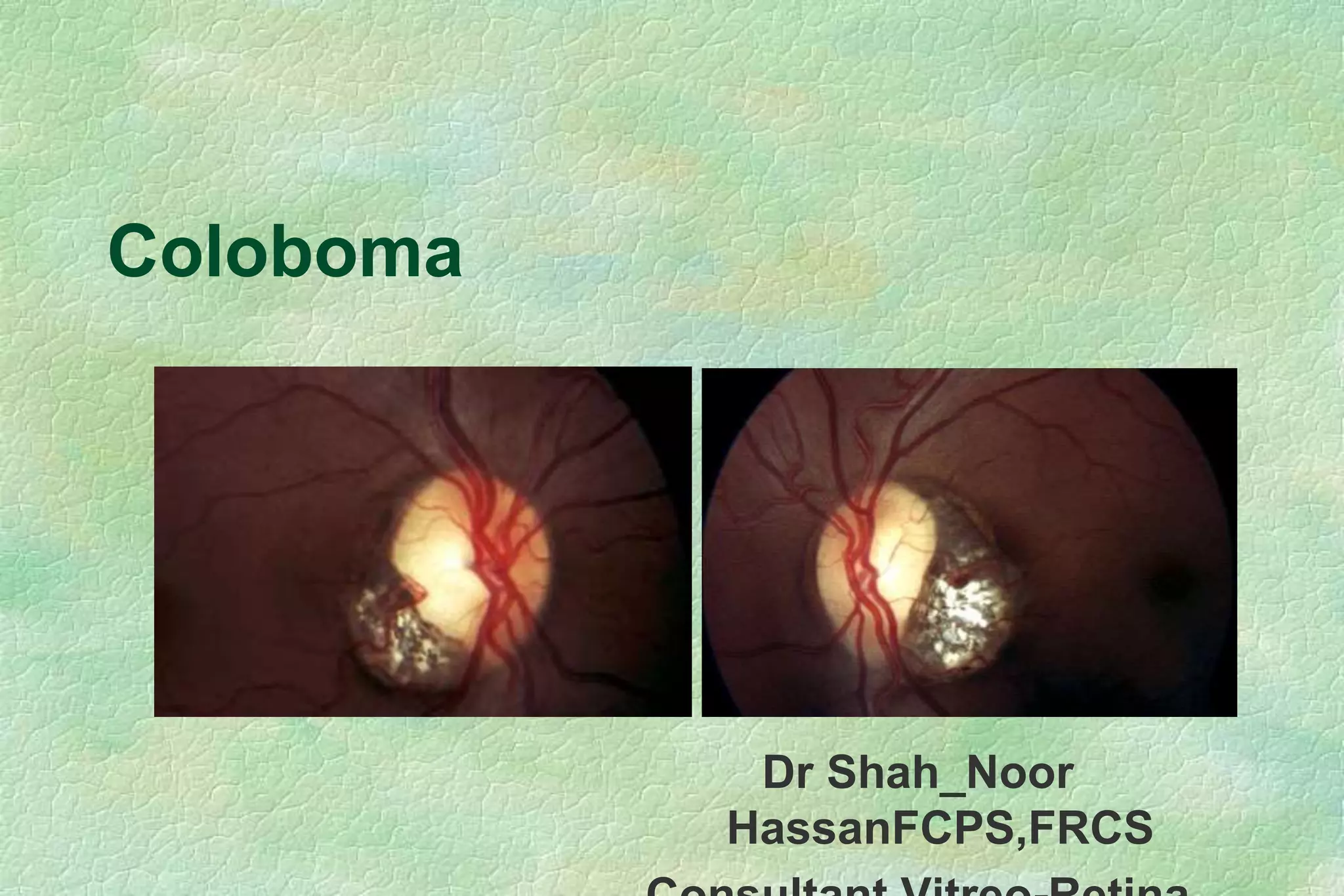
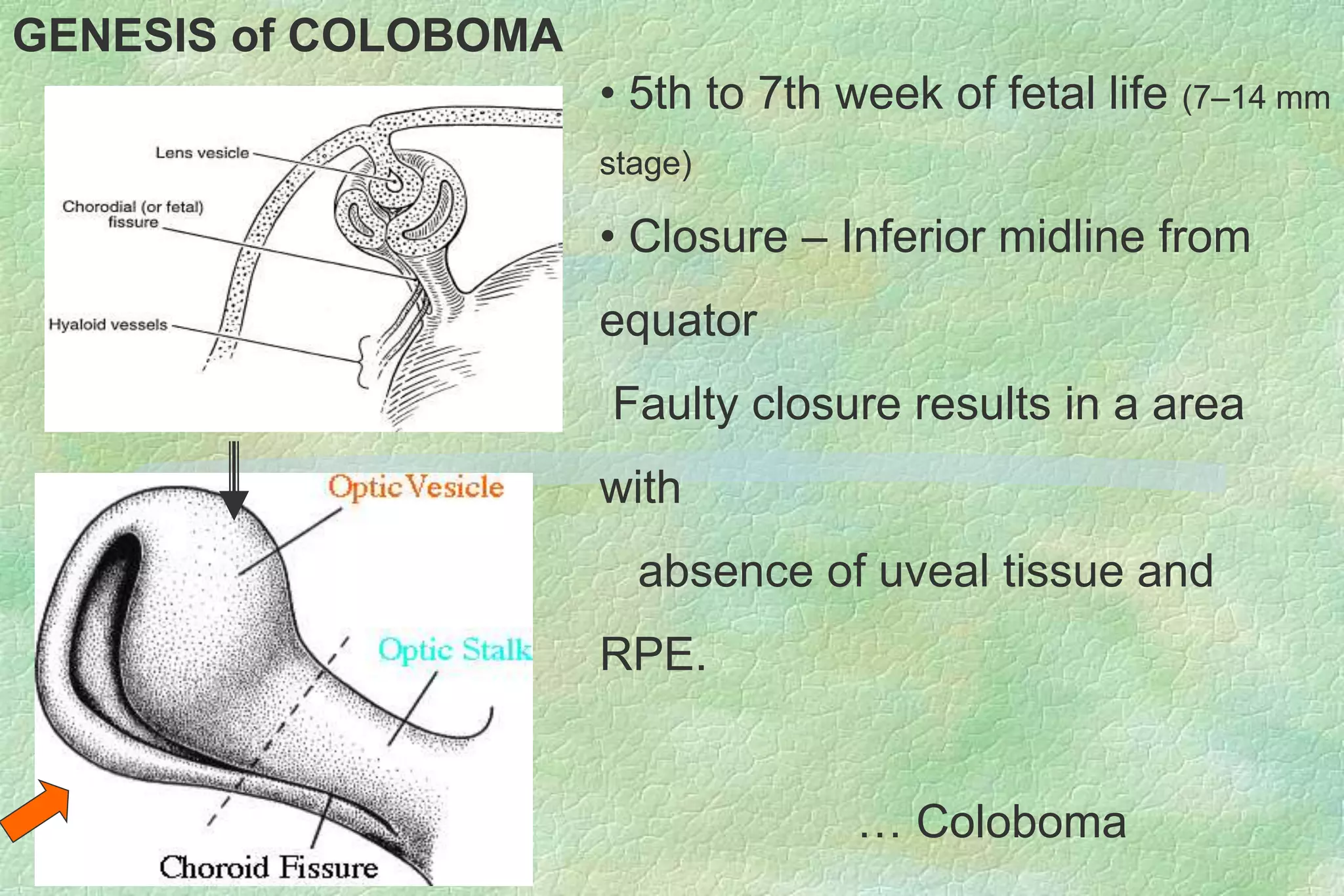
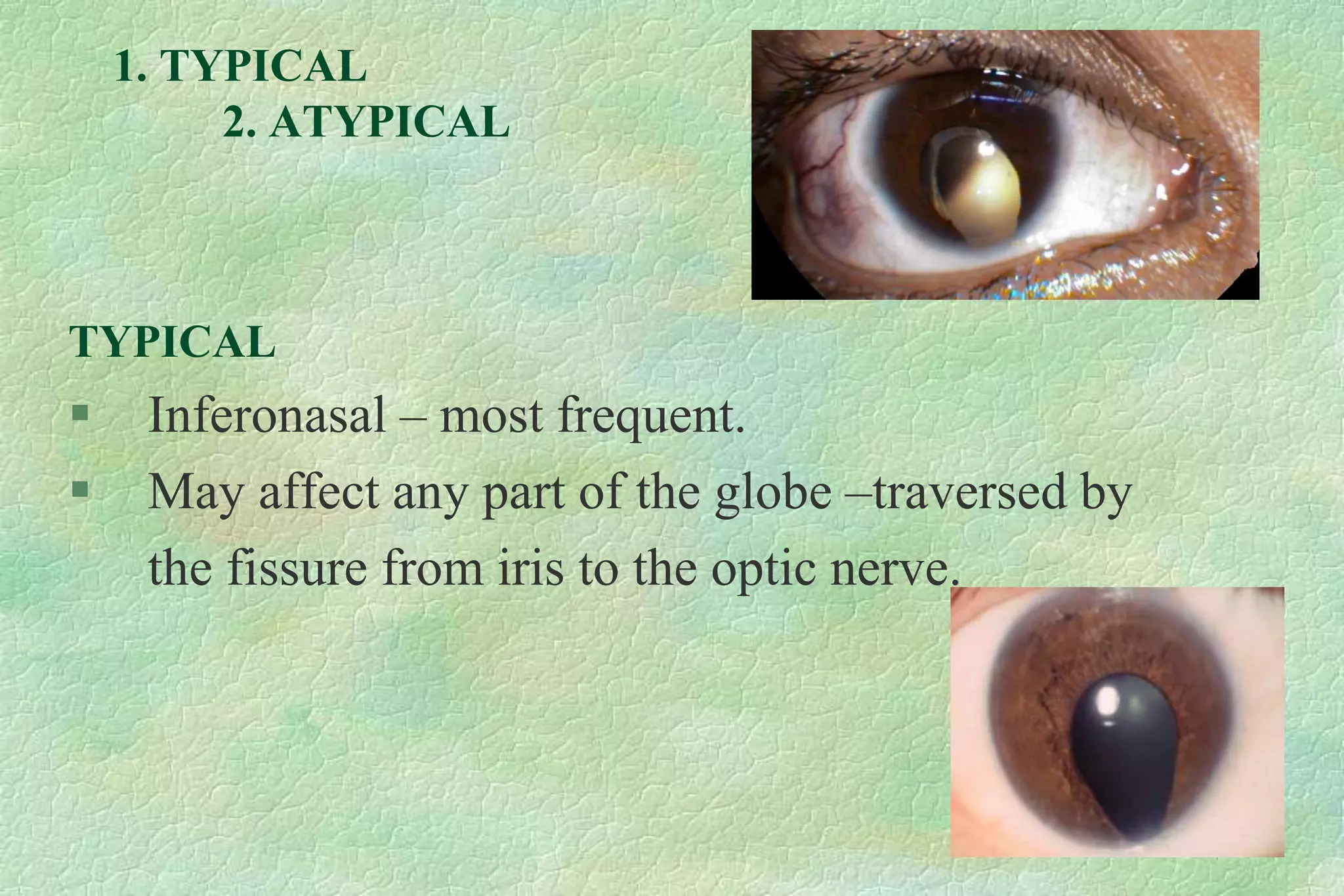
