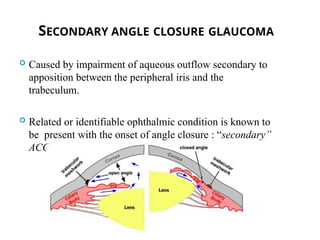
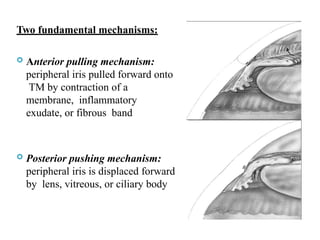
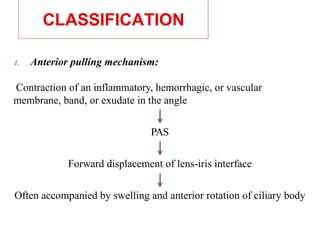
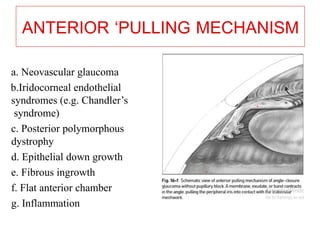
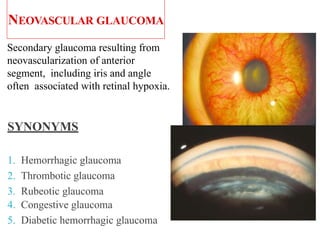
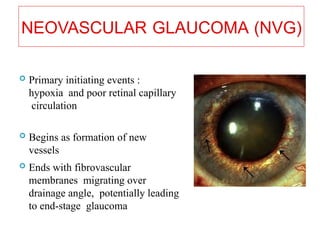
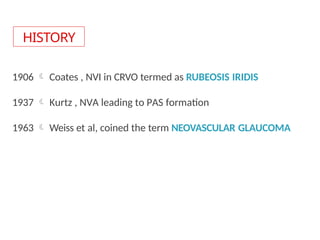
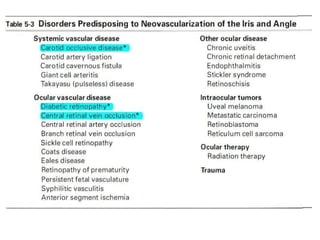
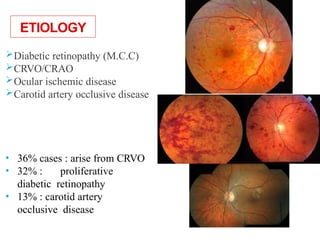
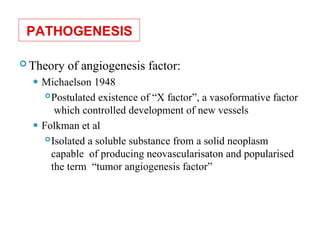
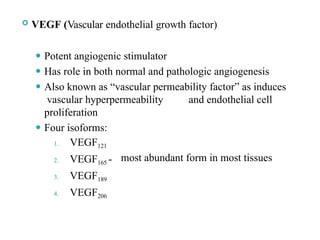
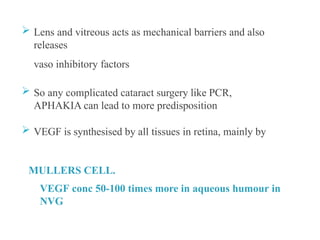
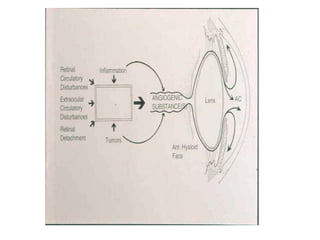
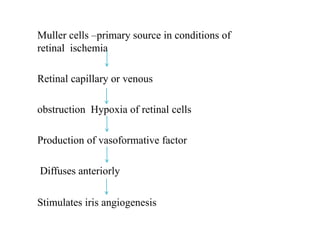
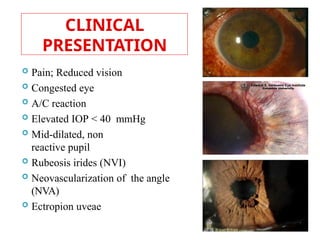
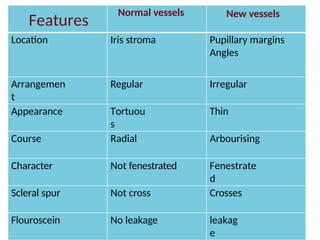
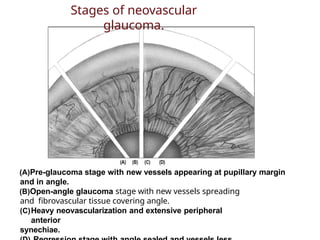
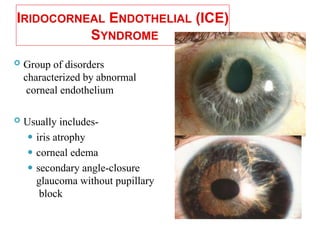
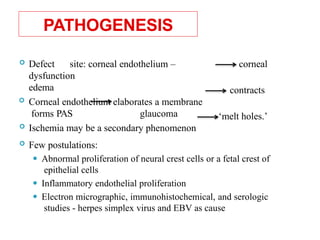
