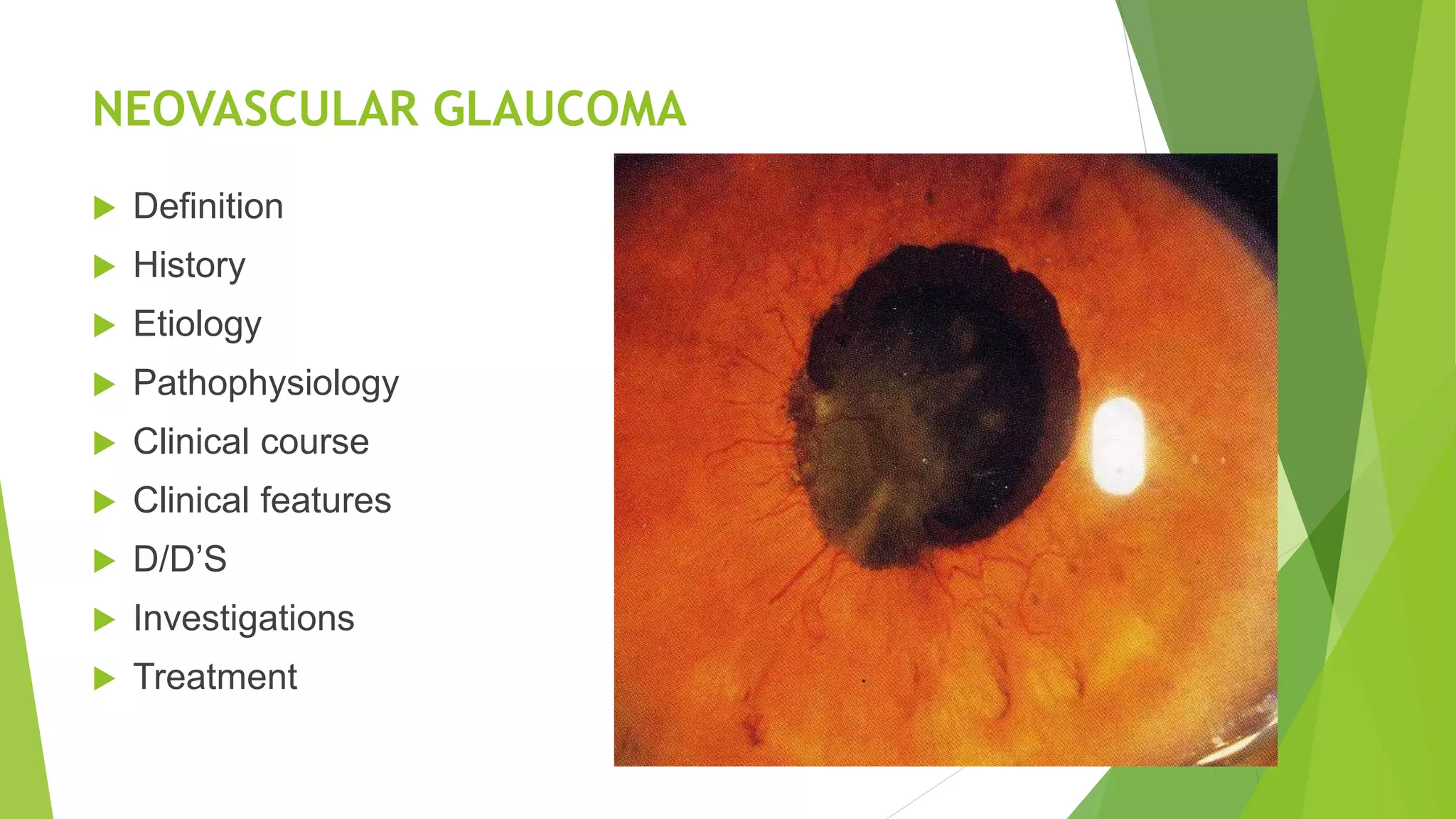