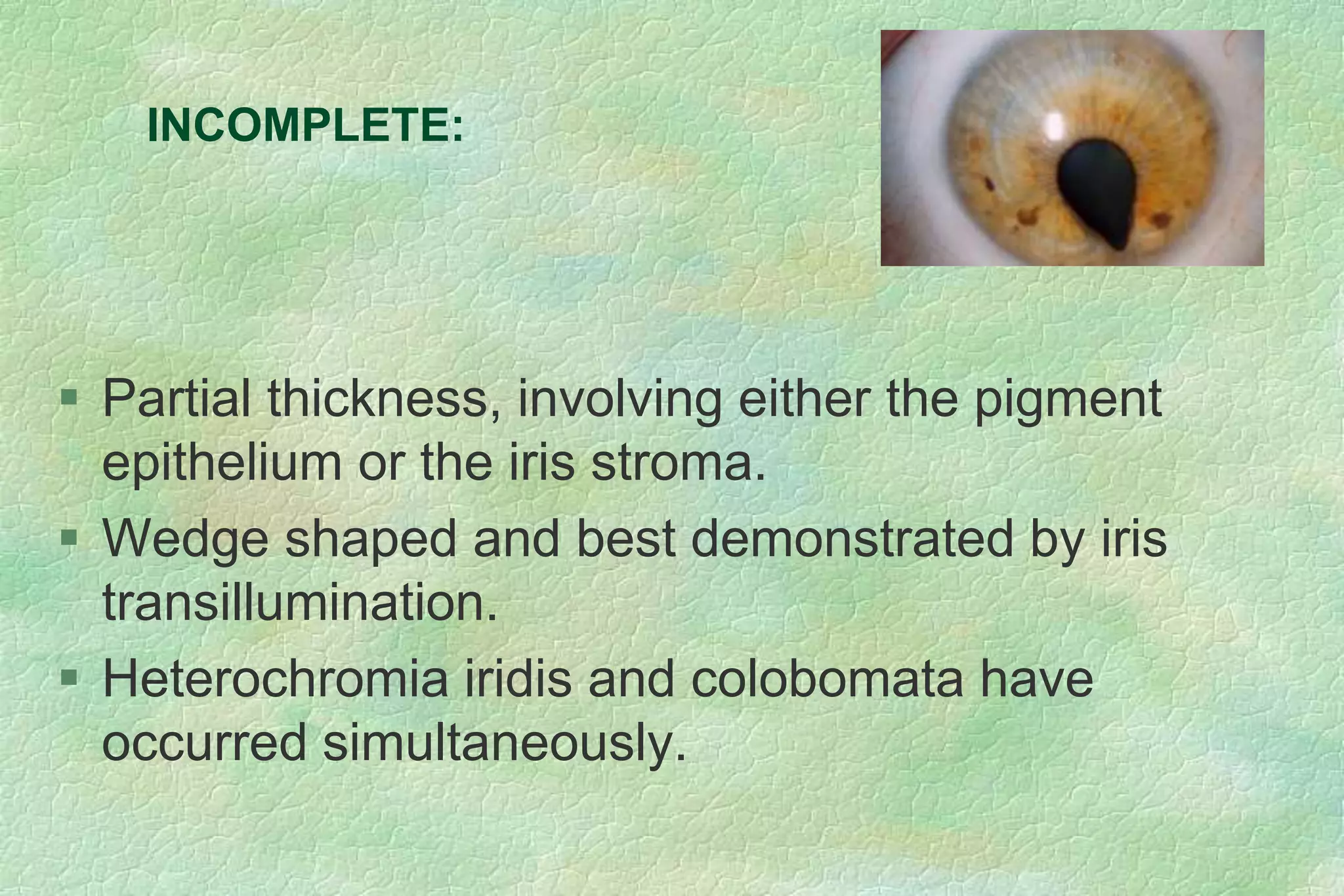
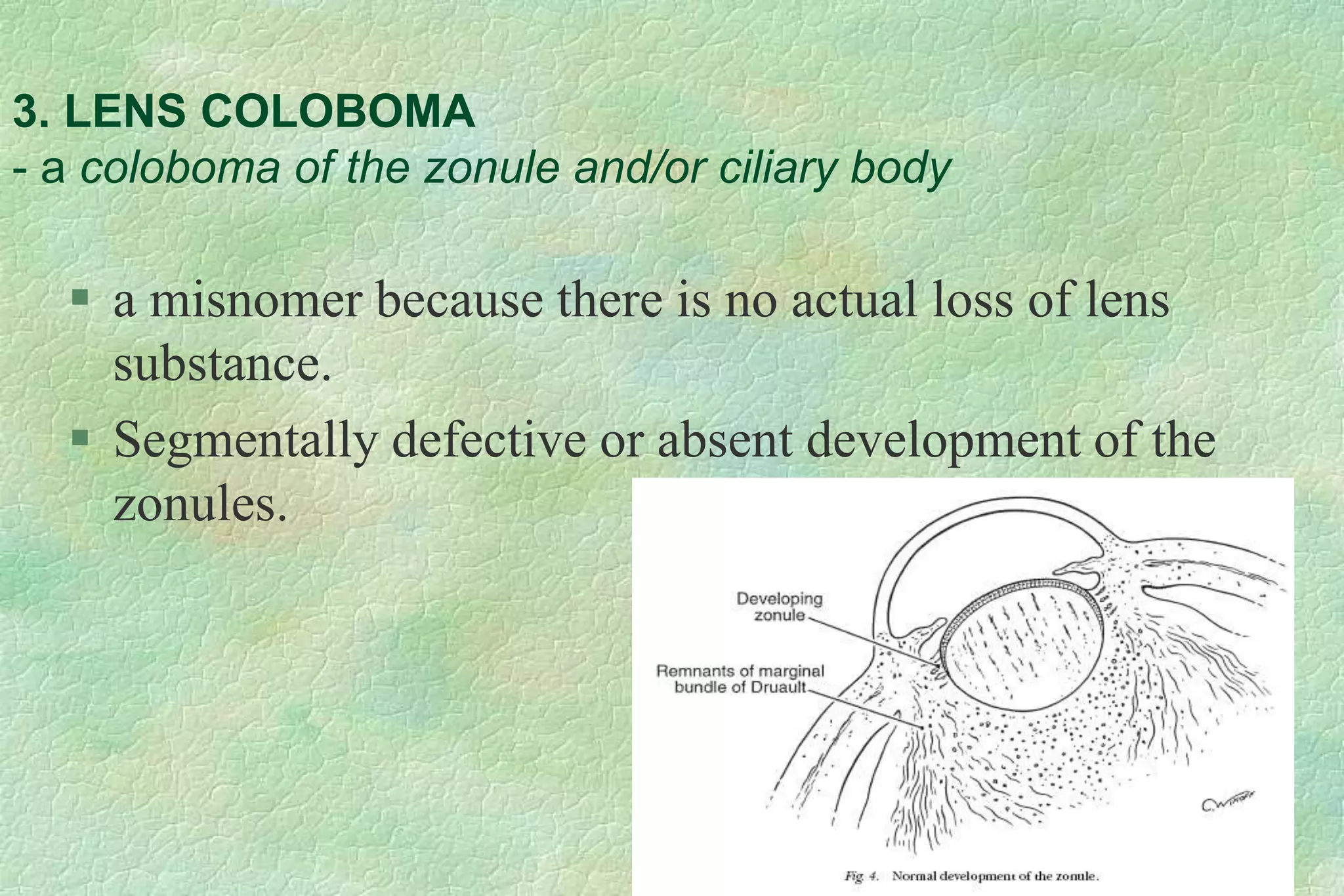
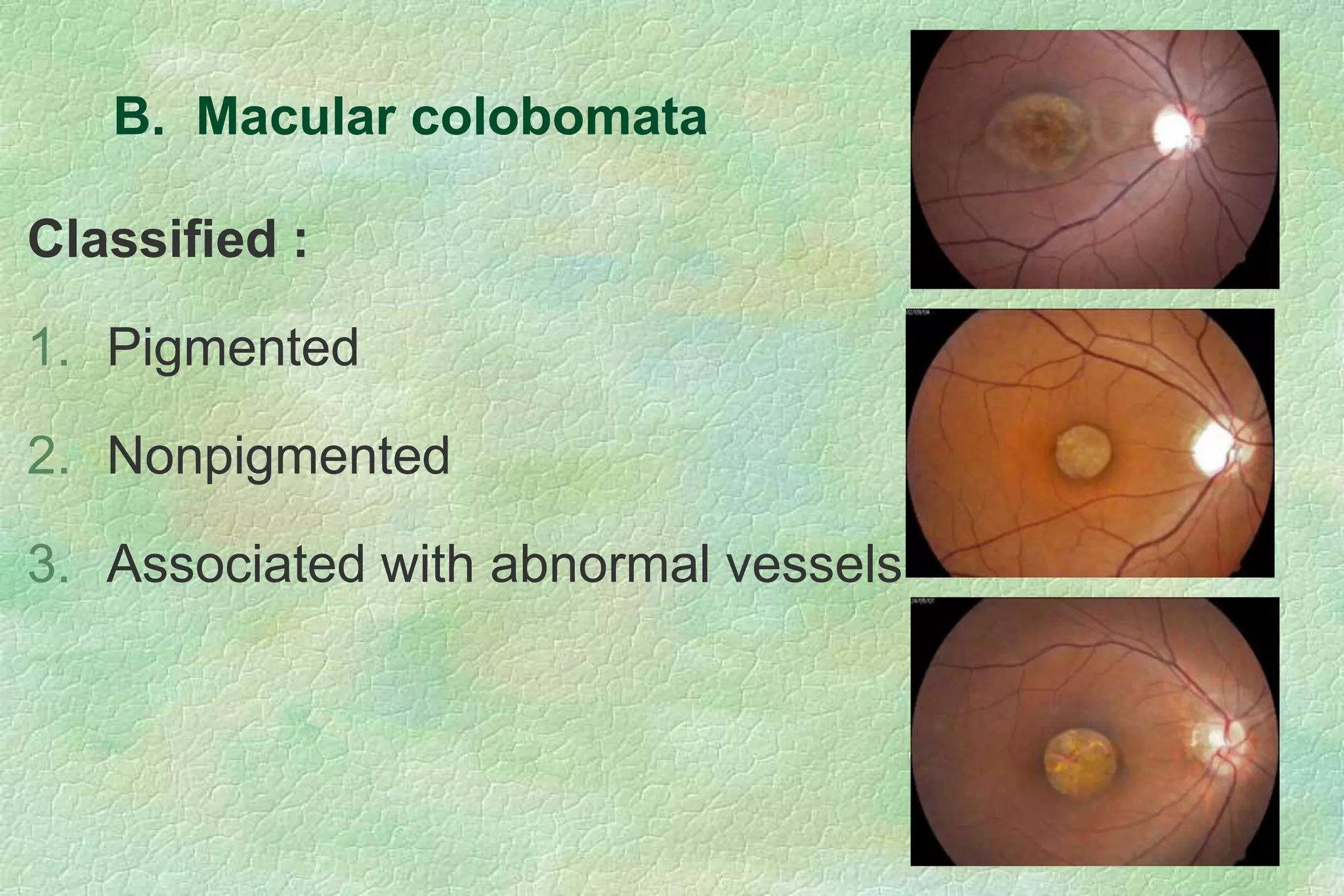
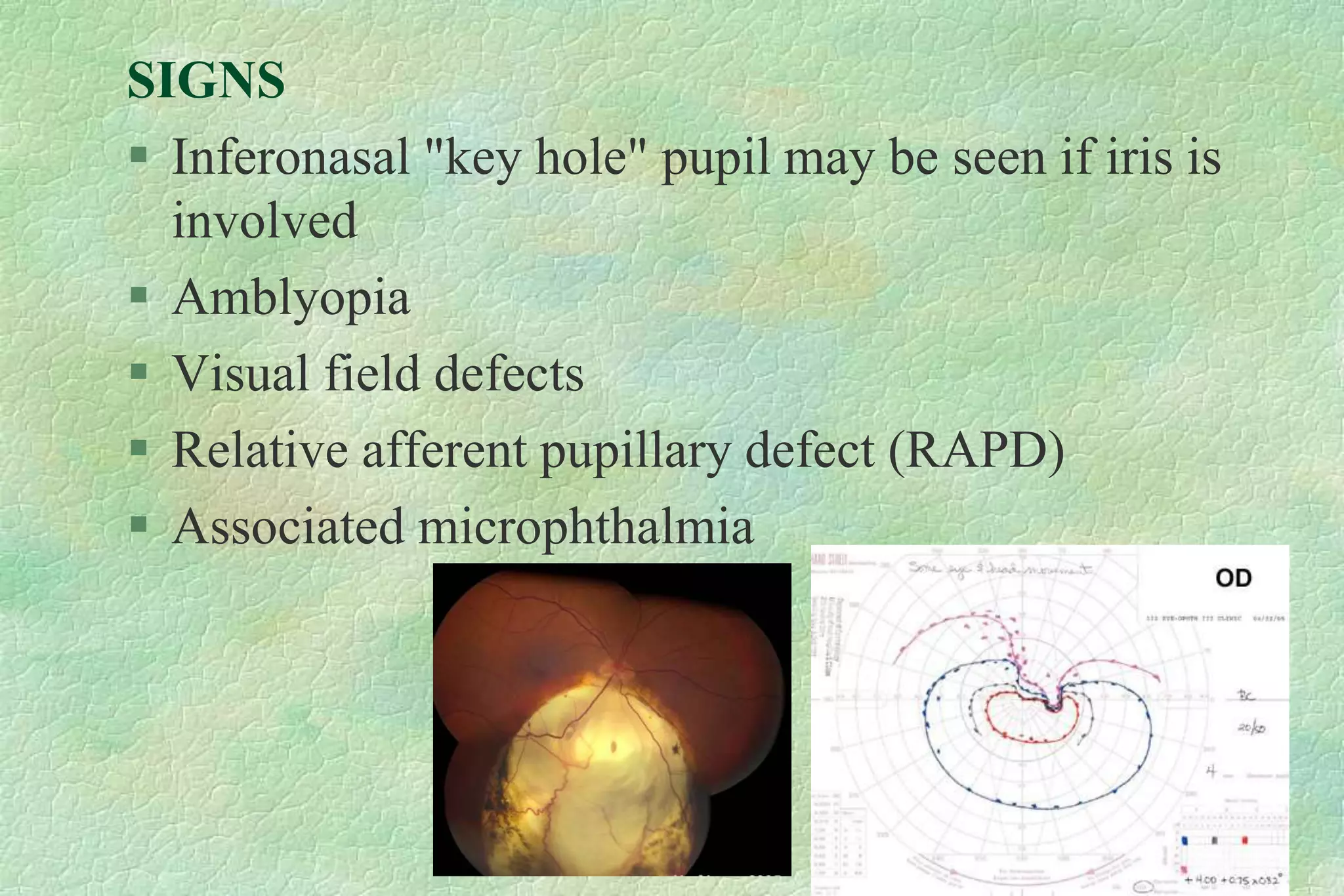