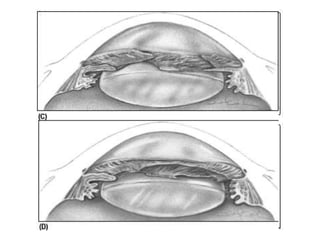
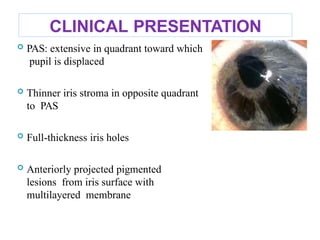
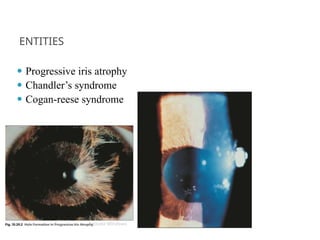
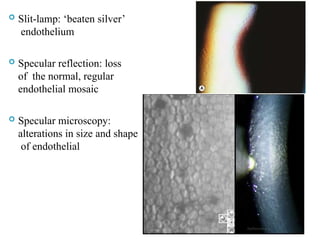
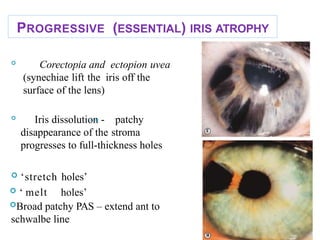
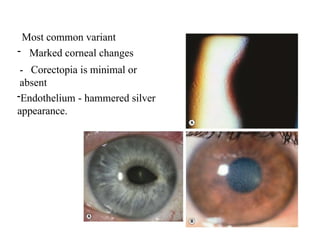
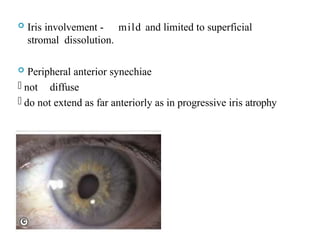
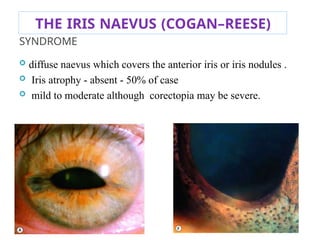
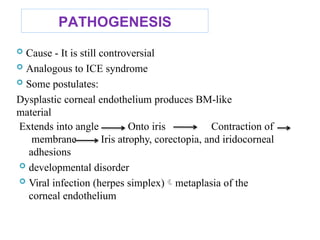
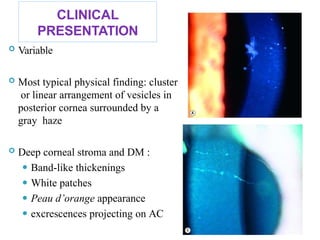
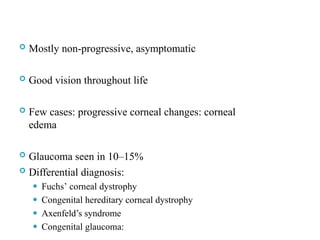
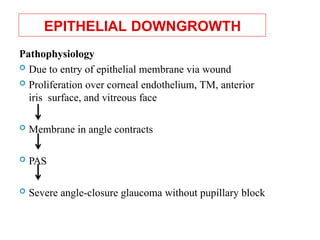
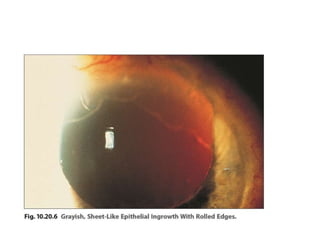
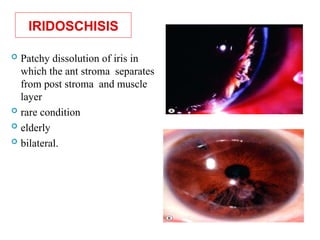
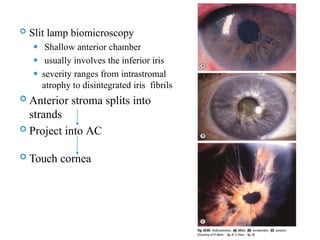
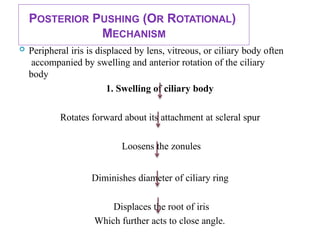
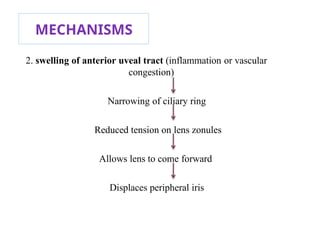
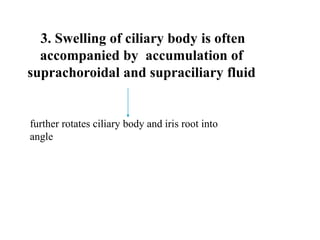
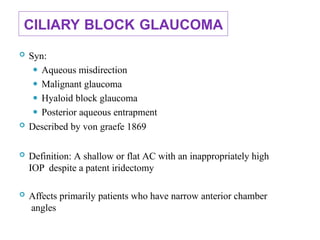
