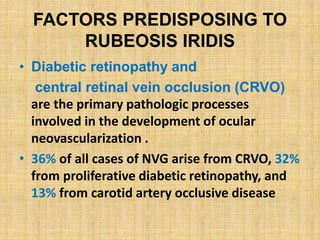
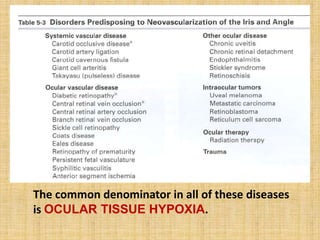
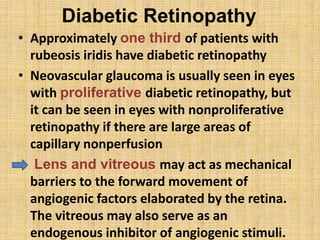
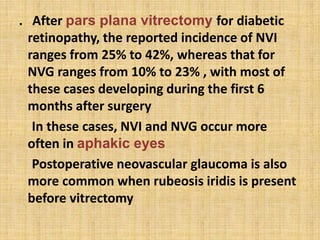
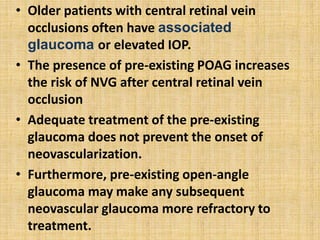
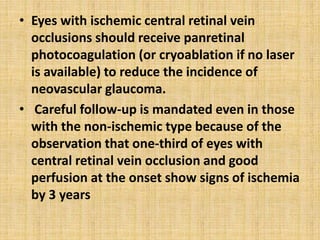
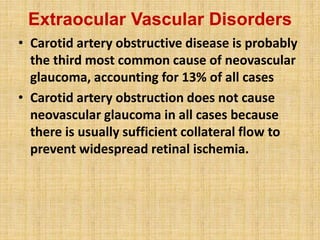
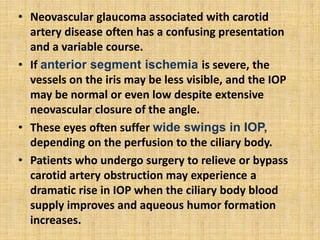
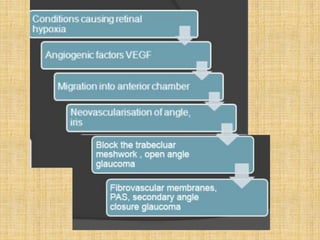
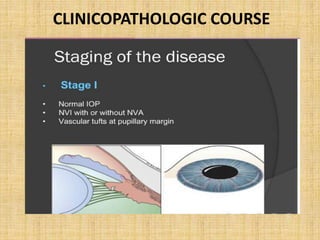
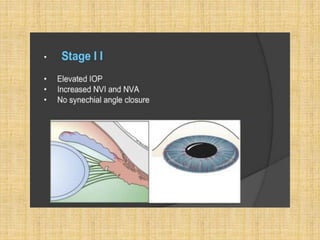
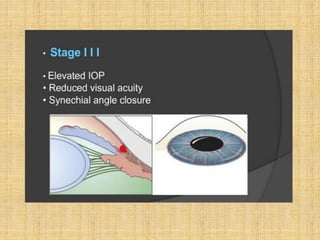
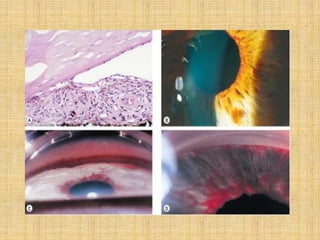
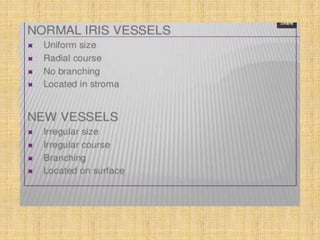
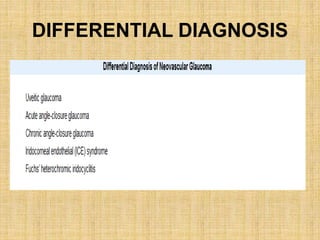
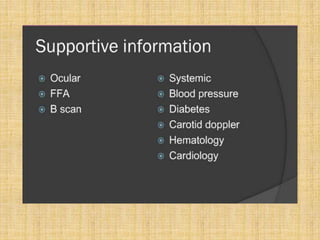
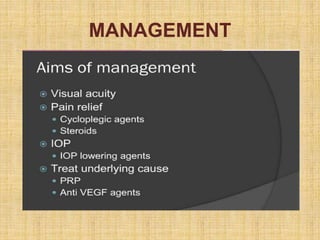
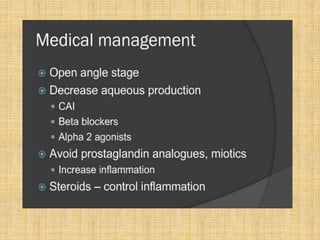
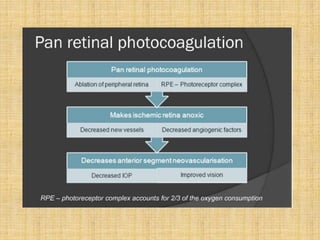
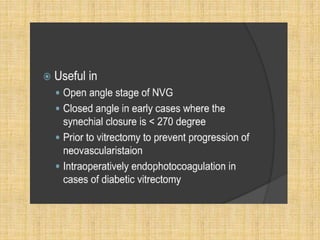
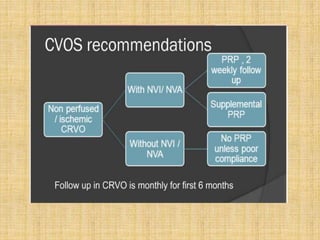
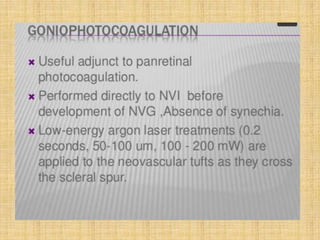