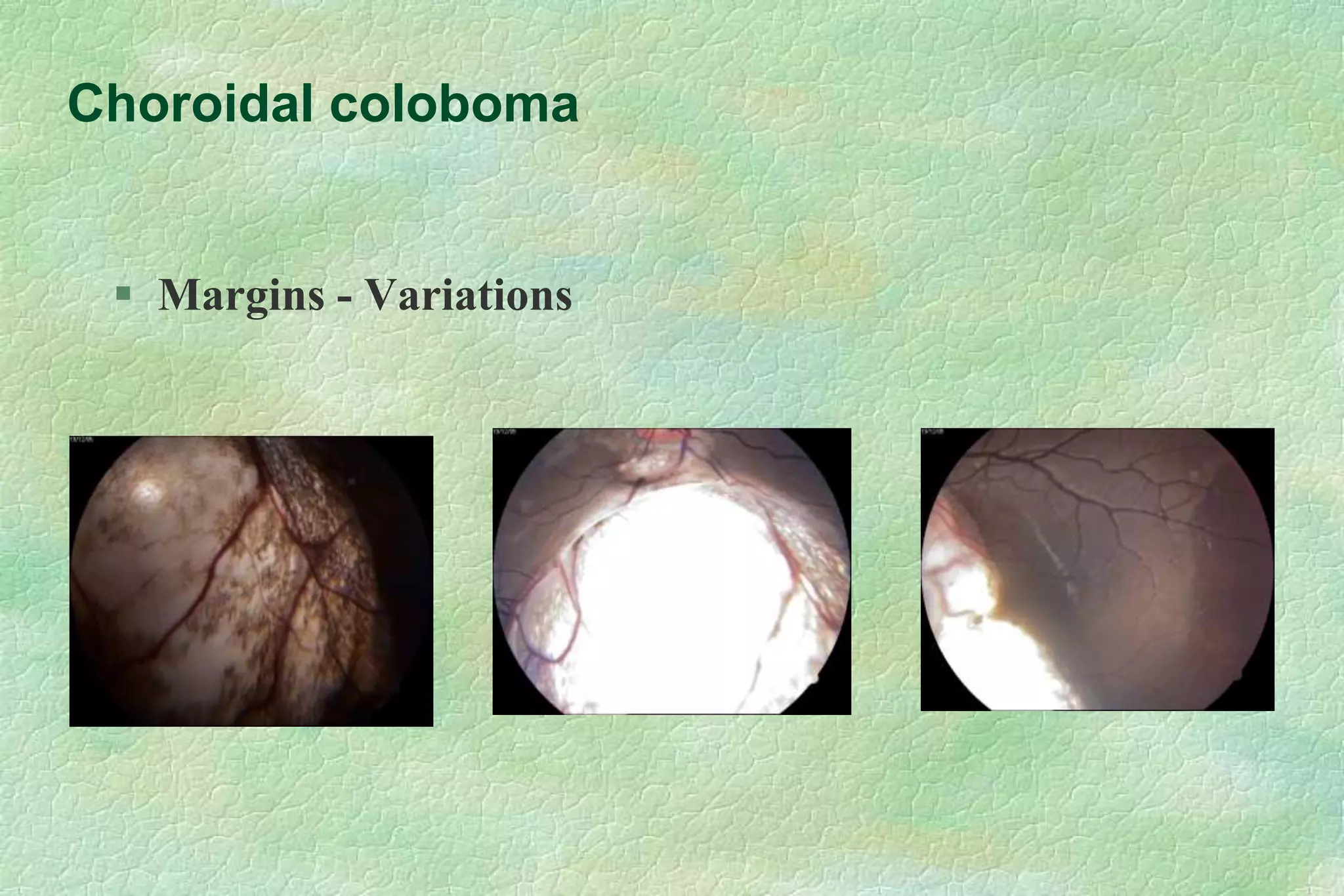
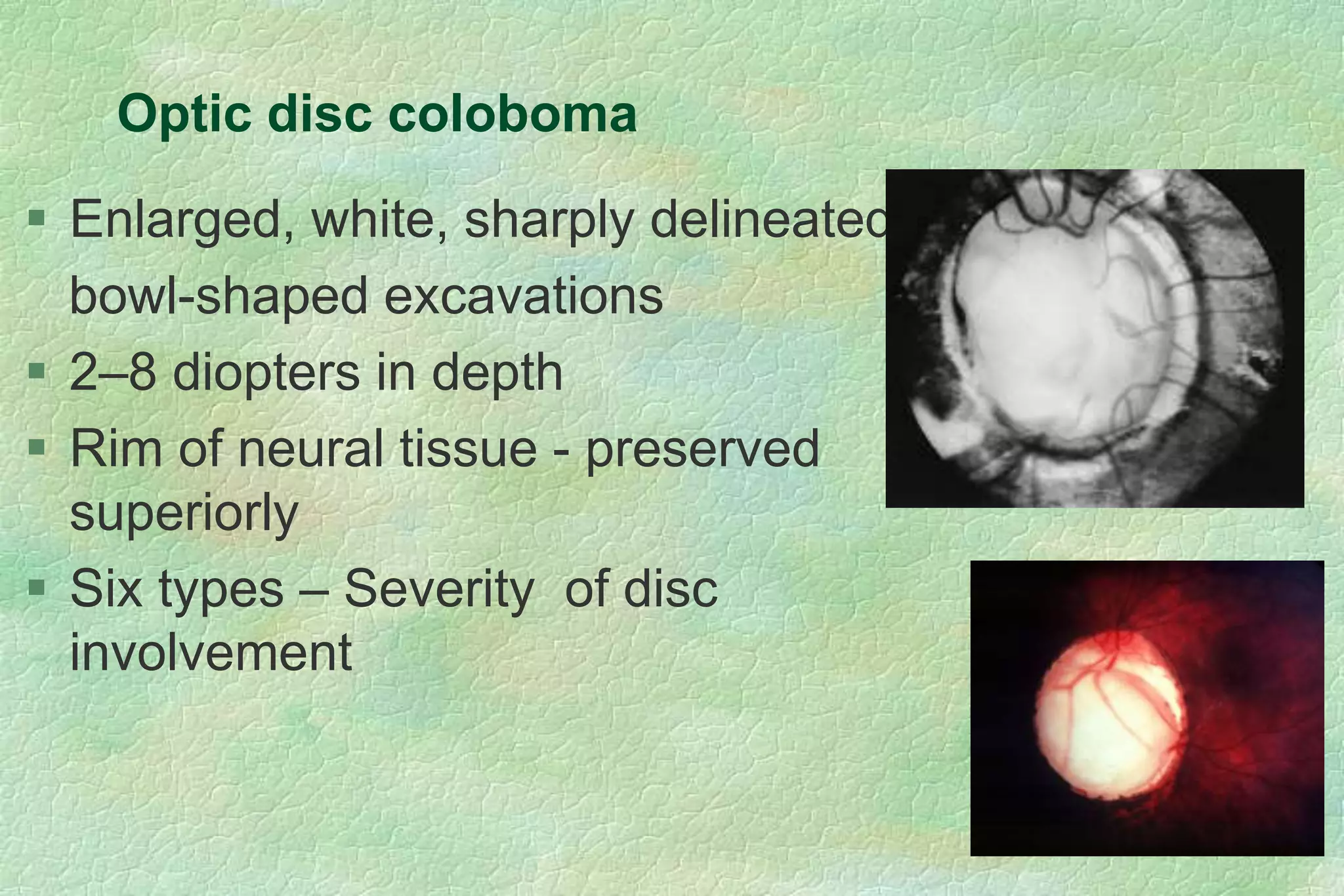
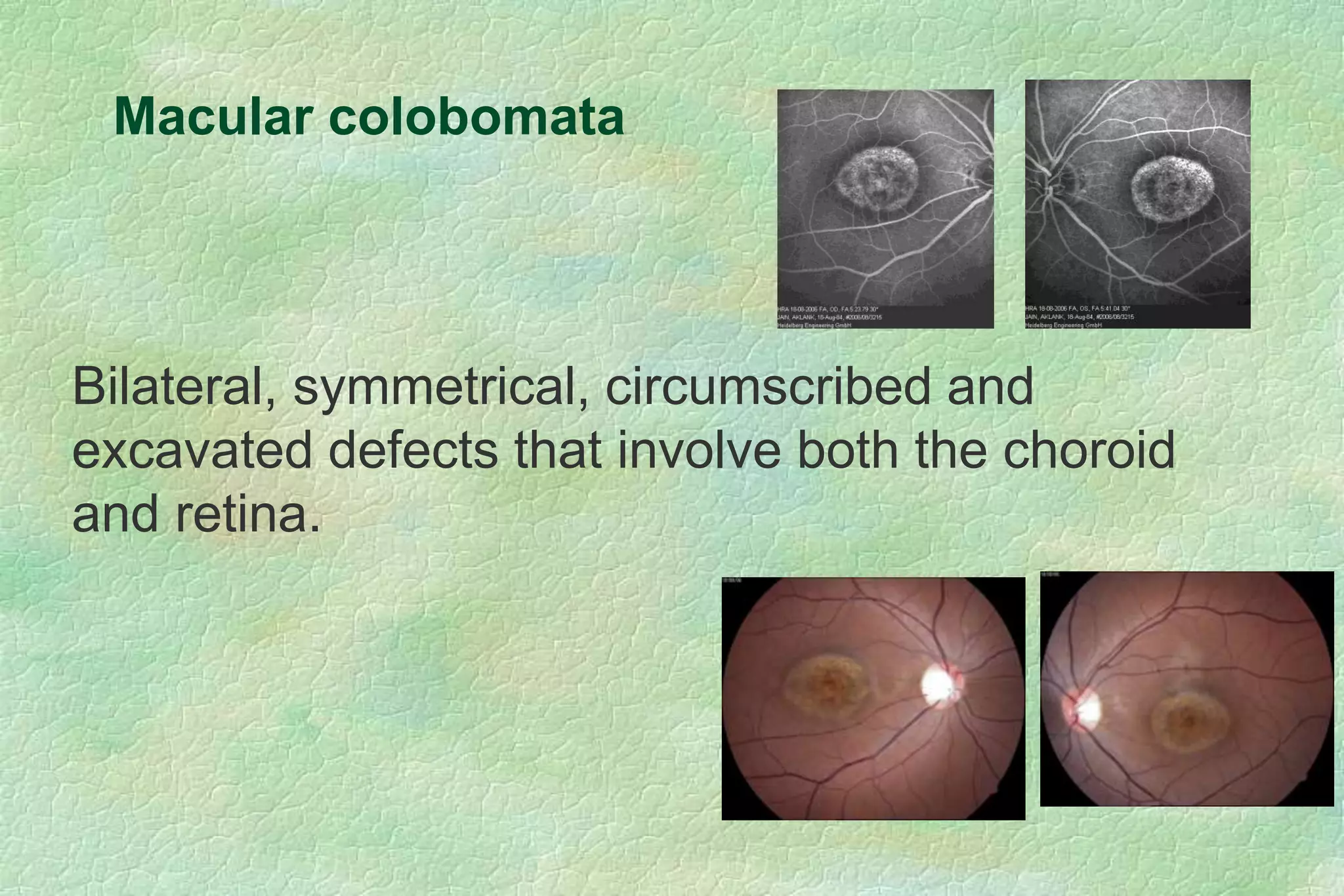
