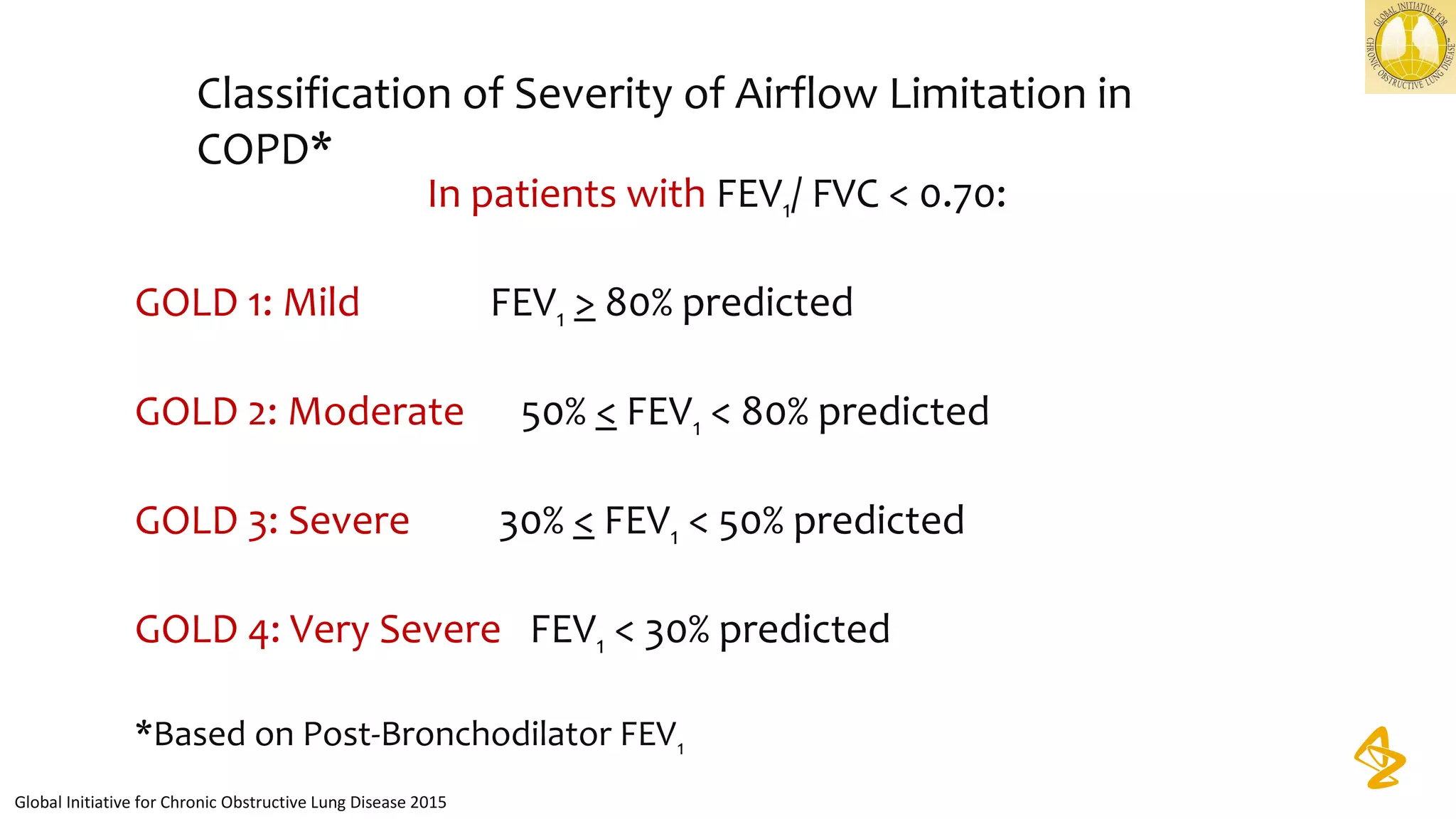
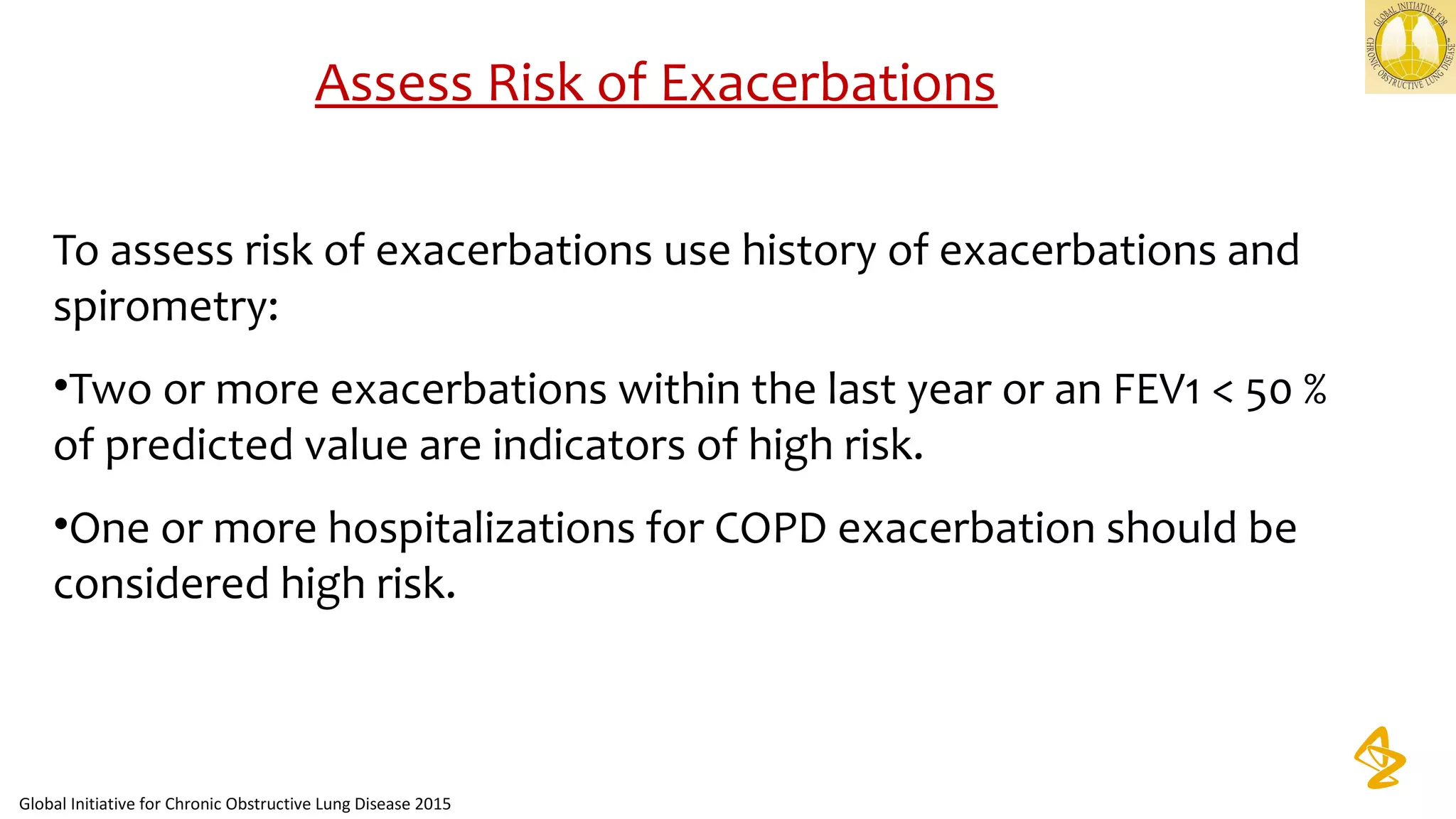
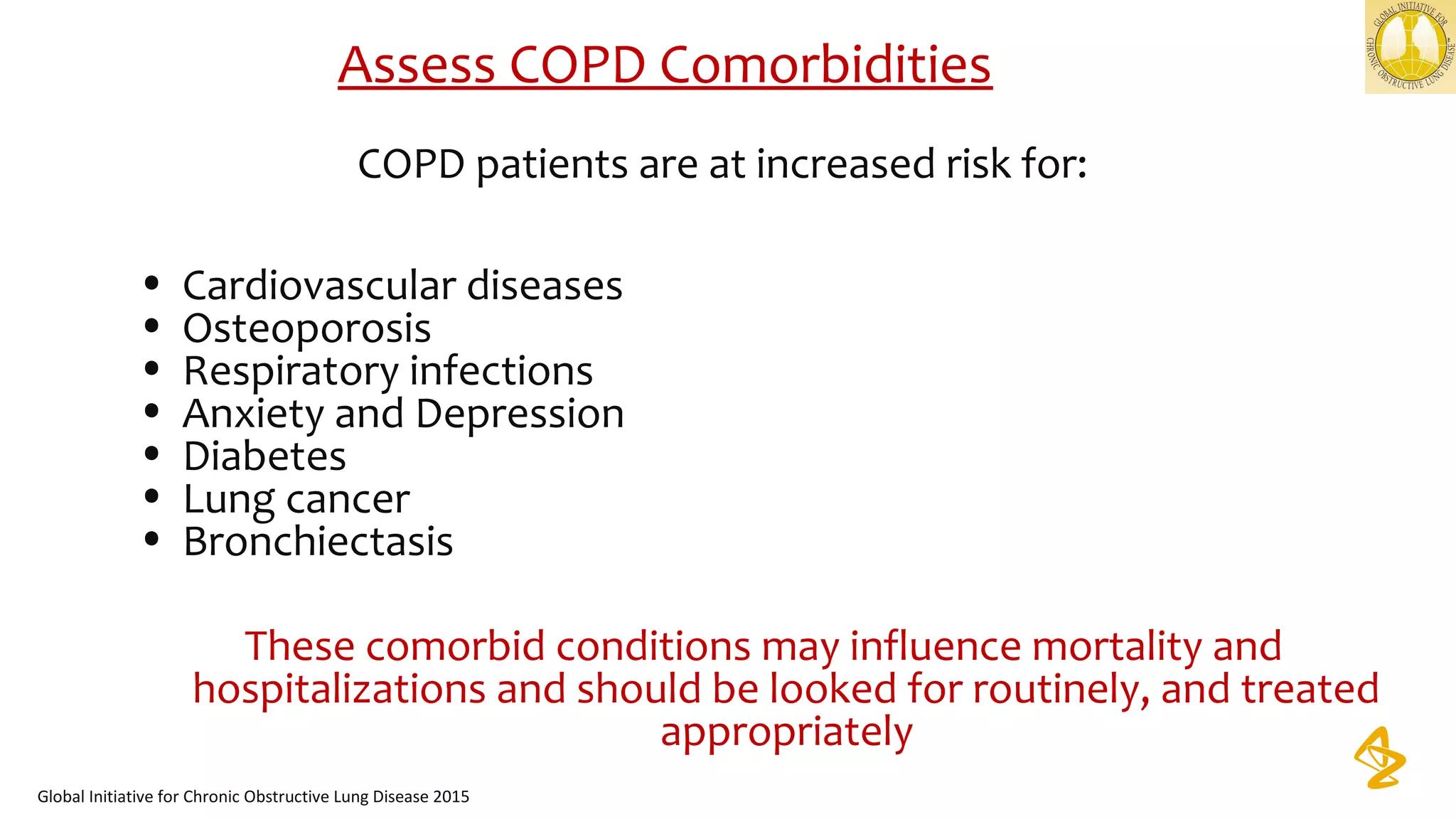
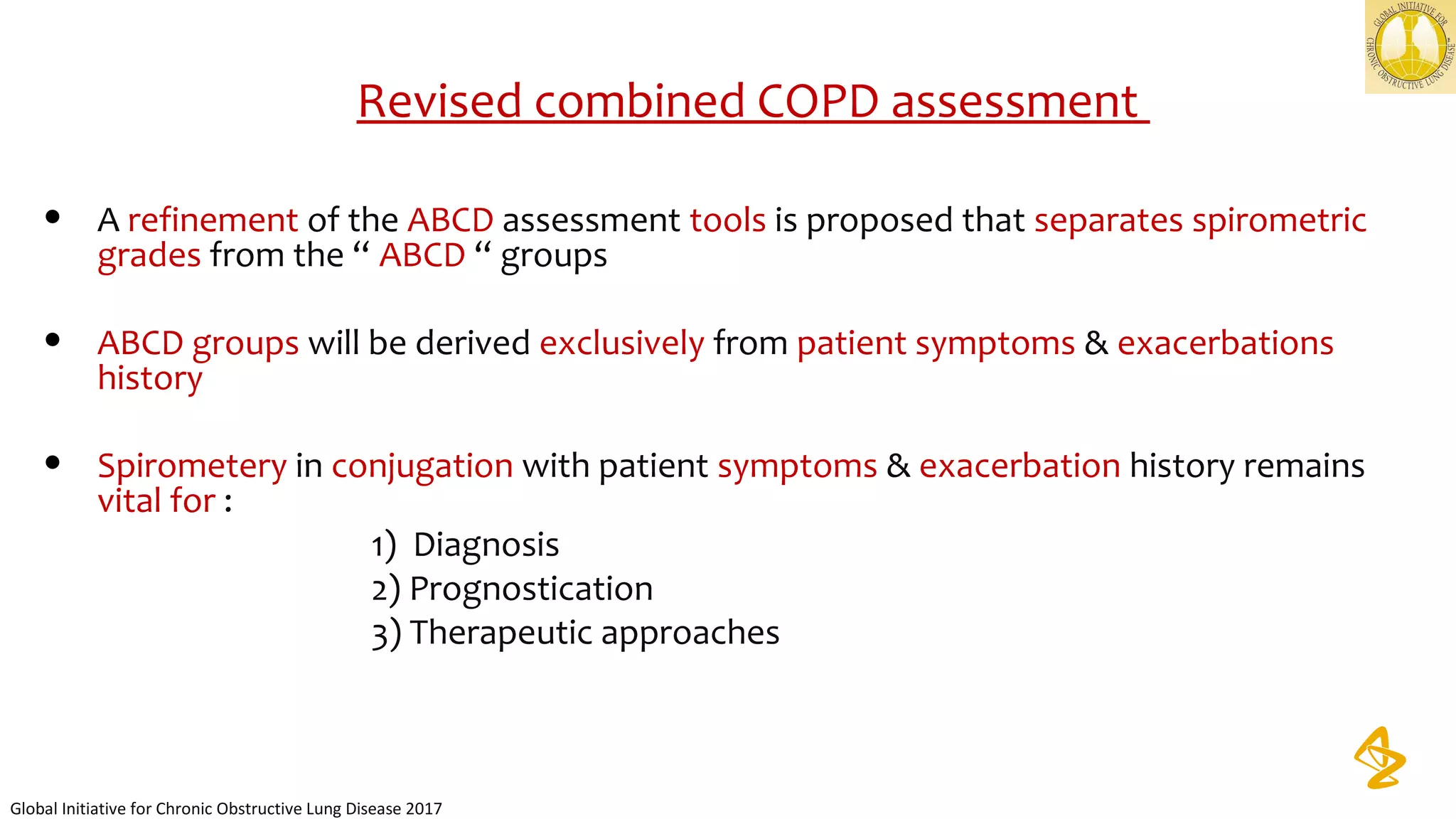
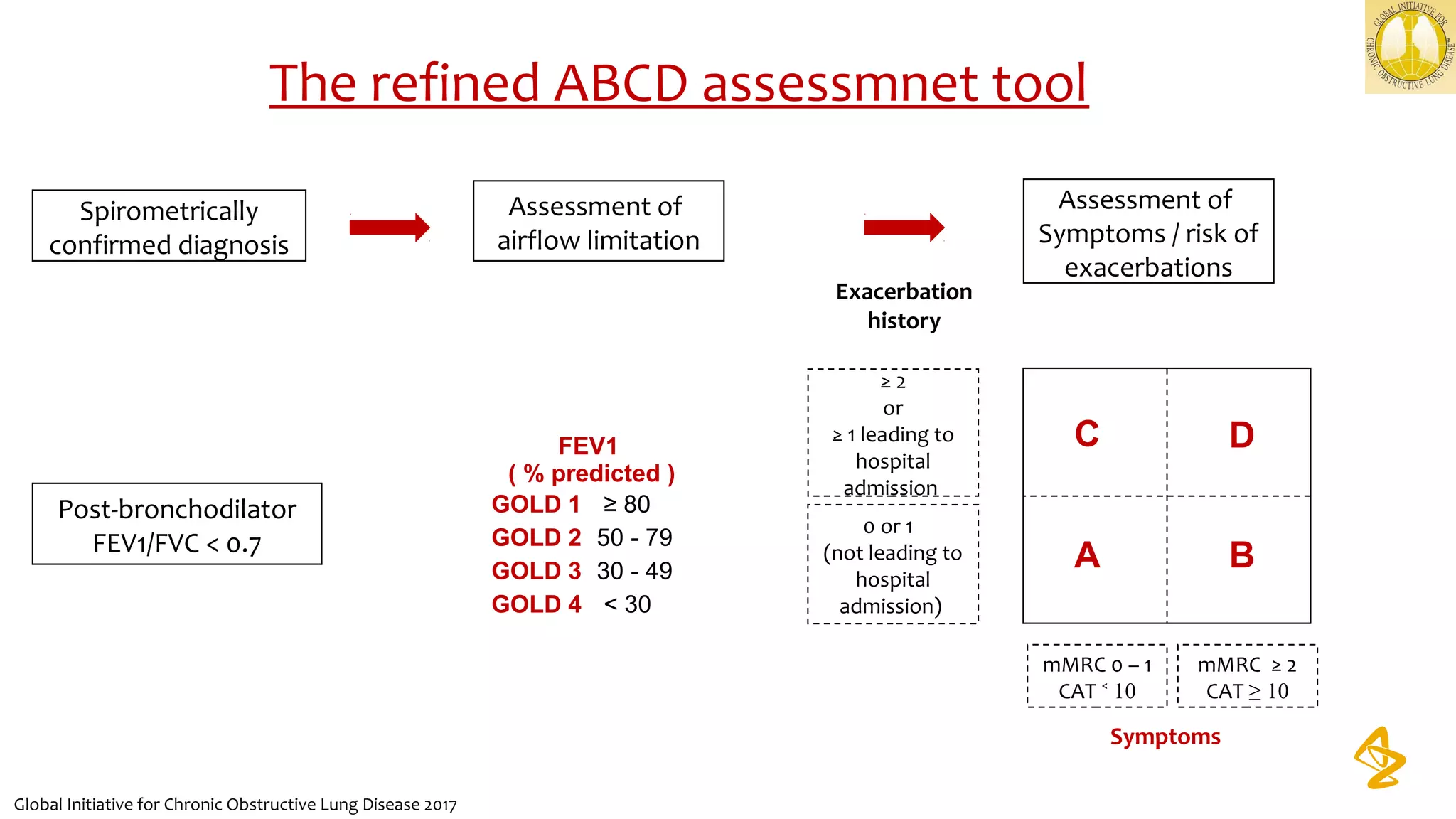
2) Spirometry is required for diagnosis of COPD and can assess severity based on airflow