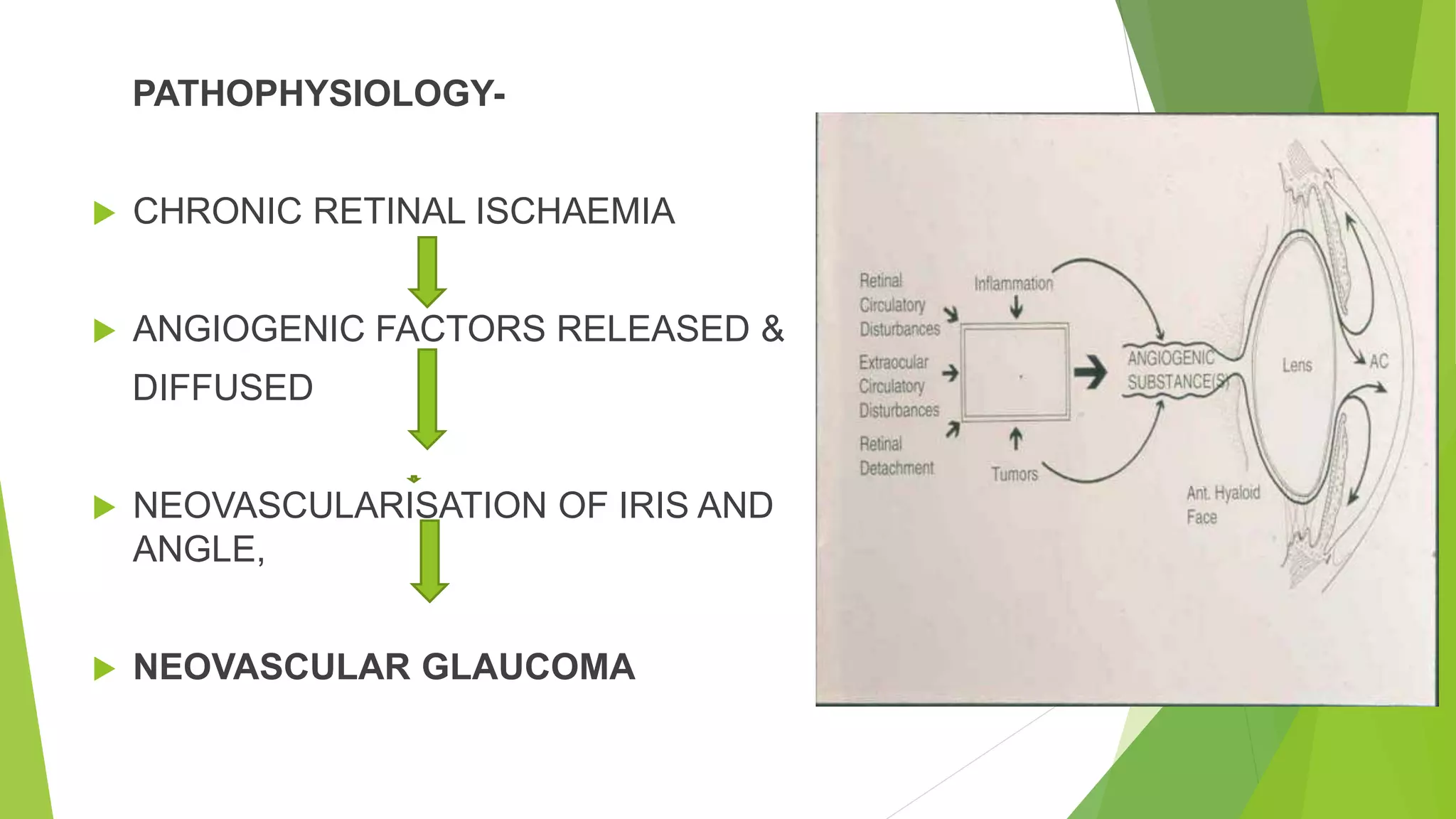