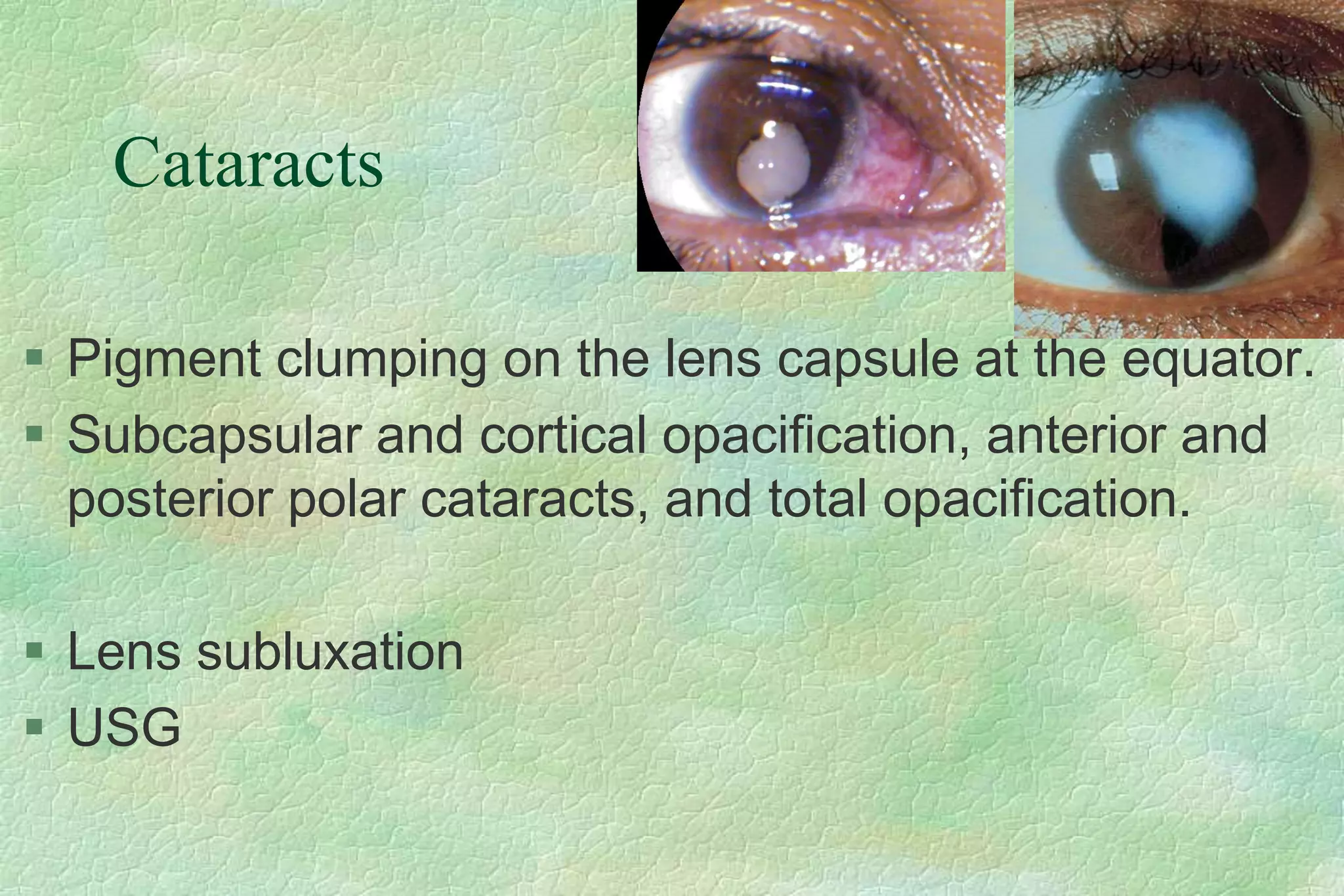
This document discusses coloboma, which is an embryologic defect resulting in a notch or gap in ocular structures. It can affect the iris, choroid, optic disc, or macula. Coloboma is usually sporadic but sometimes associated with genetic syndromes. Complications include retinal detachment, cataract, glaucoma, and amblyopia. Diagnosis involves examination and imaging. Management depends on the location and severity but may include treatment of refractive error, retinal detachment surgery, or cataract surgery. Prognosis depends on the structures involved, with macular or optic nerve coloboma having worse visual outcomes.