limitation. Symptoms, exacerbation history, and comorbidities are also assessed.
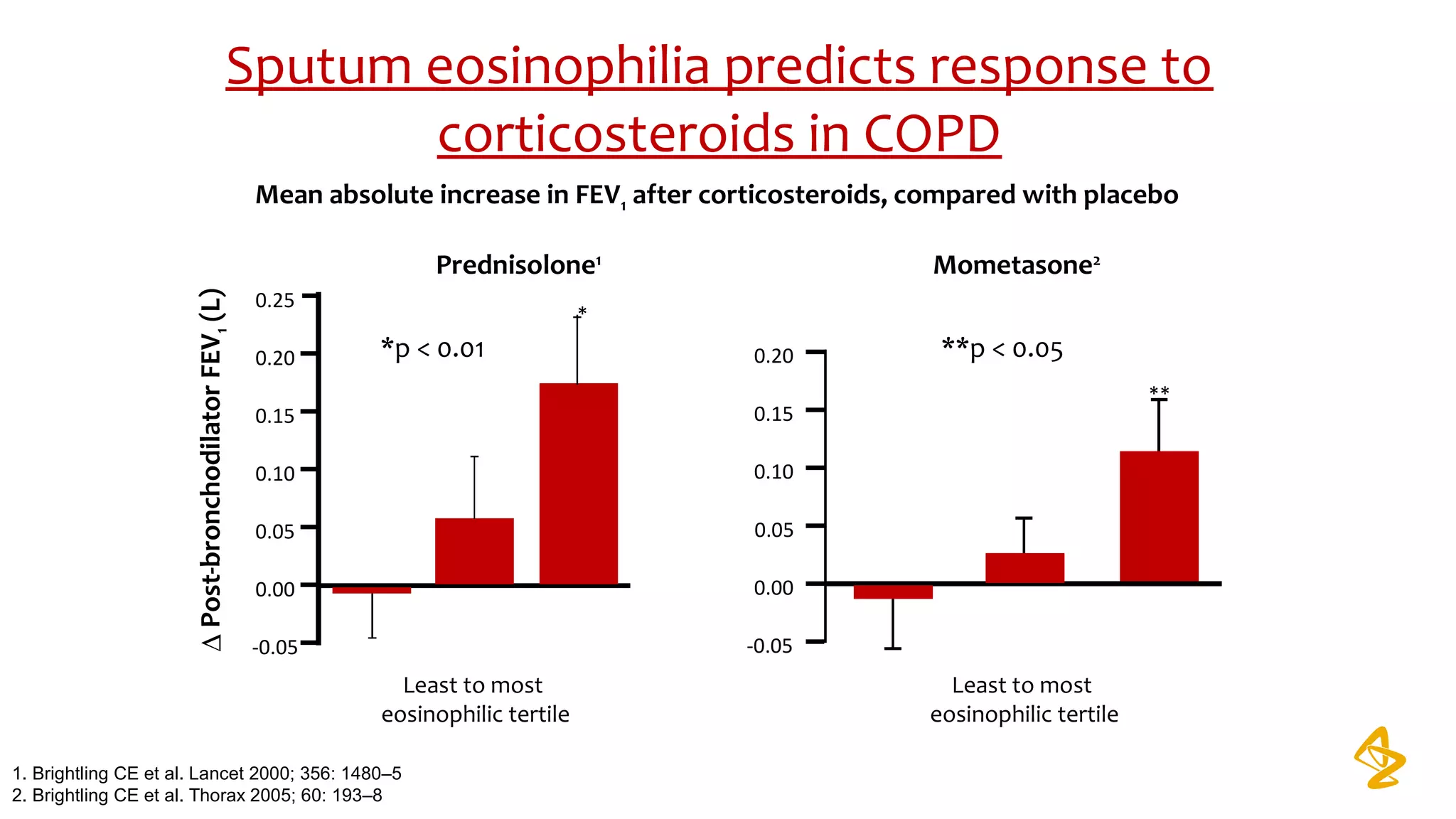
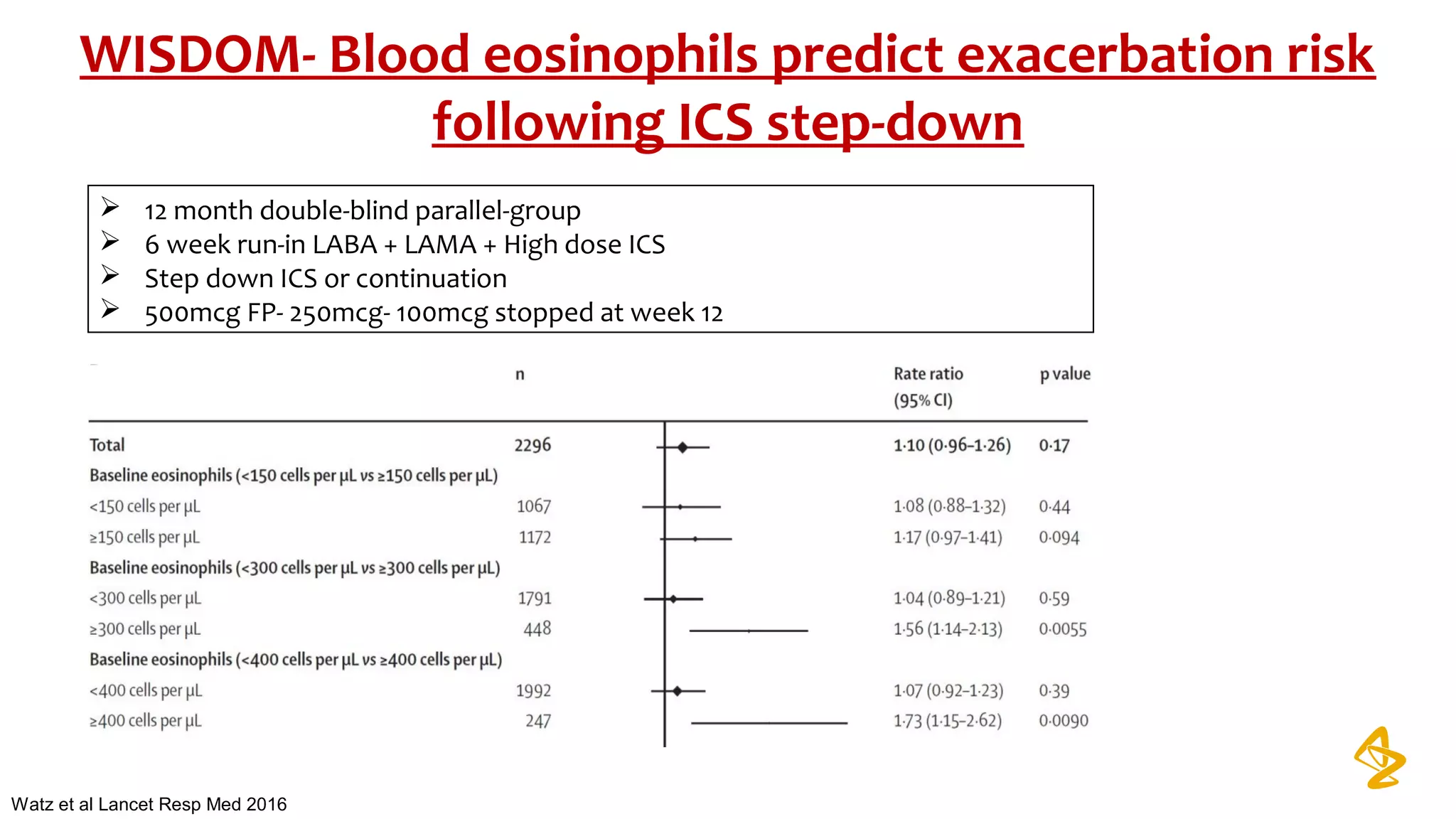
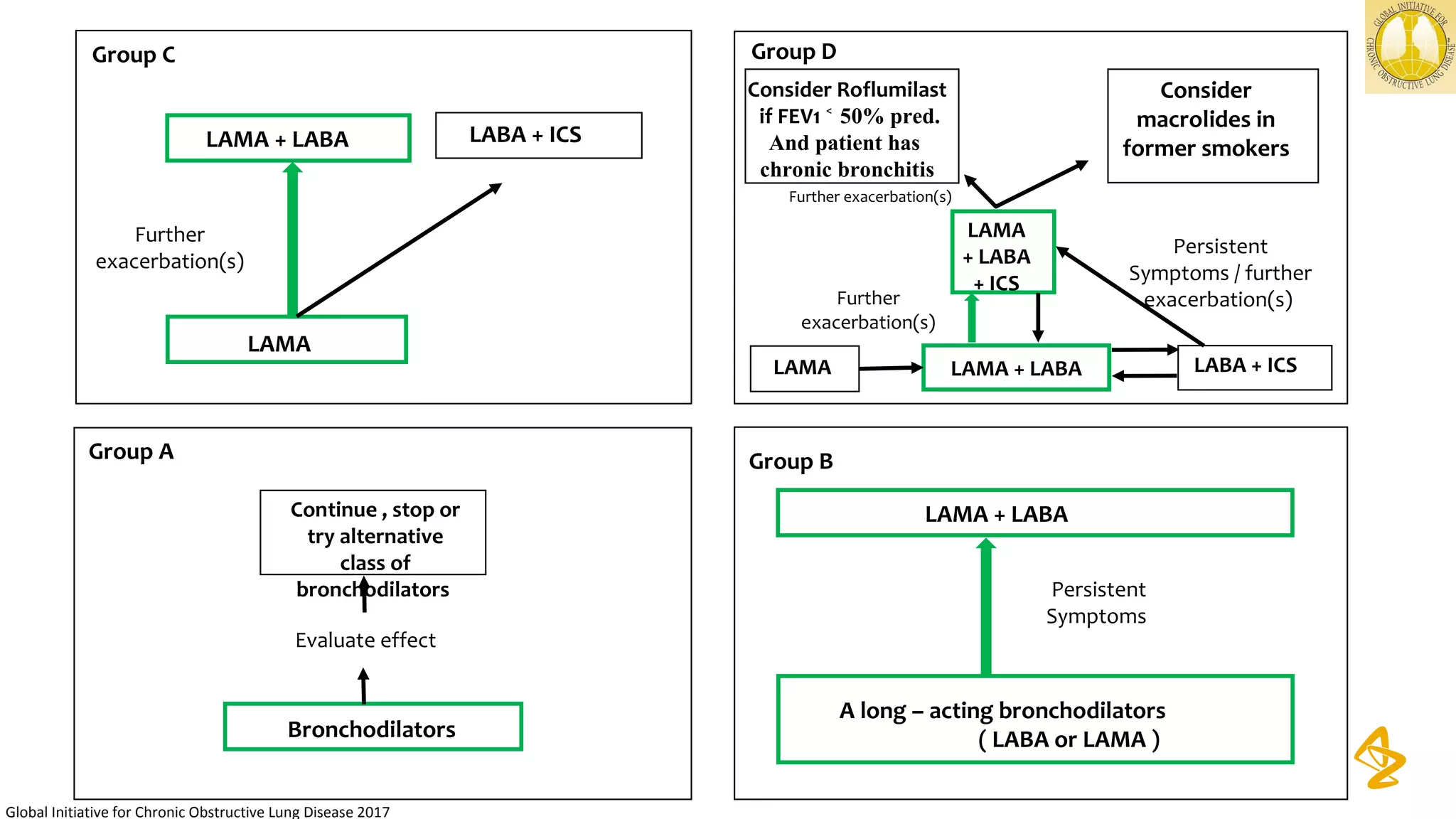
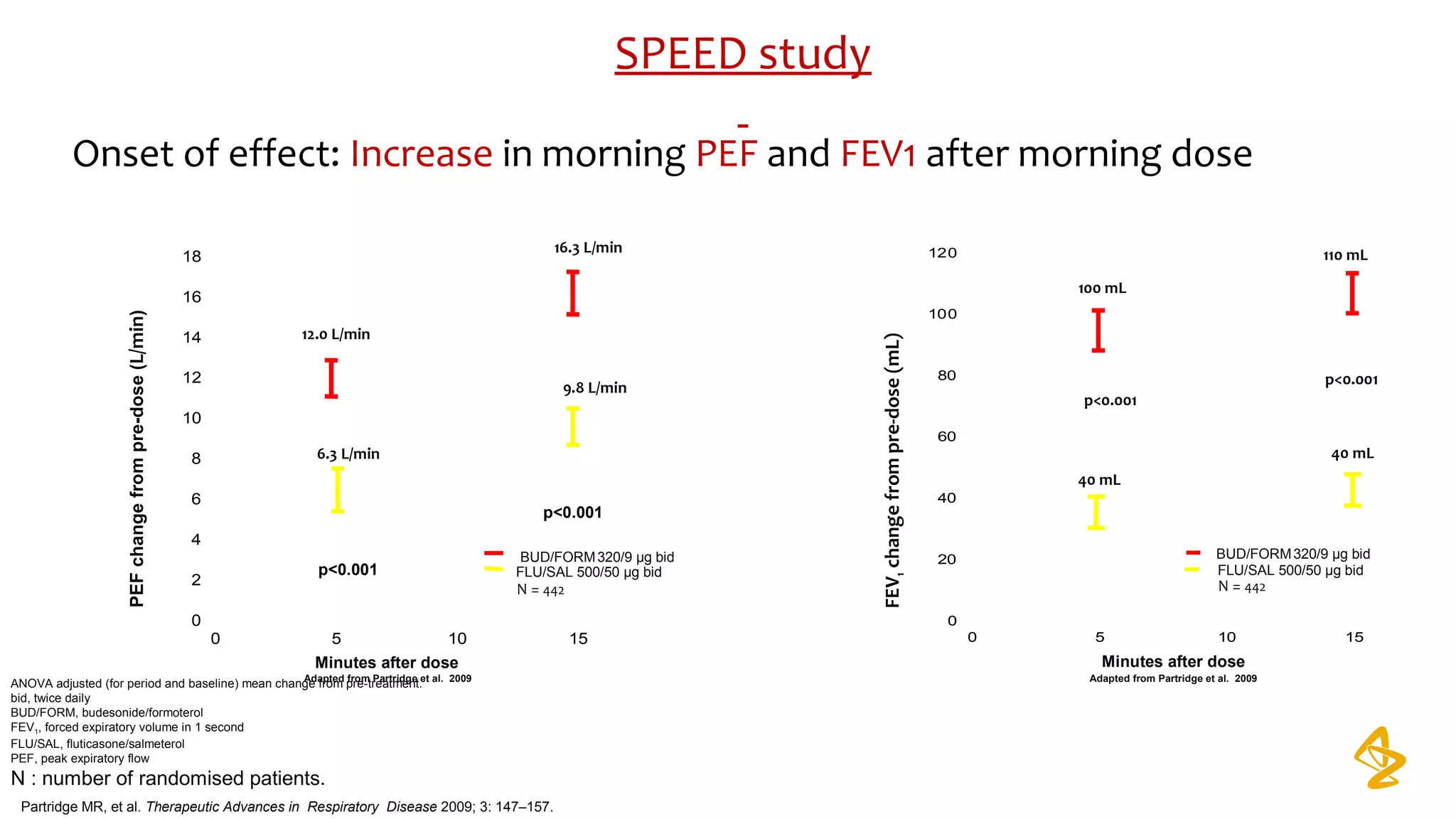
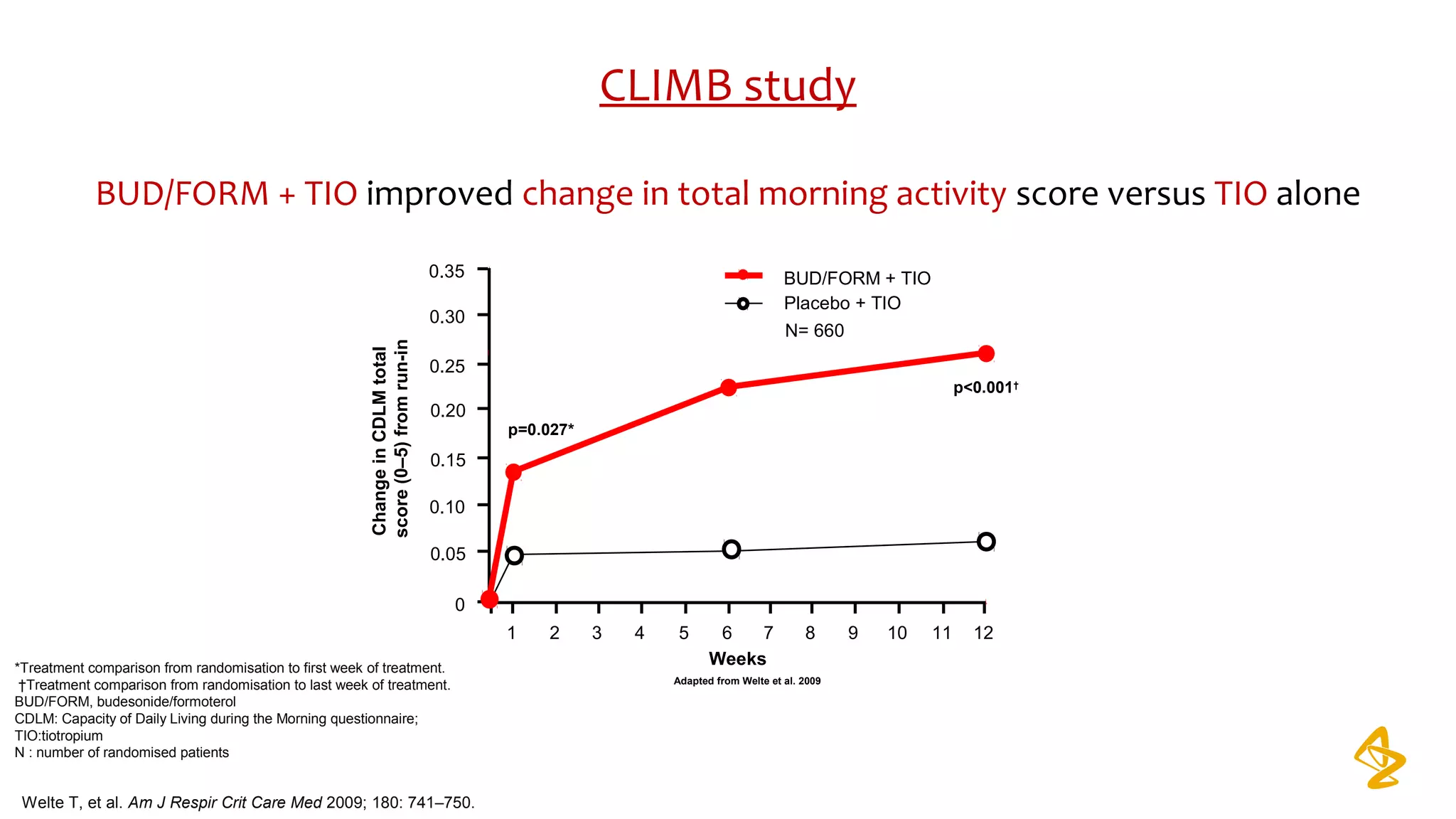