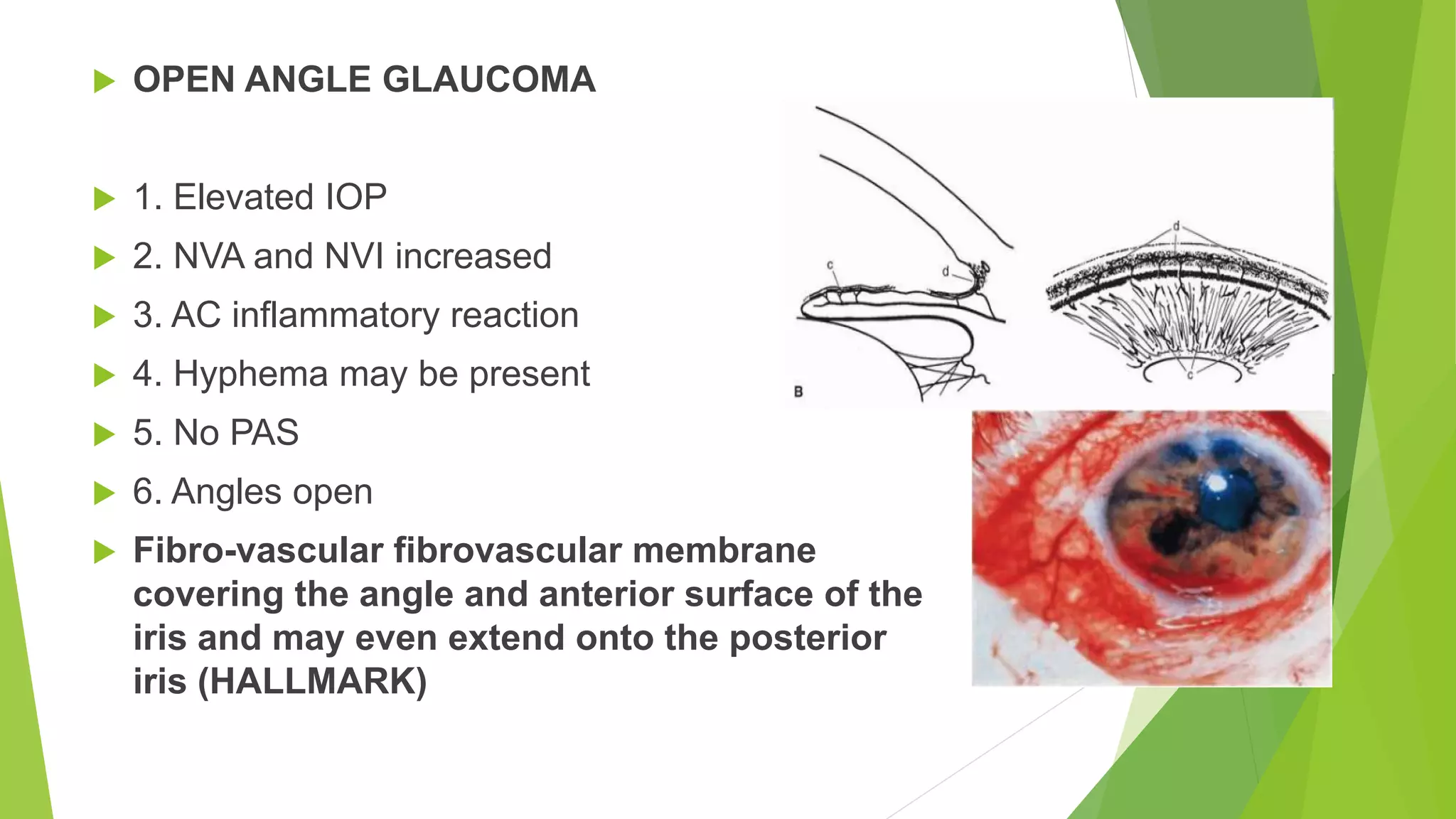