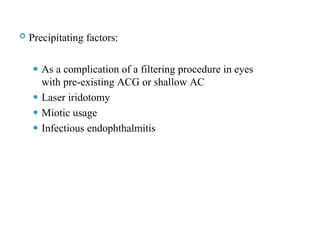
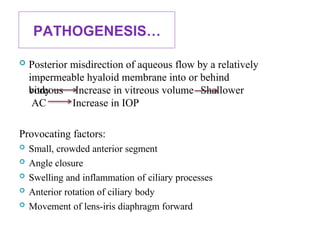
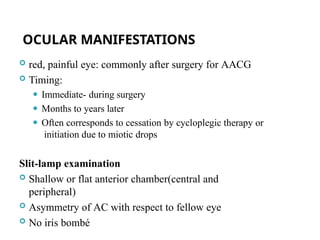
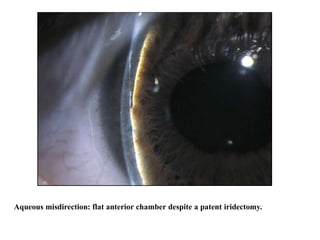
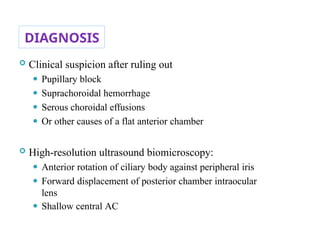
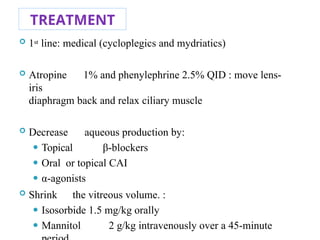
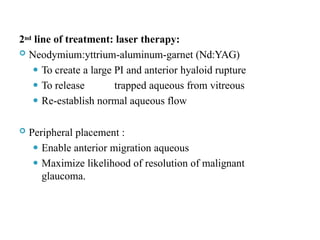
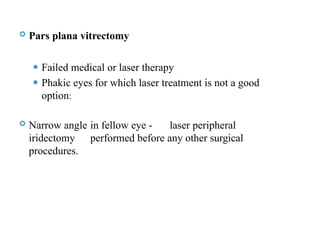
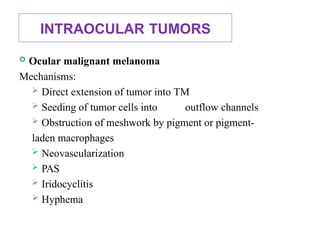
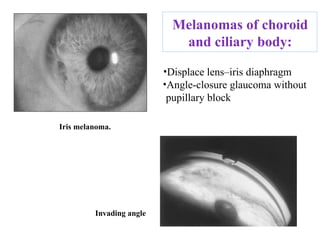
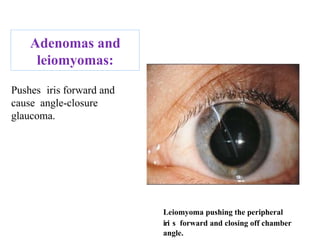
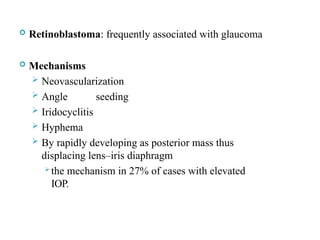
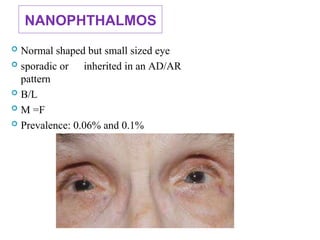
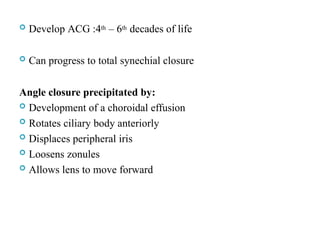
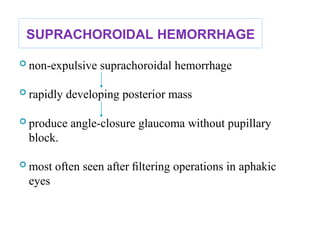
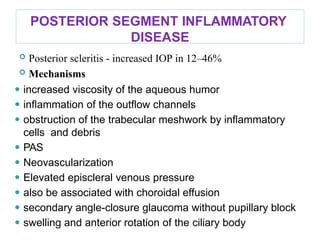
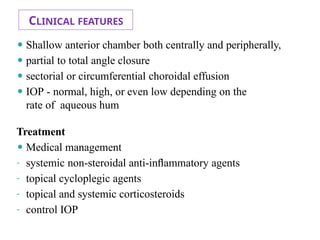
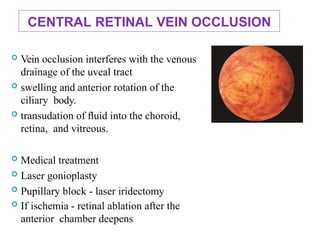
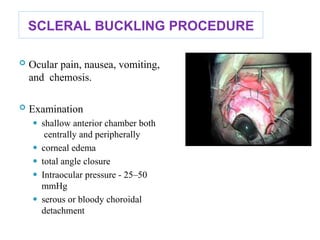