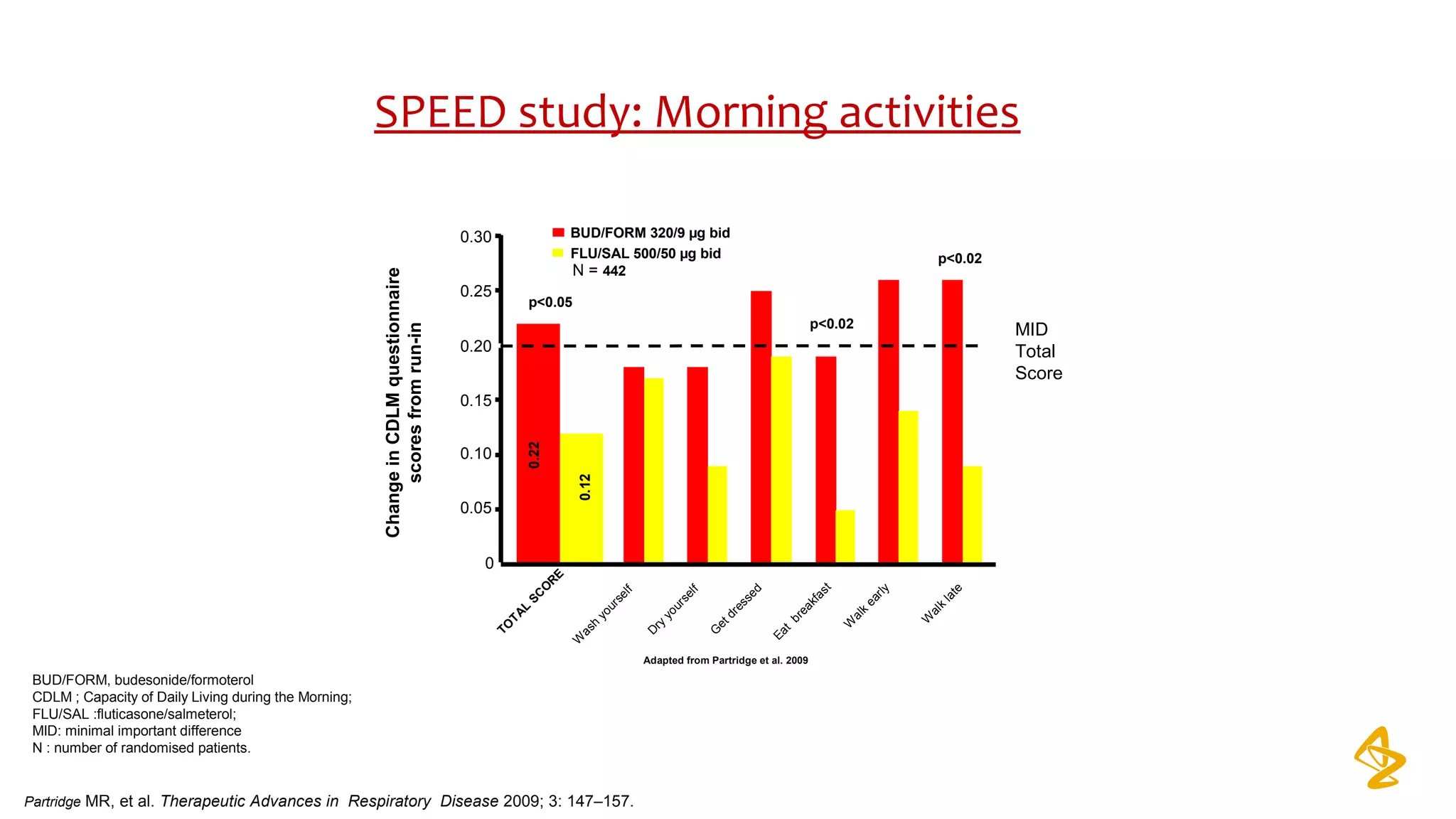
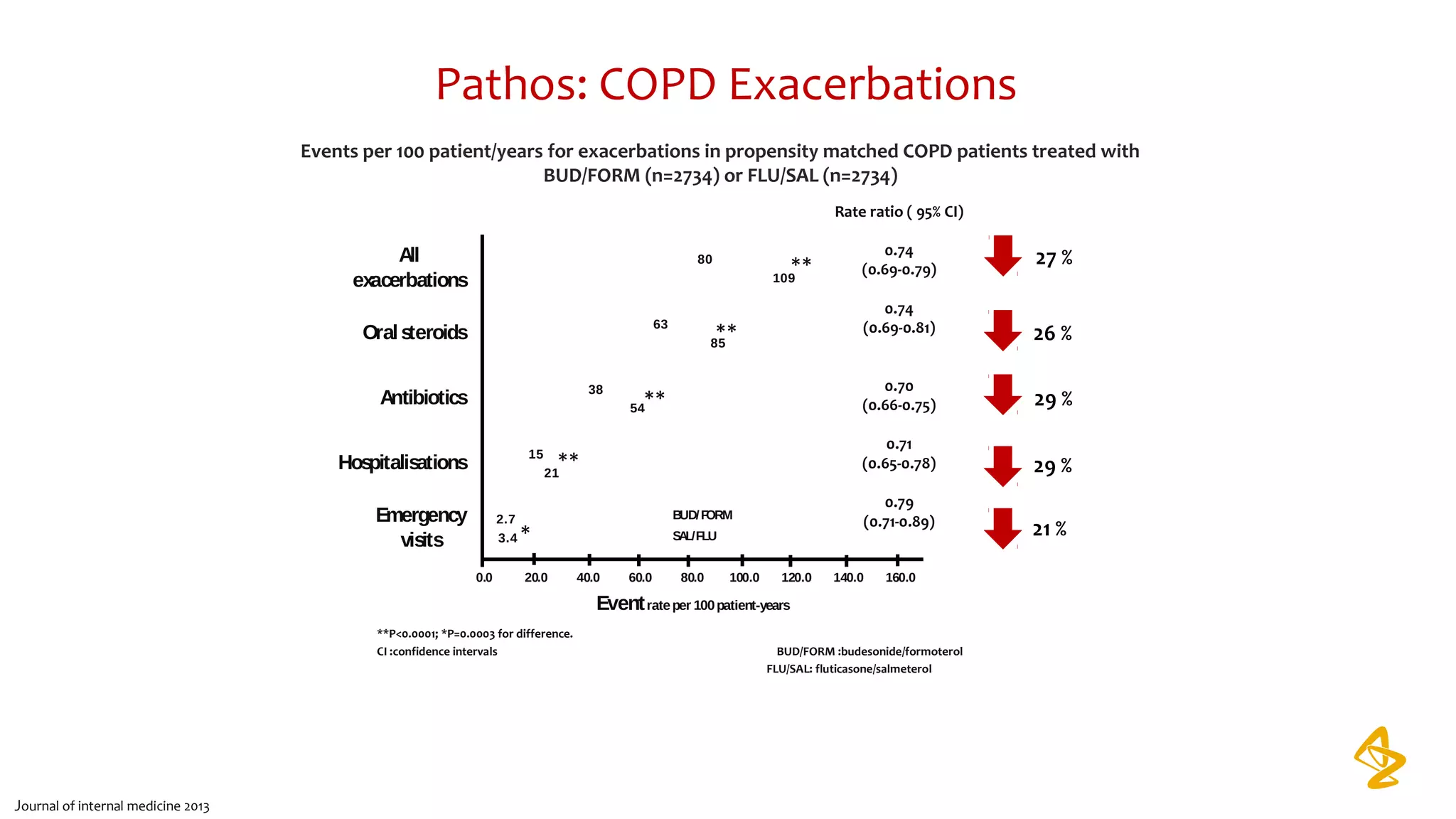
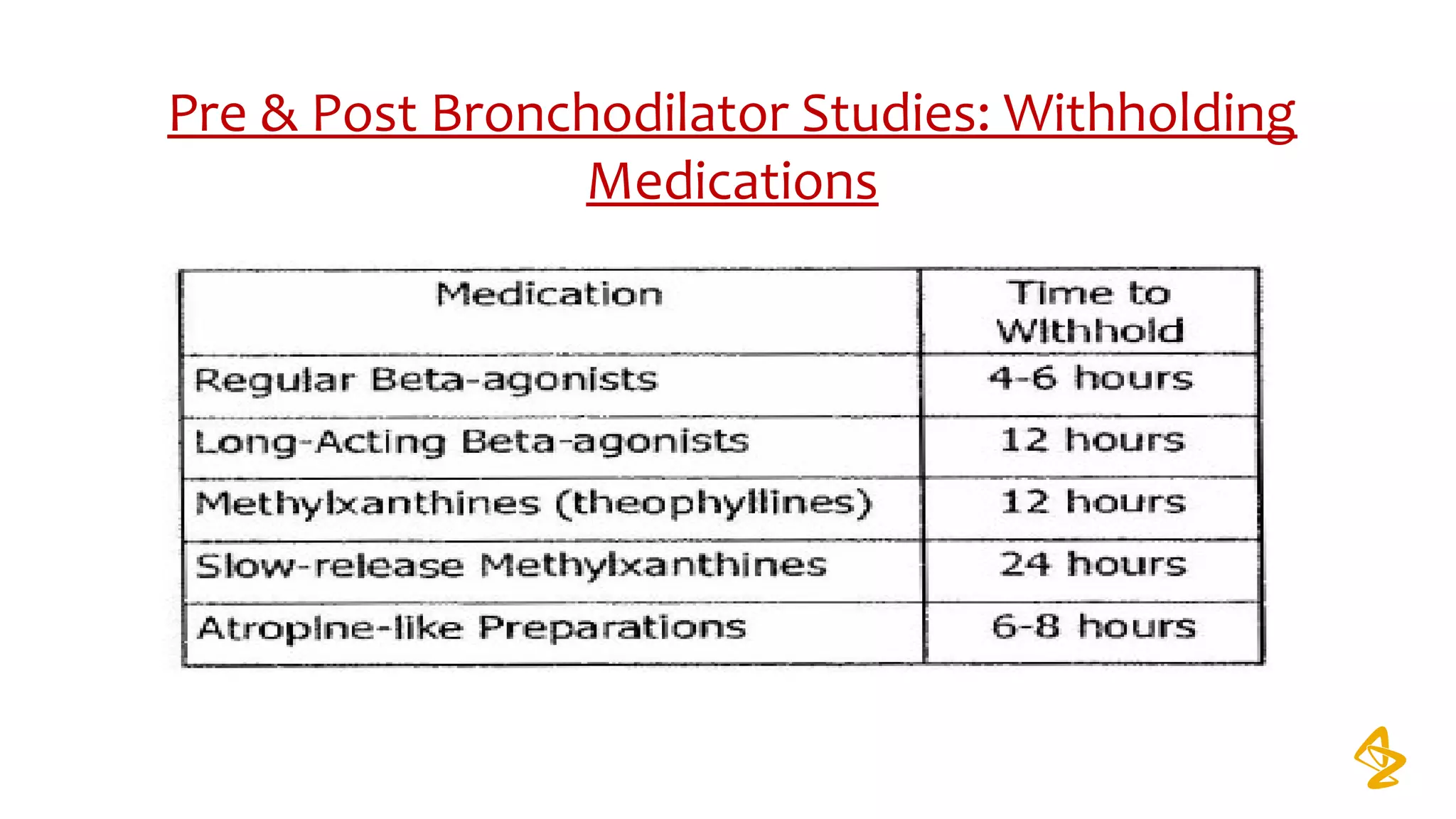
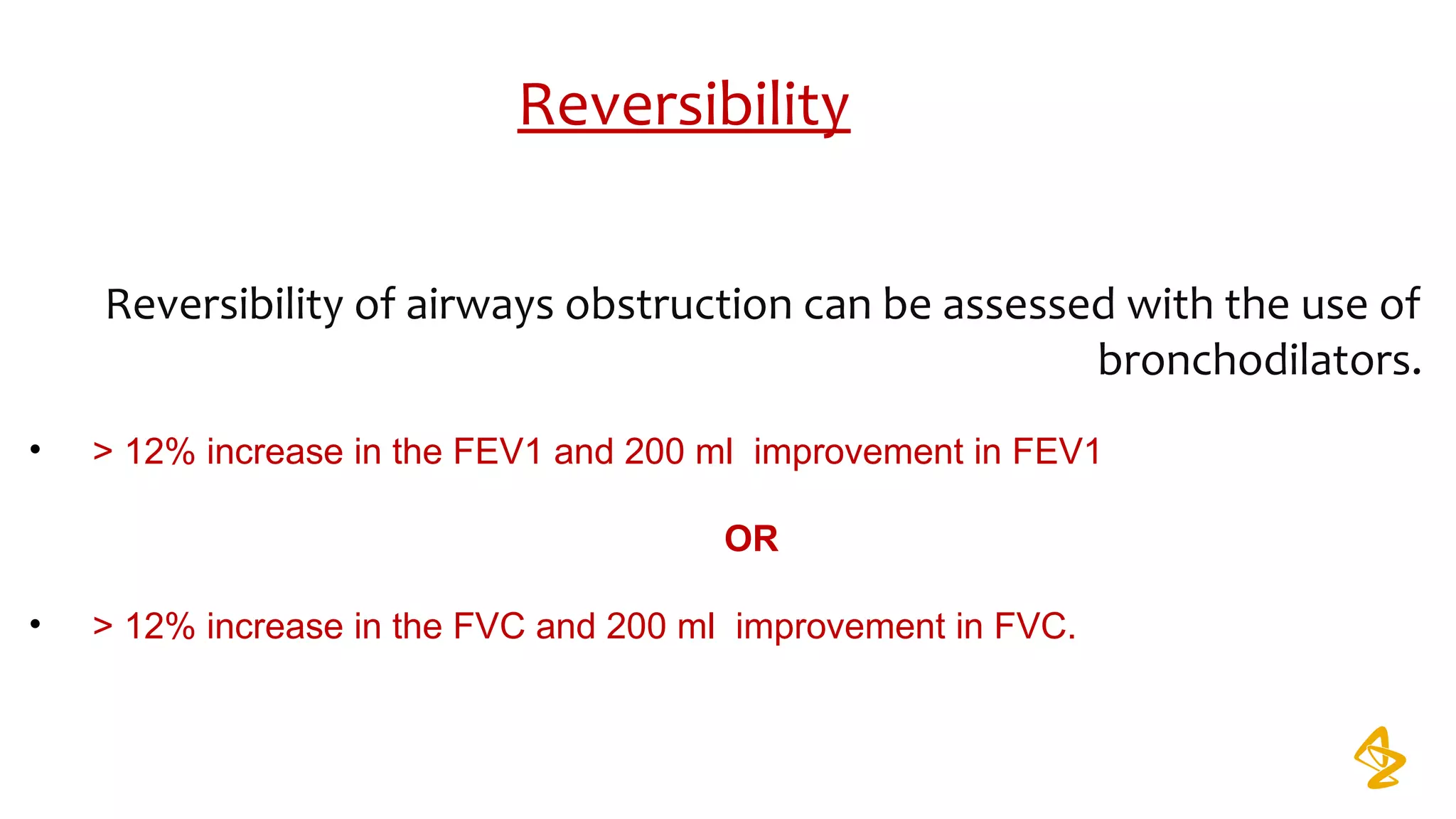
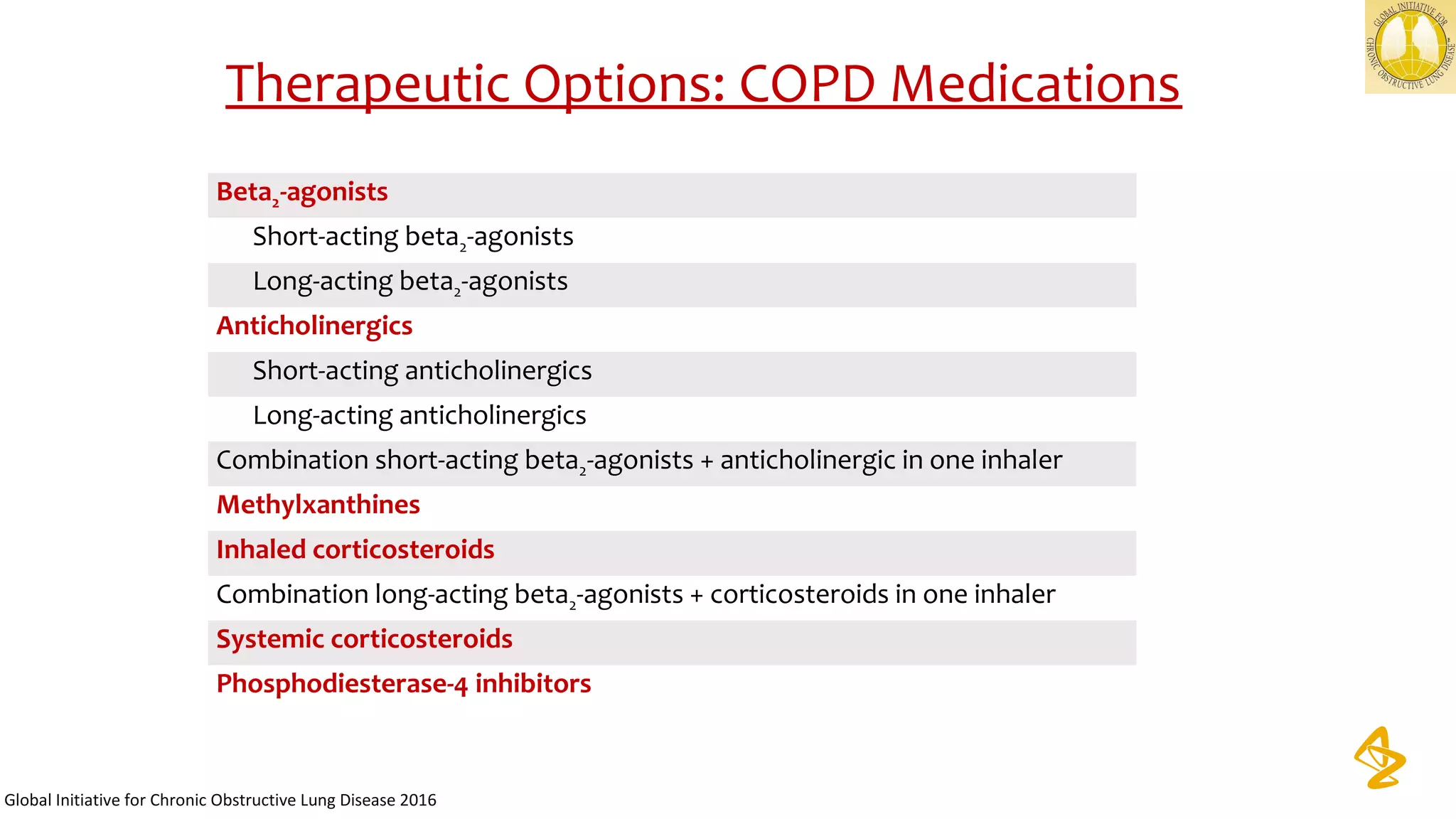
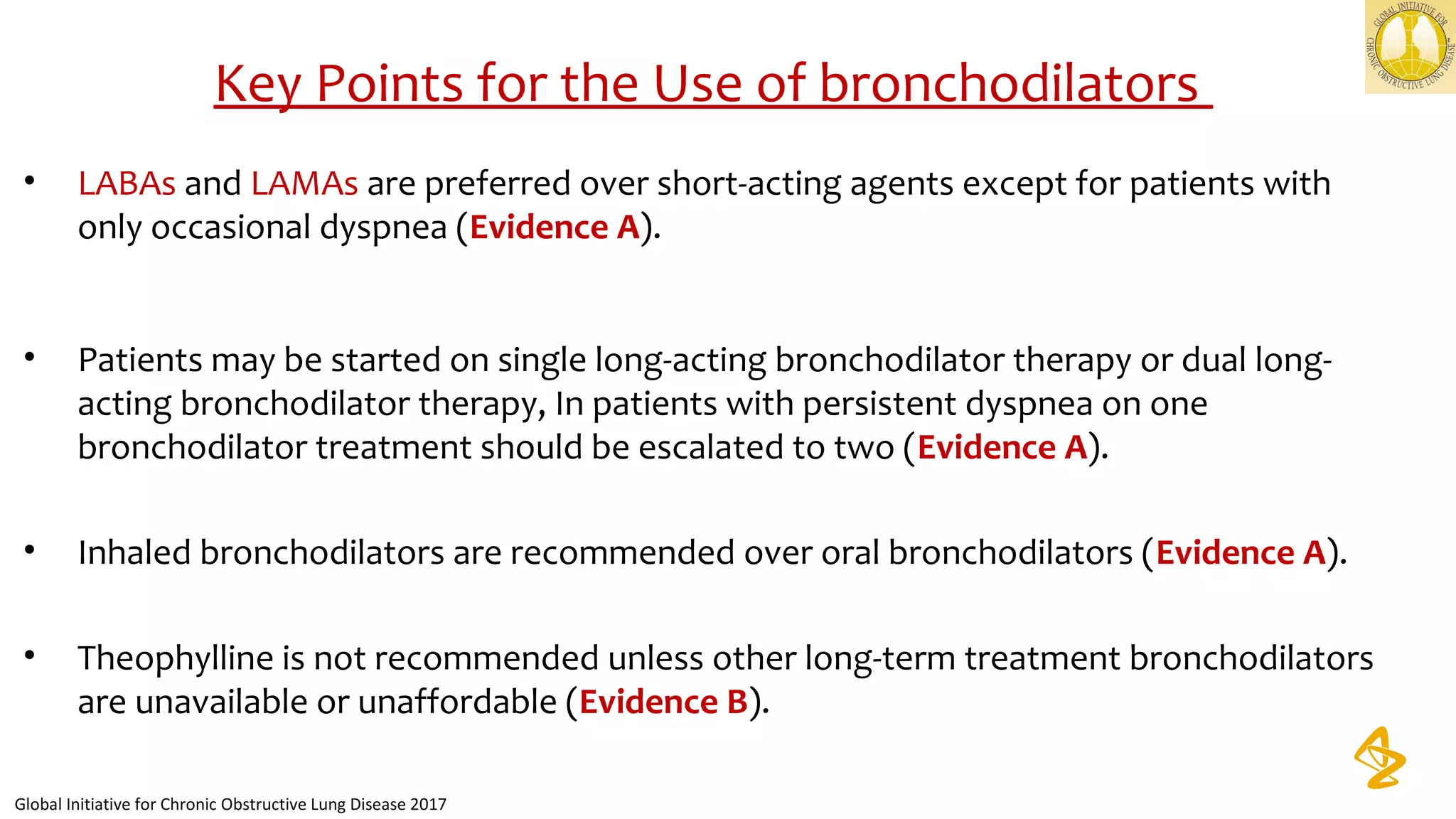
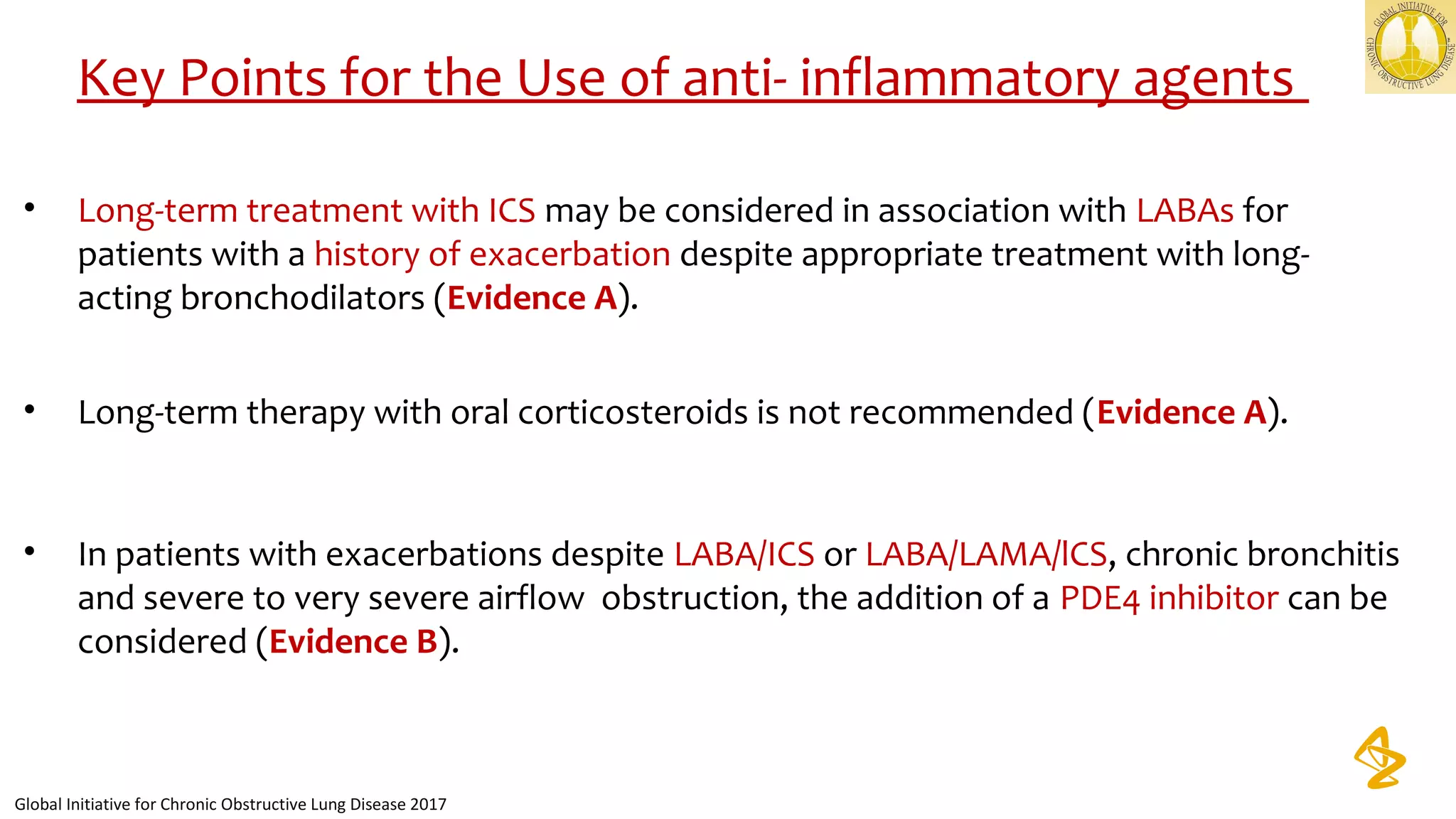