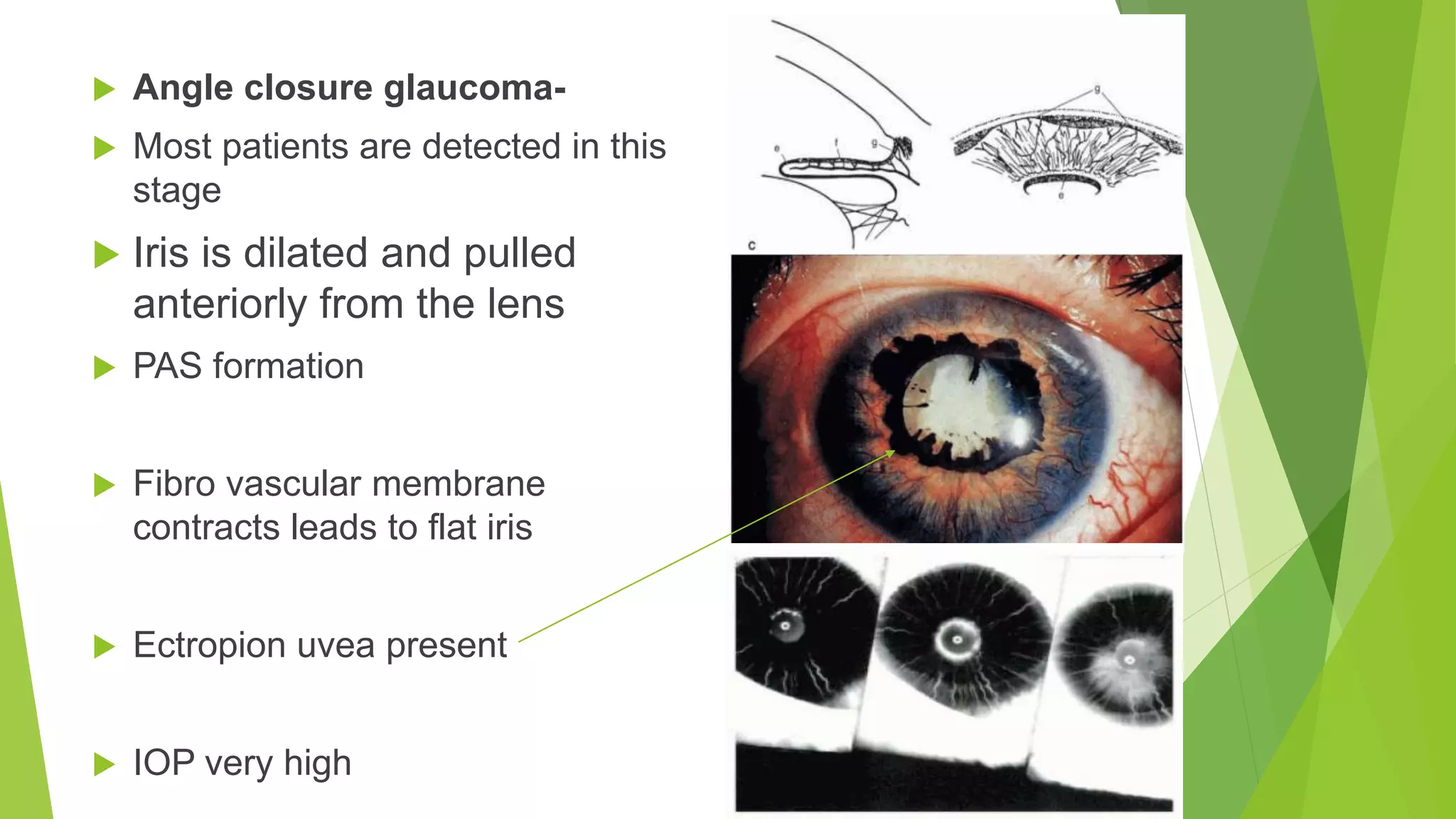