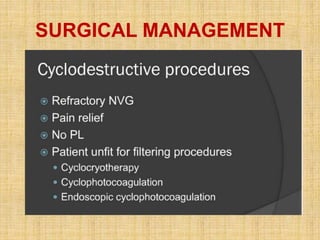
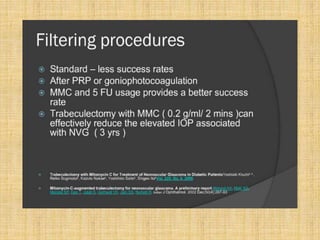
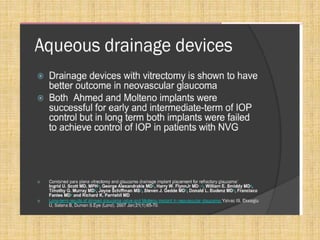
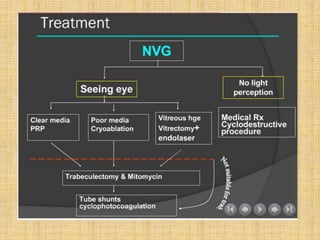
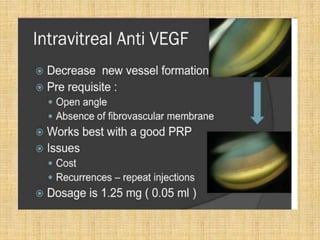
This document discusses neovascular glaucoma, also known as rubeotic glaucoma. It begins by defining the terminology and describing the clinical features. The main causes of neovascular glaucoma are diabetic retinopathy, central retinal vein occlusion, and carotid artery occlusive disease, all of which result in ocular tissue hypoxia. This hypoxia leads to the release of angiogenic factors like vascular endothelial growth factor that induce new blood vessel growth on the iris and in the anterior chamber angle, causing glaucoma. Later sections discuss theories of neovasculogenesis, angiogenic and vasoinhibitory factors, clinical course, differential diagnosis, medical management, and surgical options.