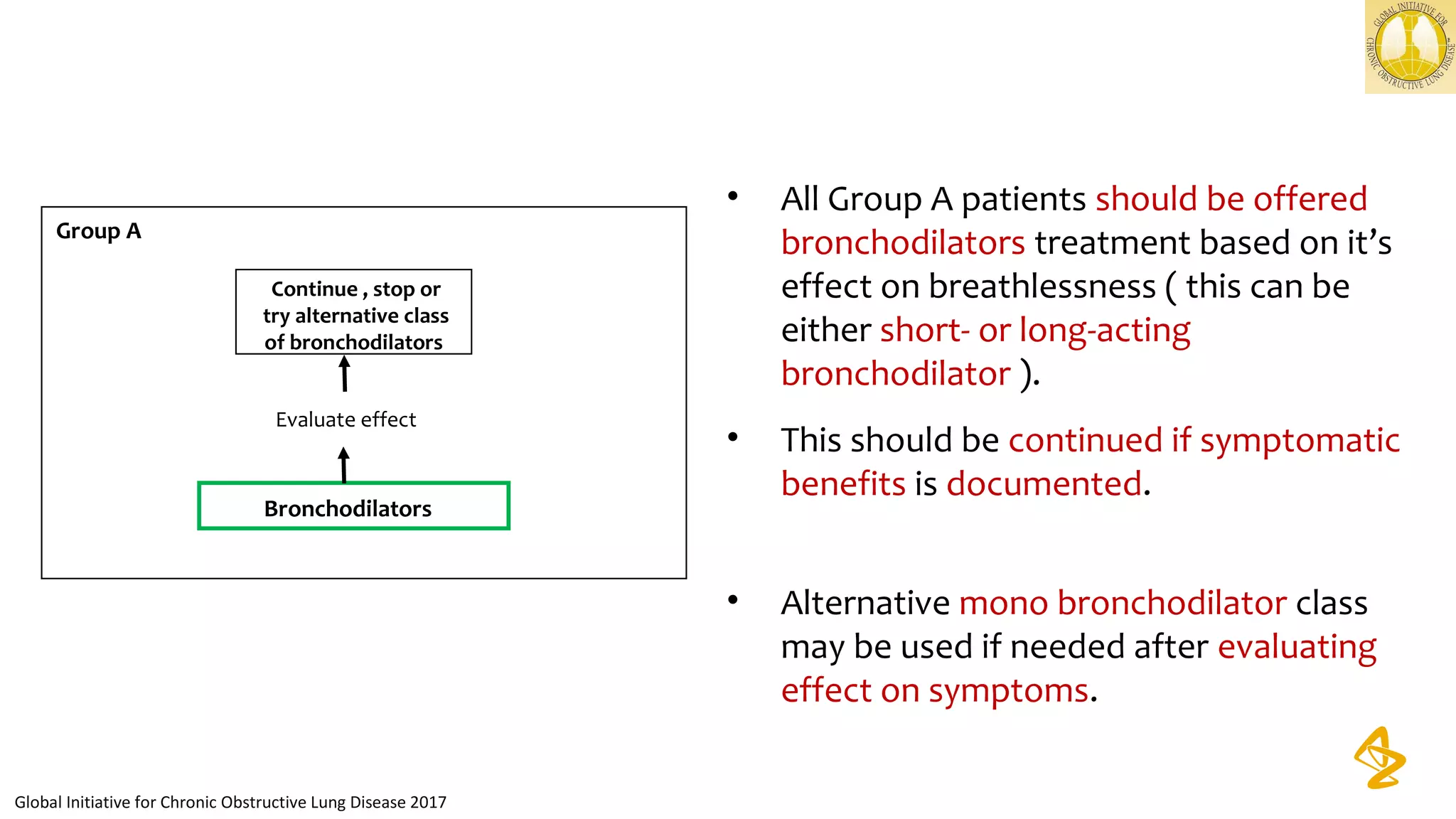
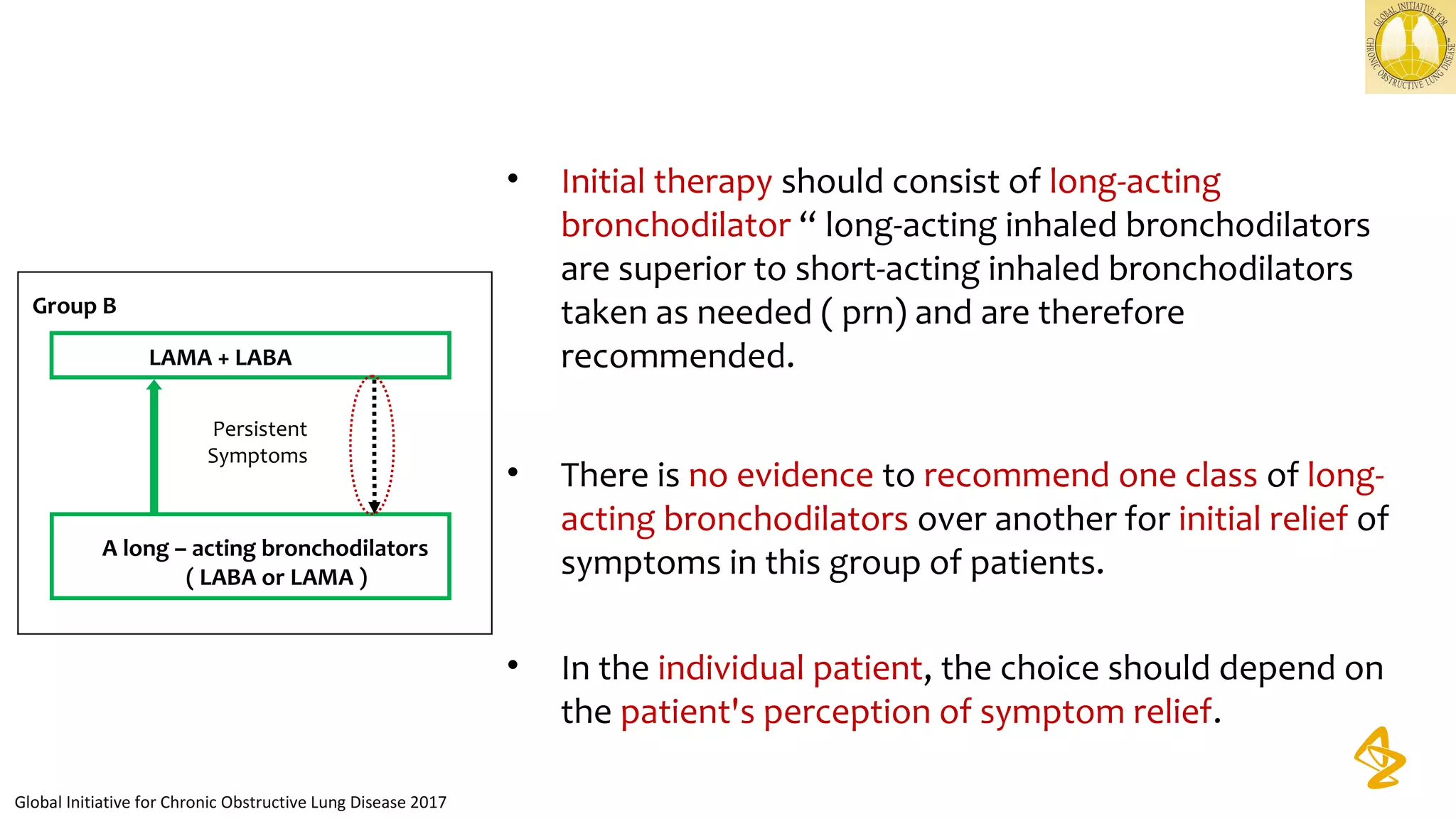
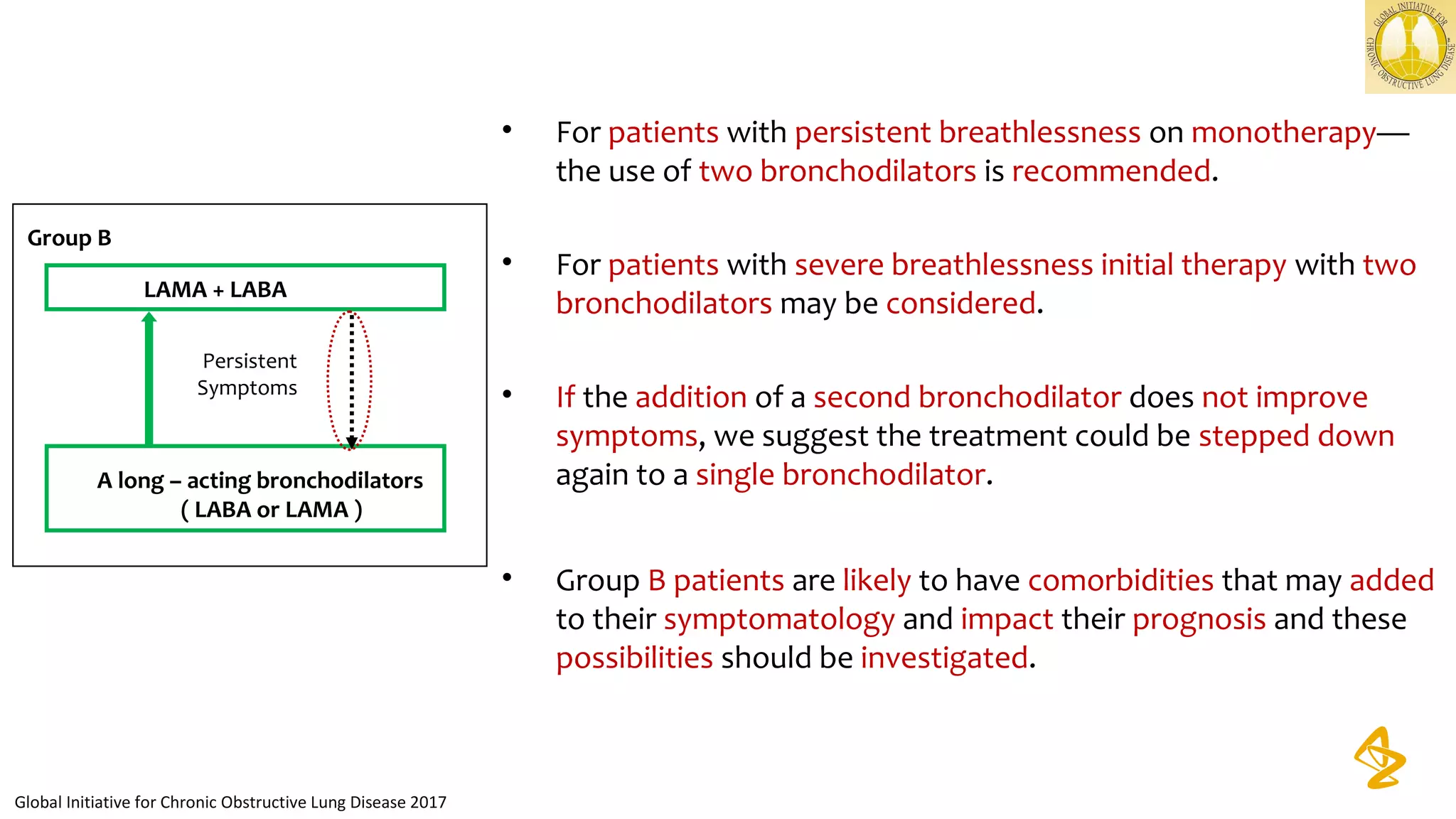
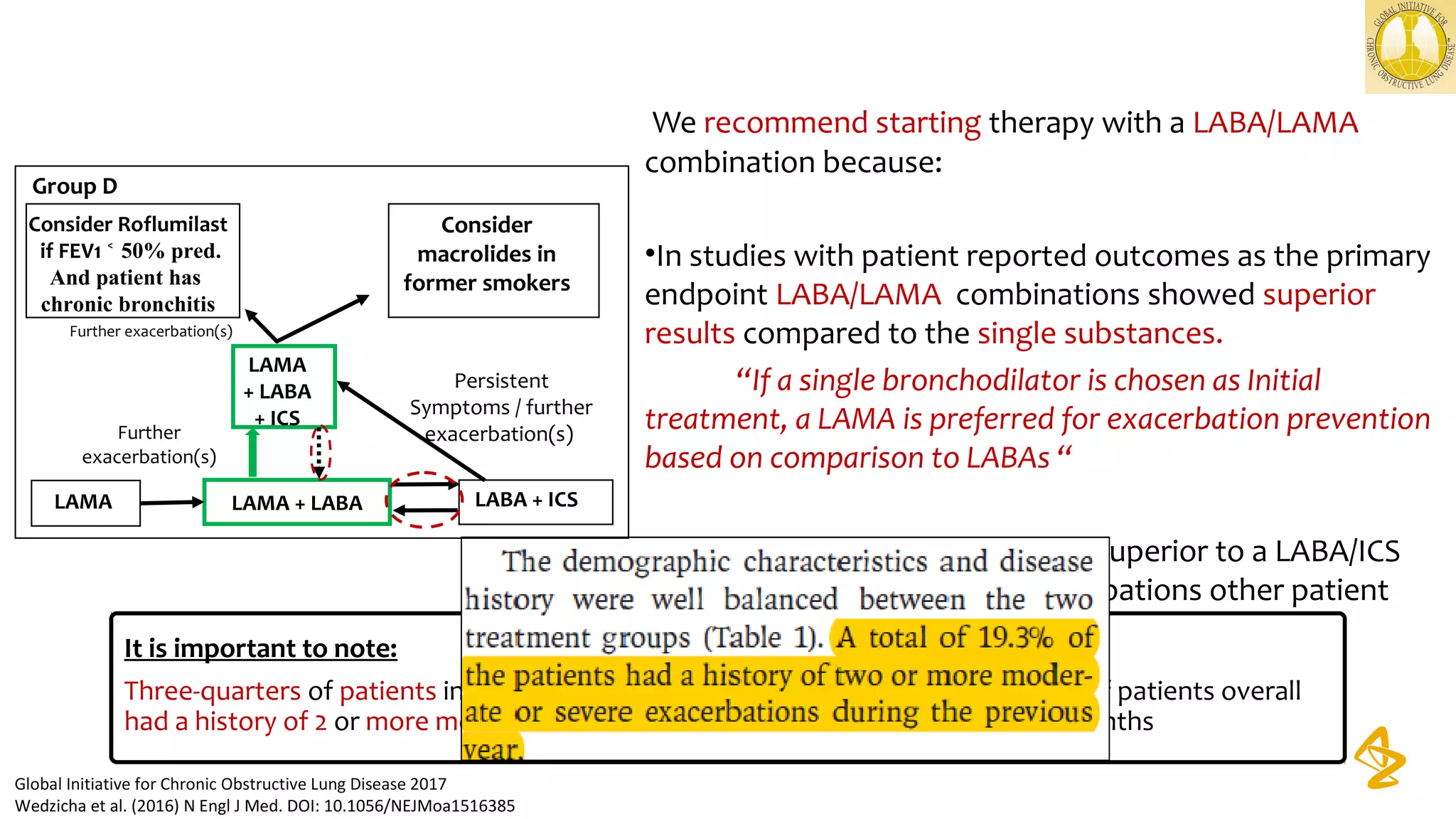
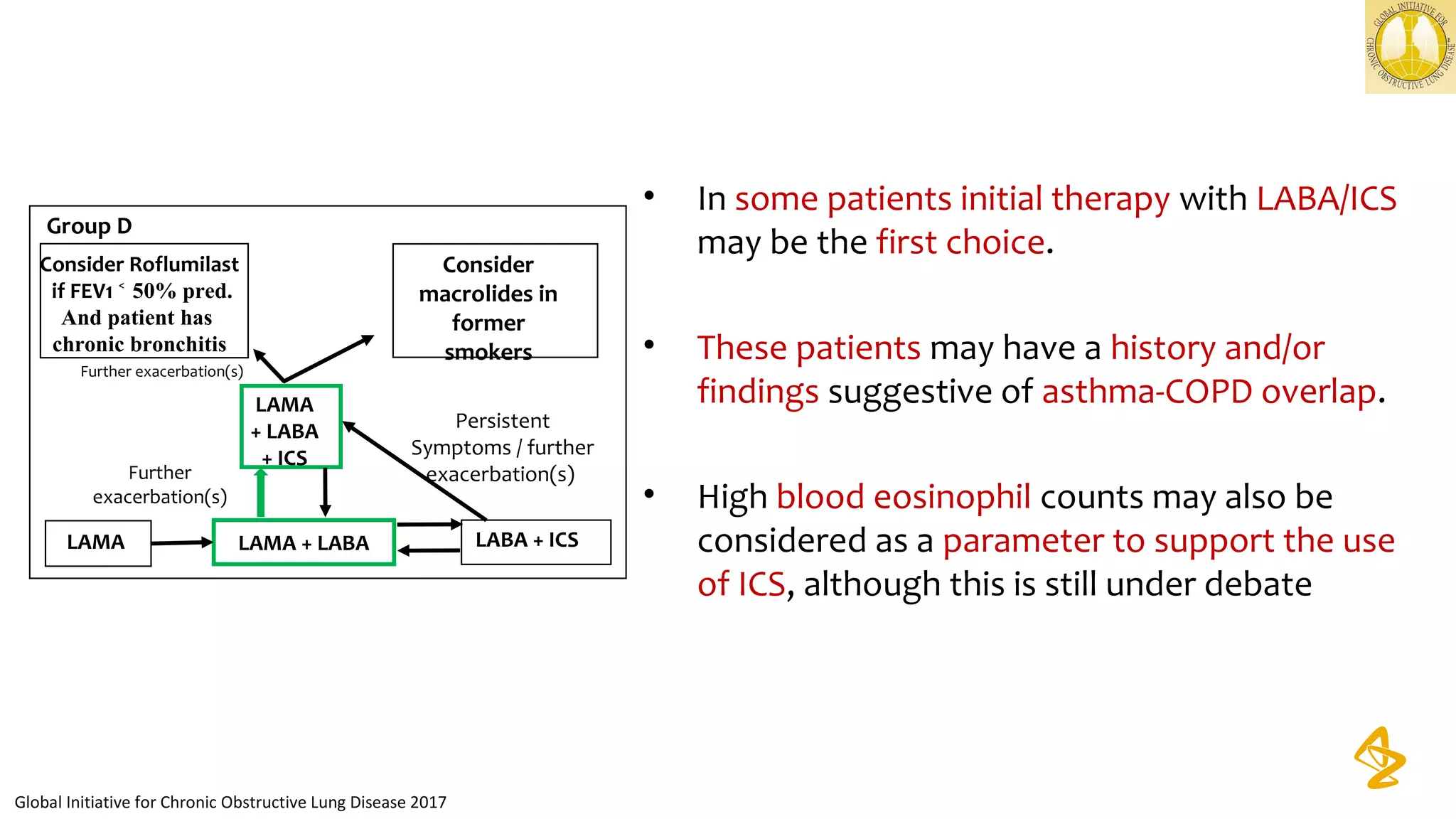
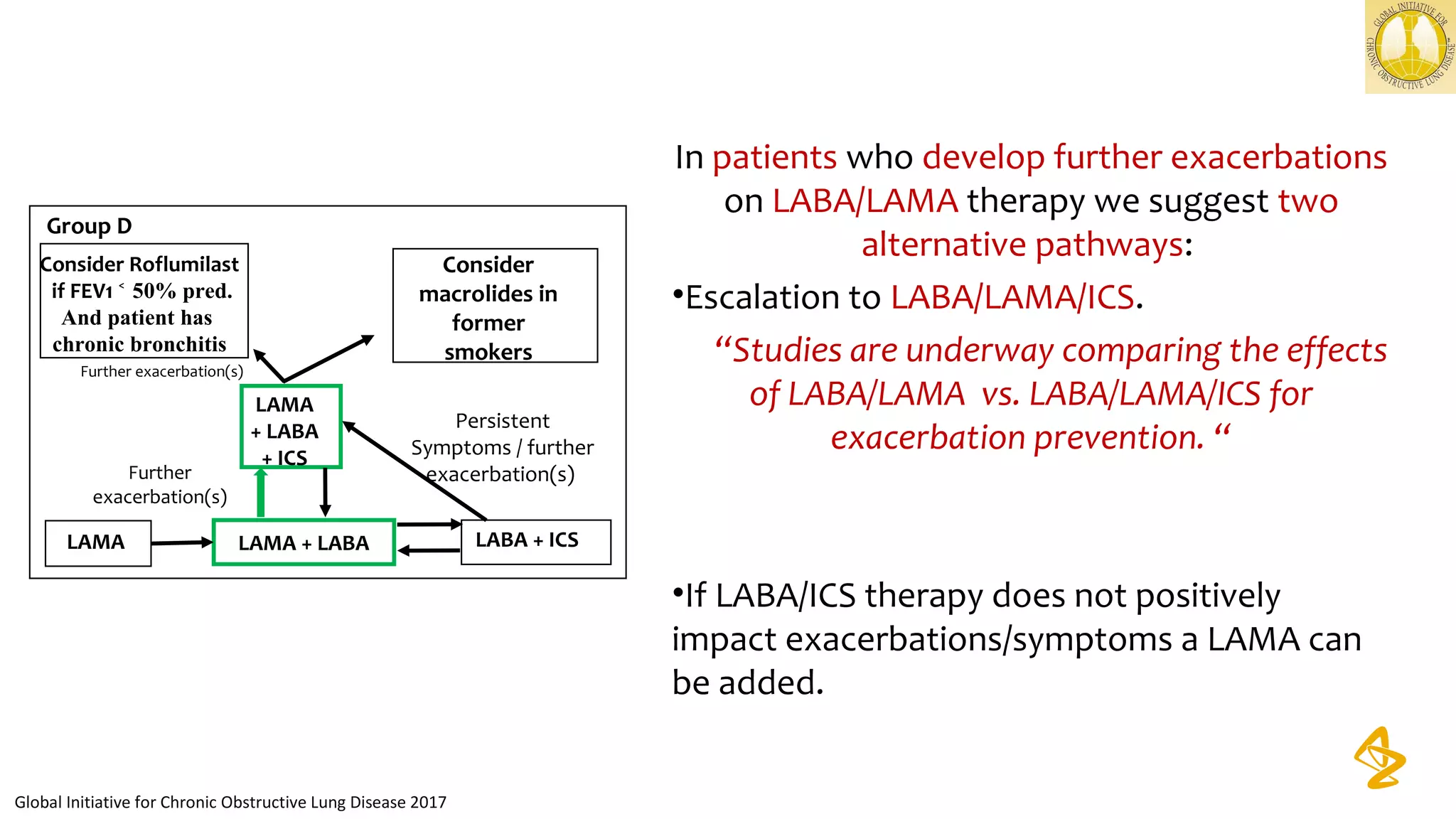
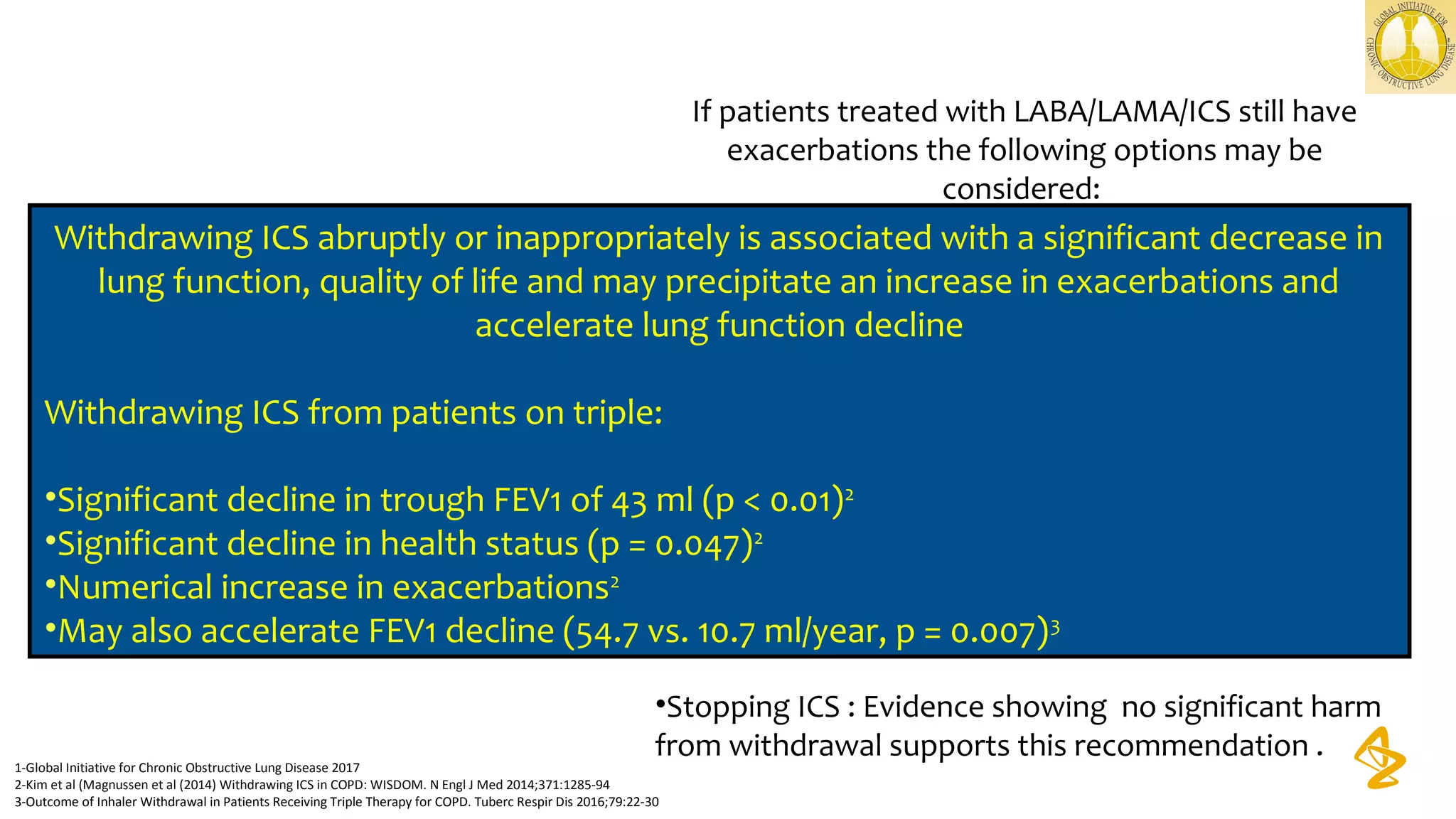