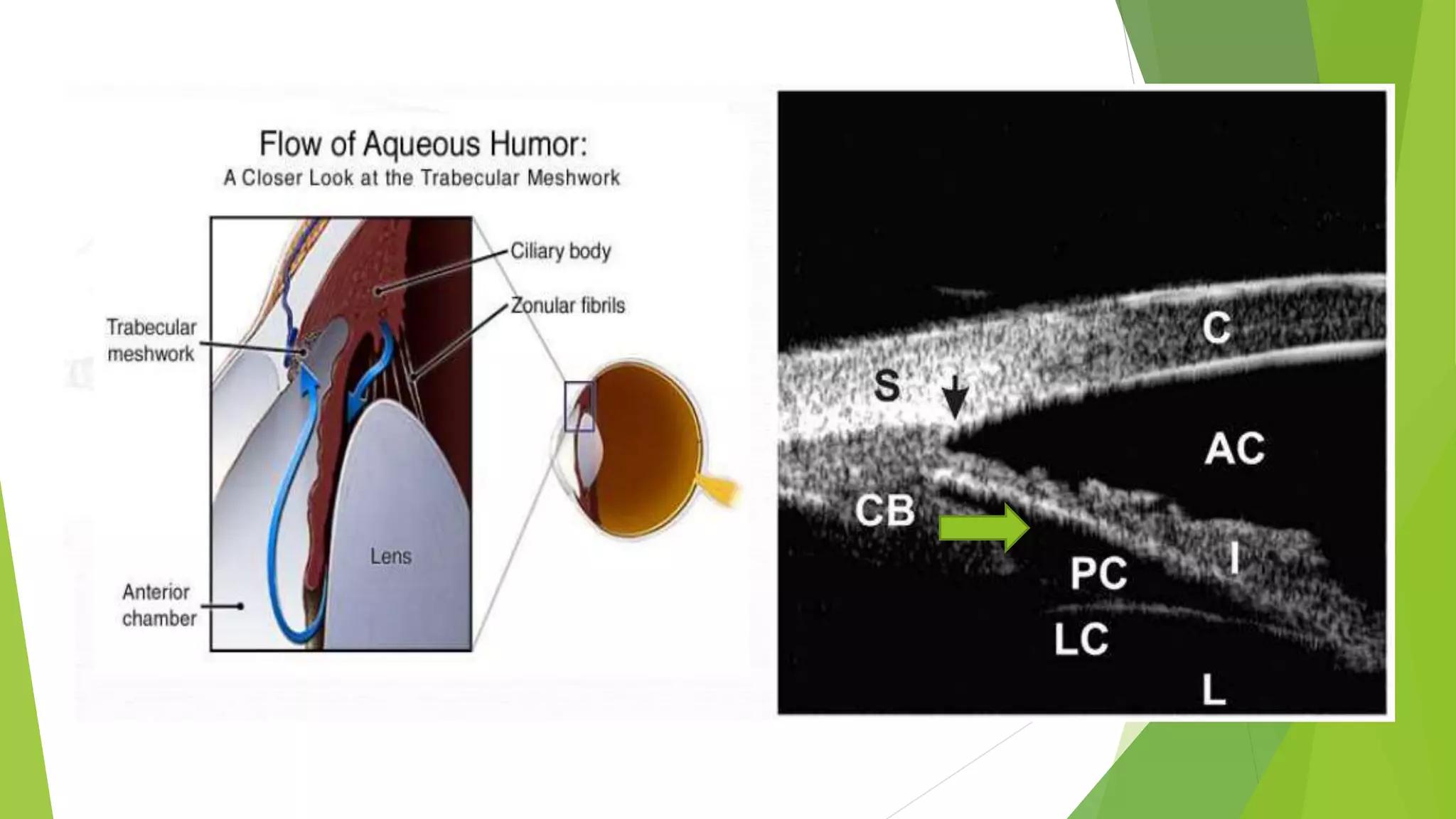
