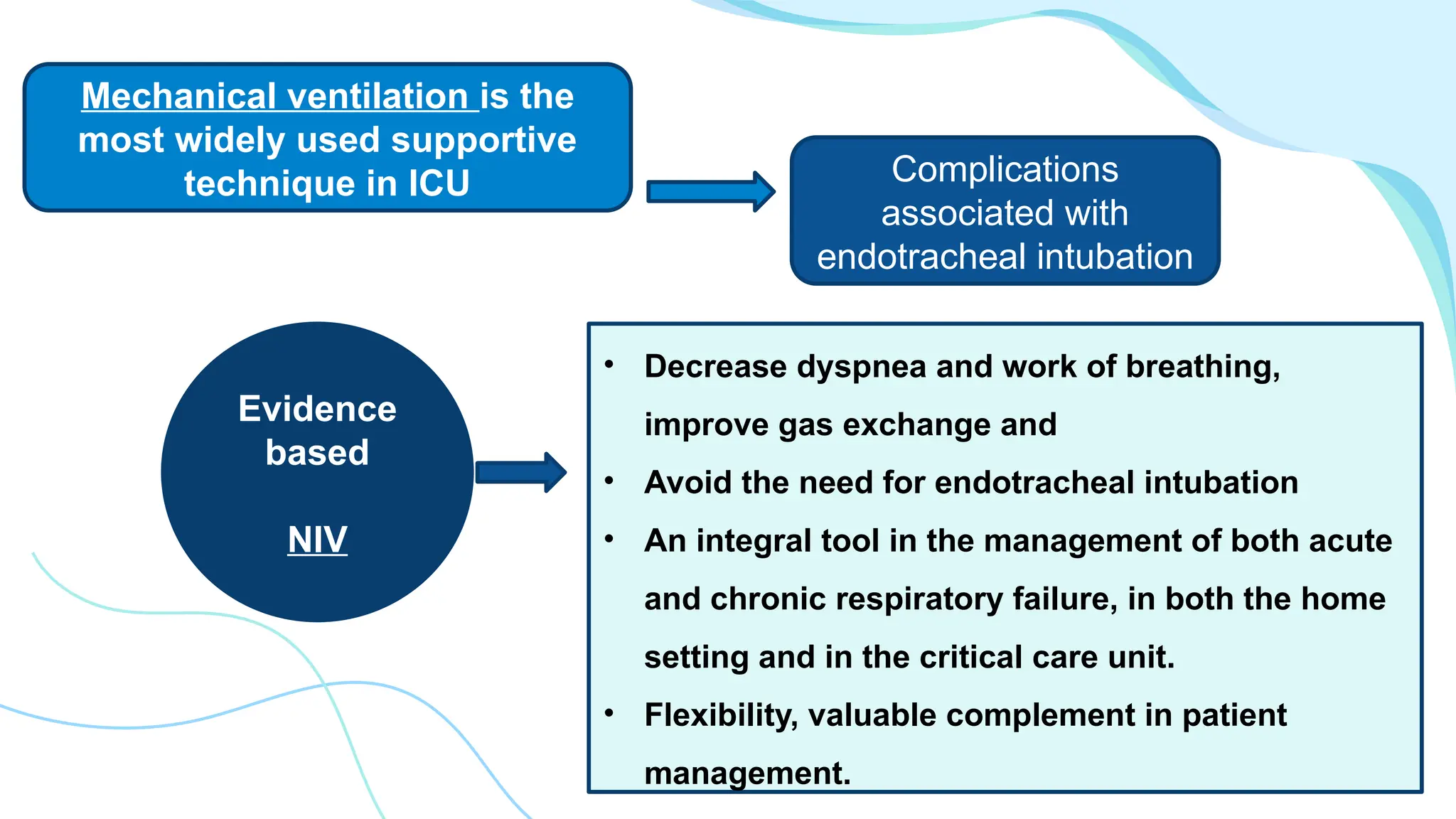
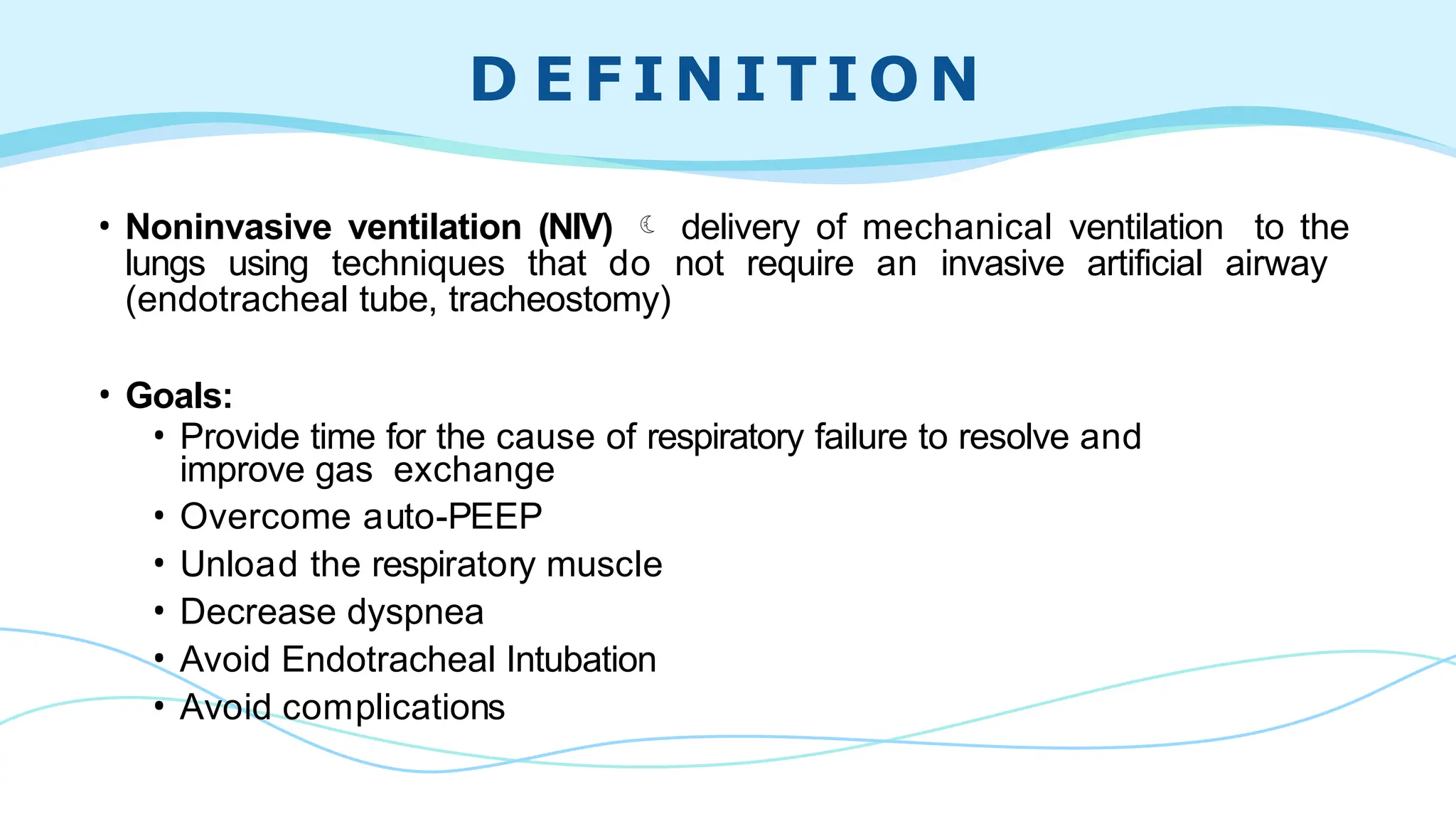
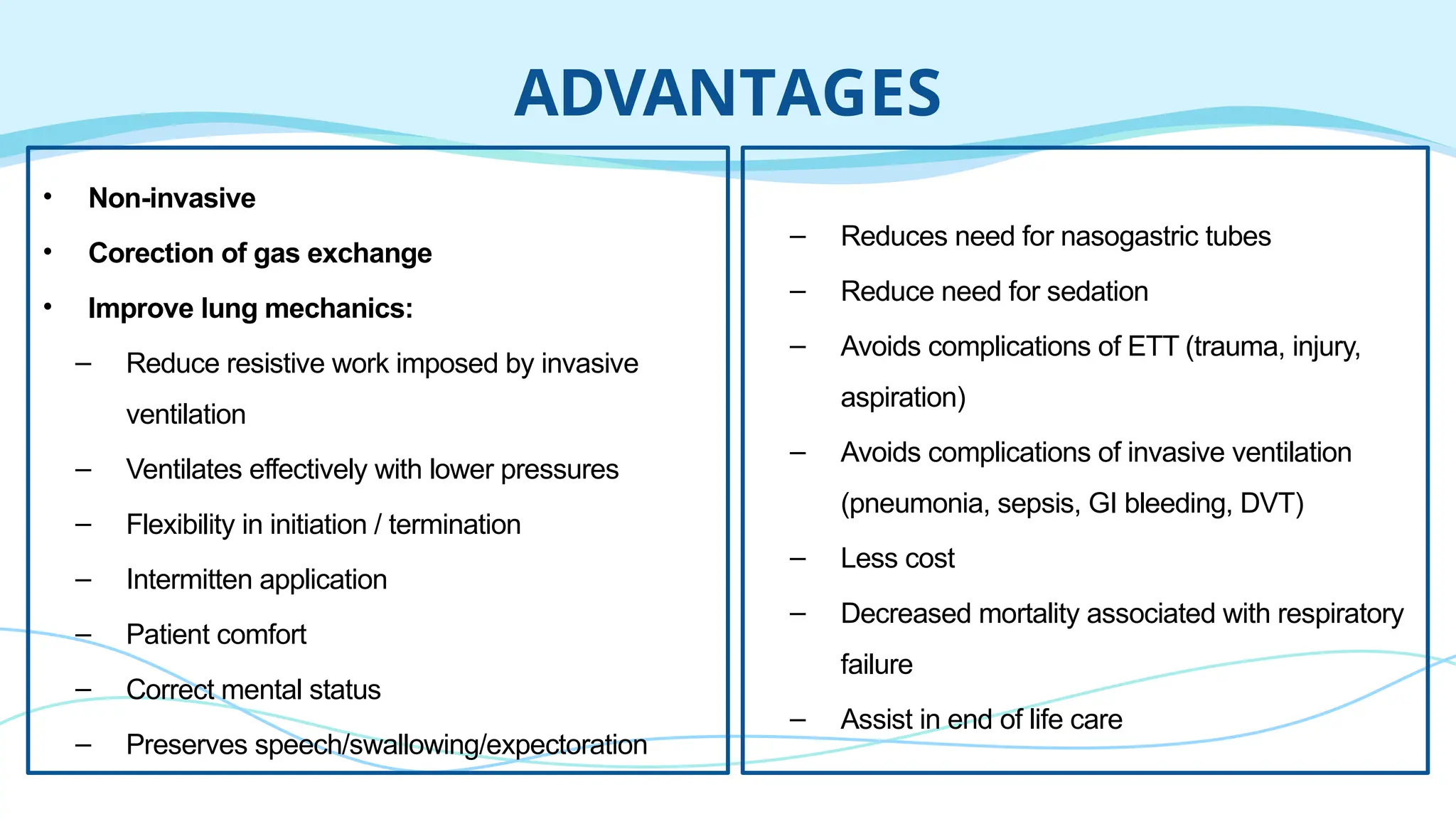
The document discusses non-invasive ventilation (NIV) as a supportive treatment for patients with respiratory failure, detailing its mechanisms, advantages, and types such as CPAP and BiPAP. It highlights the goals of NIV, its application in various acute respiratory conditions, and the criteria for patient selection, as well as the potential complications and contraindications. The findings emphasize NIV's effectiveness in improving respiratory function while minimizing the risks associated with invasive mechanical ventilation.