3) Treatment options discussed include short and long-acting bronchodilators, inhaled corticosteroids, phosphodiesterase inhibitors, and systemic corticosteroids. Combination inhalers containing bronchodilators with inhaled corticosteroids are preferred options.
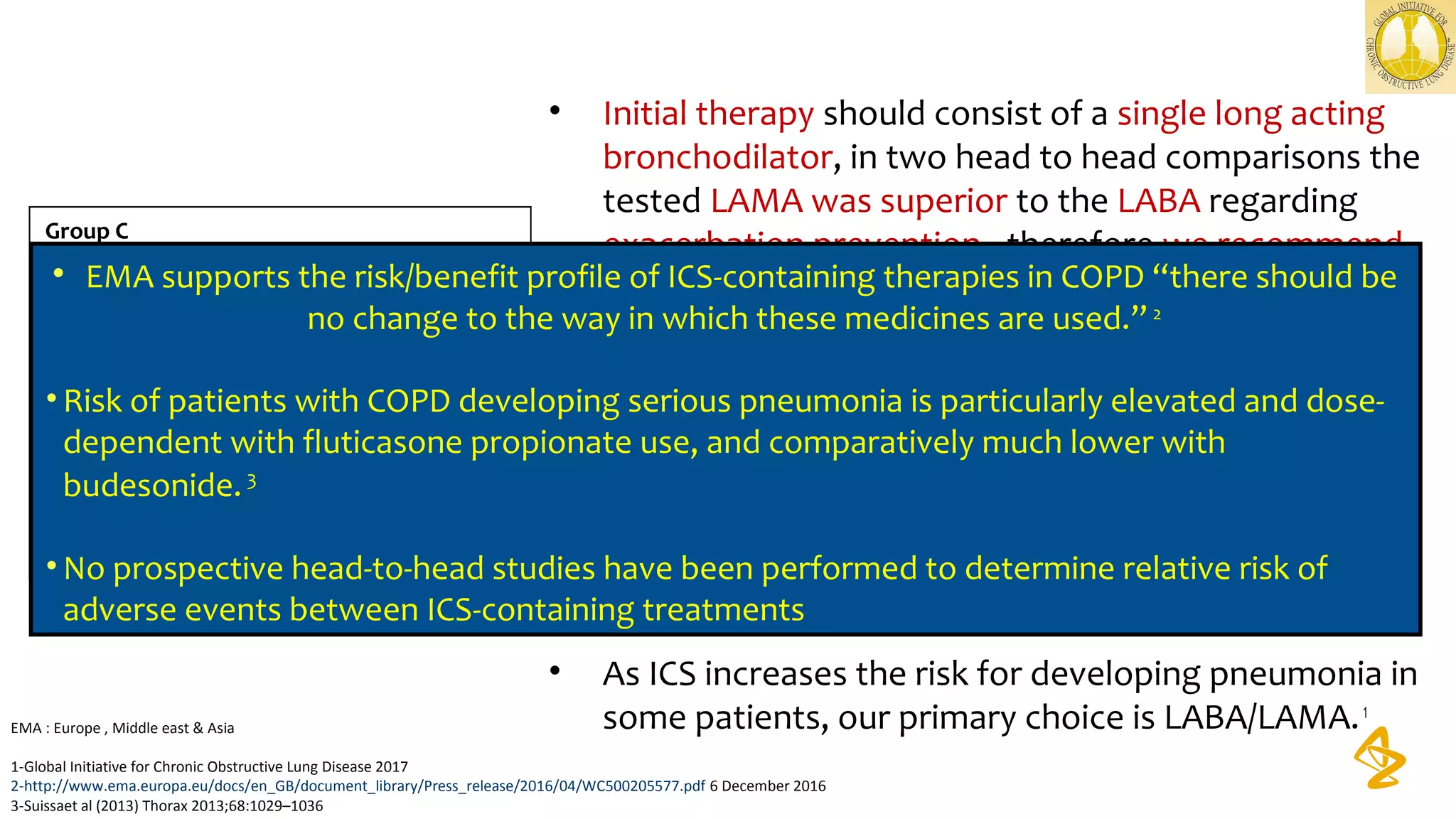
![Phenotype Infrequent exacerbator ACOS
Exacerbator with
emphysema
Exacerbator with chronic
bronchitis
Treatment strategy* Bronchodilators
Bronchodilators
+ ICS
Bronchodilators
(in some cases + ICS)
Bronchodilators
+ ICS
No Yes
ACOS? ACOS?
No Yes NoYes
Chronic cough?
YesNo
Diagnosis of COPD and ≥2 exacerbations per year?
*Choice of treatment should be based on clinical phenotype and the intensity determined by severity
• *Choice of treatment should be based on clinical phenotype and the intensity determined by severity
• ACOS = asthma COPD overlap syndrome; GesEPOC = Guía Española de la EPOC [Spanish Guidelines for COPD]; ICS = inhaled corticosteroid‒
Miravitlles M, et al. Arch Bronconeumol 2012
Characterization of patients with COPD: GesEPOC](https://image.slidesharecdn.com/essbfinalpresentation8december2017final-161209151928/75/Role-of-Inhaled-Corticosteroids-in-COPD-60-2048.jpg)