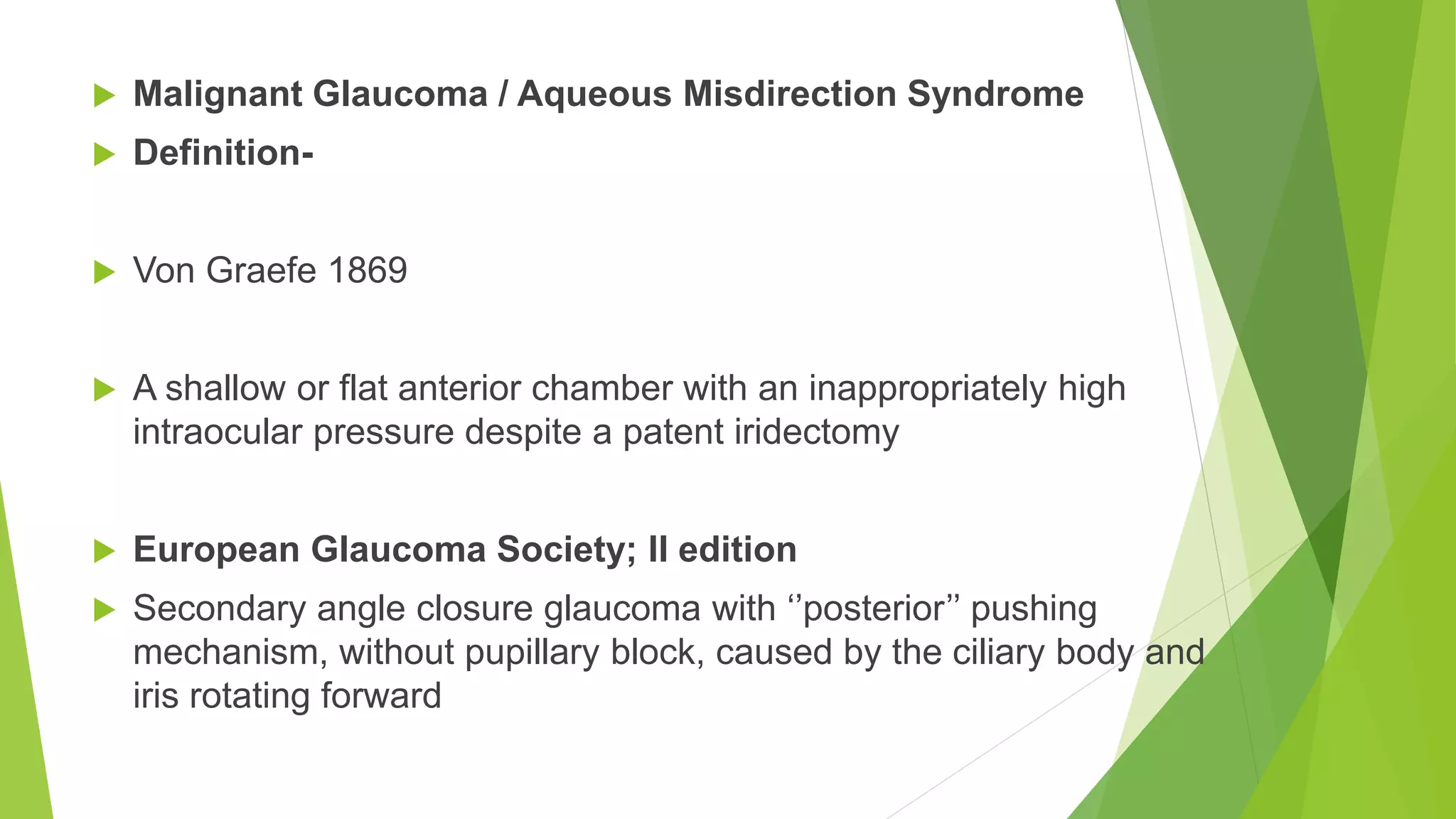