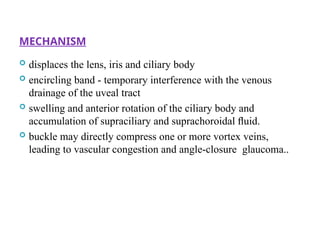
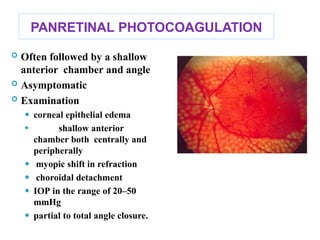
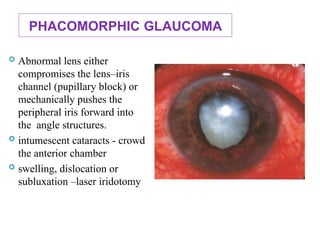
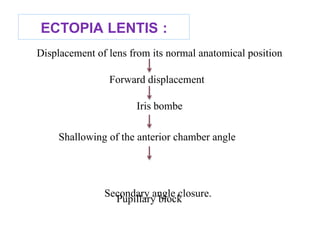
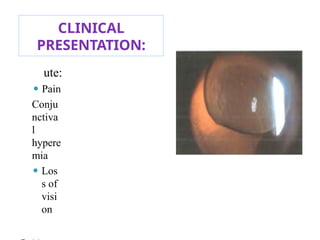
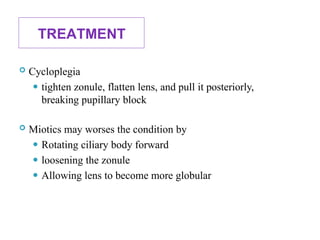
The document discusses secondary angle closure glaucoma, which is caused by impaired aqueous outflow due to apposition between the peripheral iris and the trabeculum. It presents two fundamental mechanisms—anterior pulling and posterior pushing—and highlights the importance of diagnosis and treatment options, including panretinal photocoagulation and anti-VEGF therapies. The document also covers related conditions such as neovascular glaucoma, iridocorneal endothelial syndrome, and other factors contributing to this type of glaucoma.