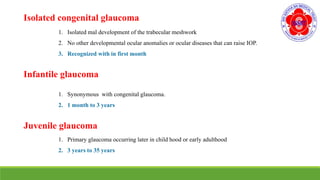
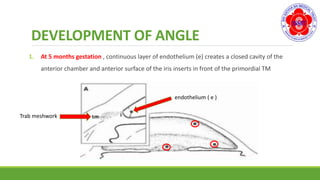
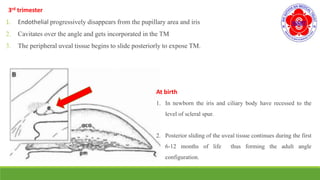
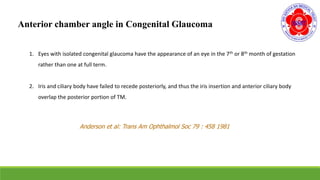
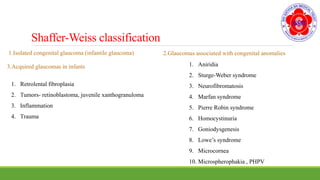
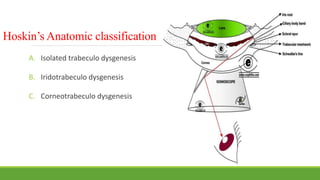
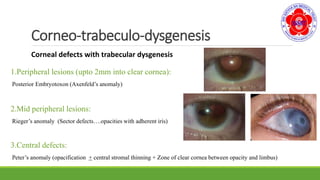
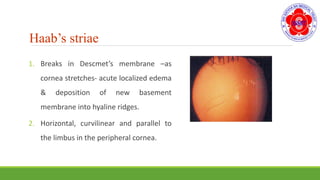
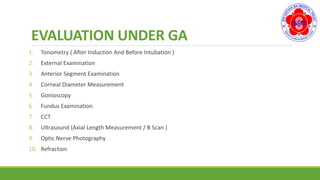
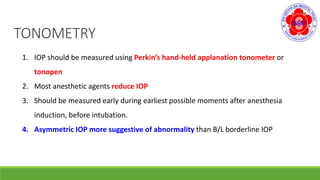
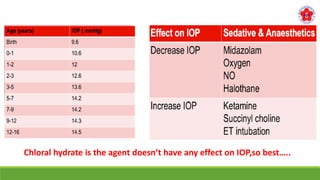
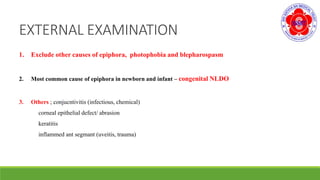
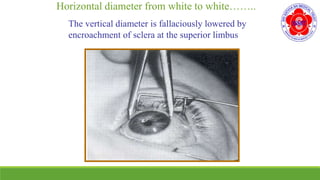
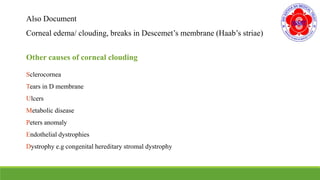
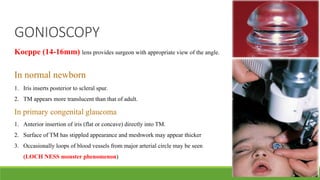
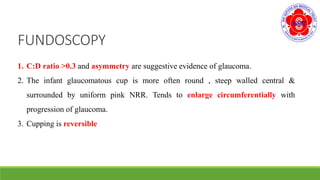
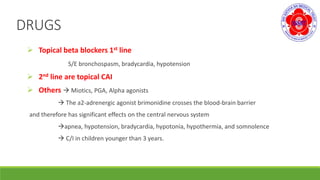
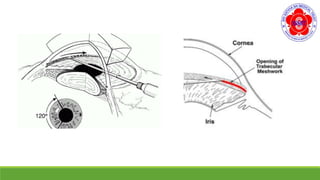
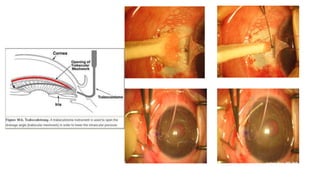
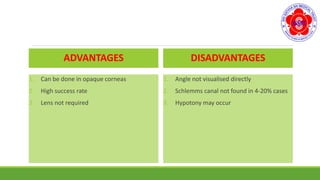
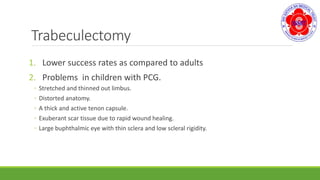
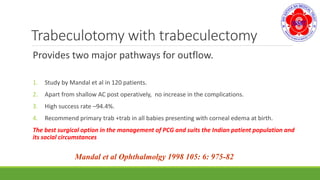
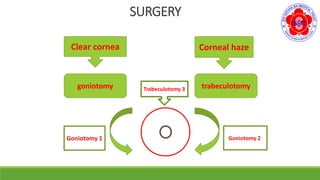
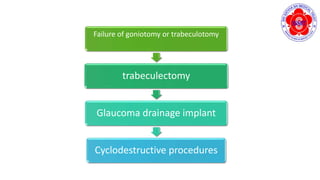
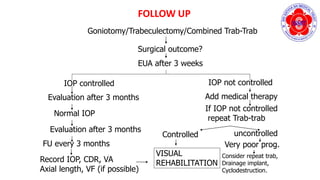
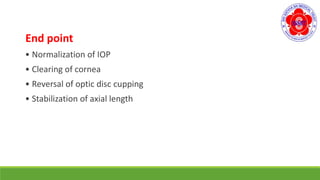
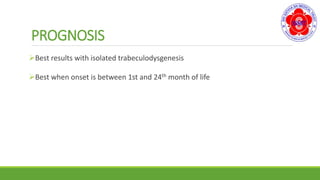
The document discusses congenital glaucoma, defining it as glaucoma present at birth associated with developmental anomalies of the eye. It covers the epidemiology, genetics, classification, pathogenesis, clinical features, evaluation, and management of congenital glaucoma. The main treatment involves surgical options like goniotomy, trabeculotomy, and trabeculectomy to lower intraocular pressure and clear the cornea.