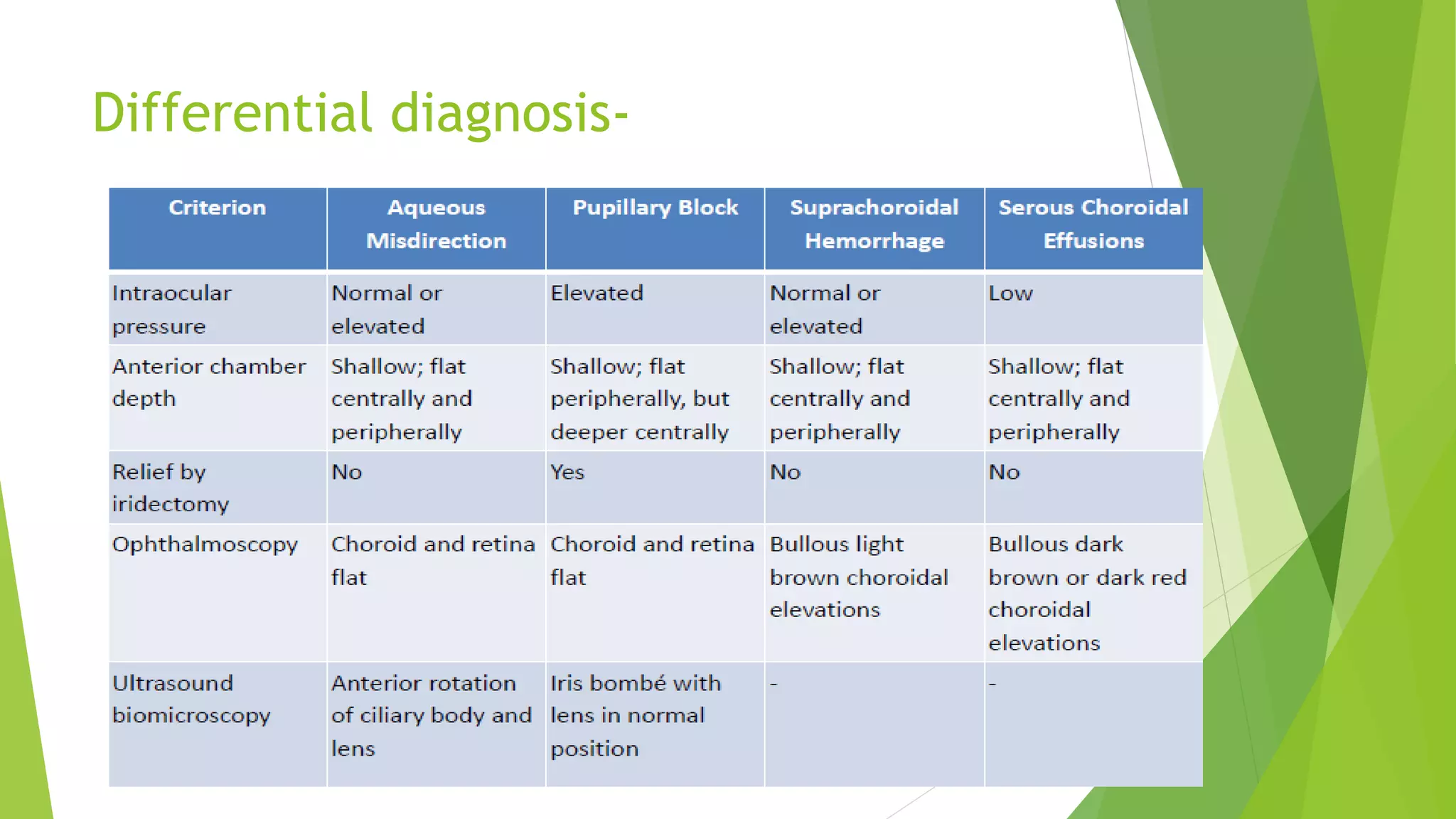
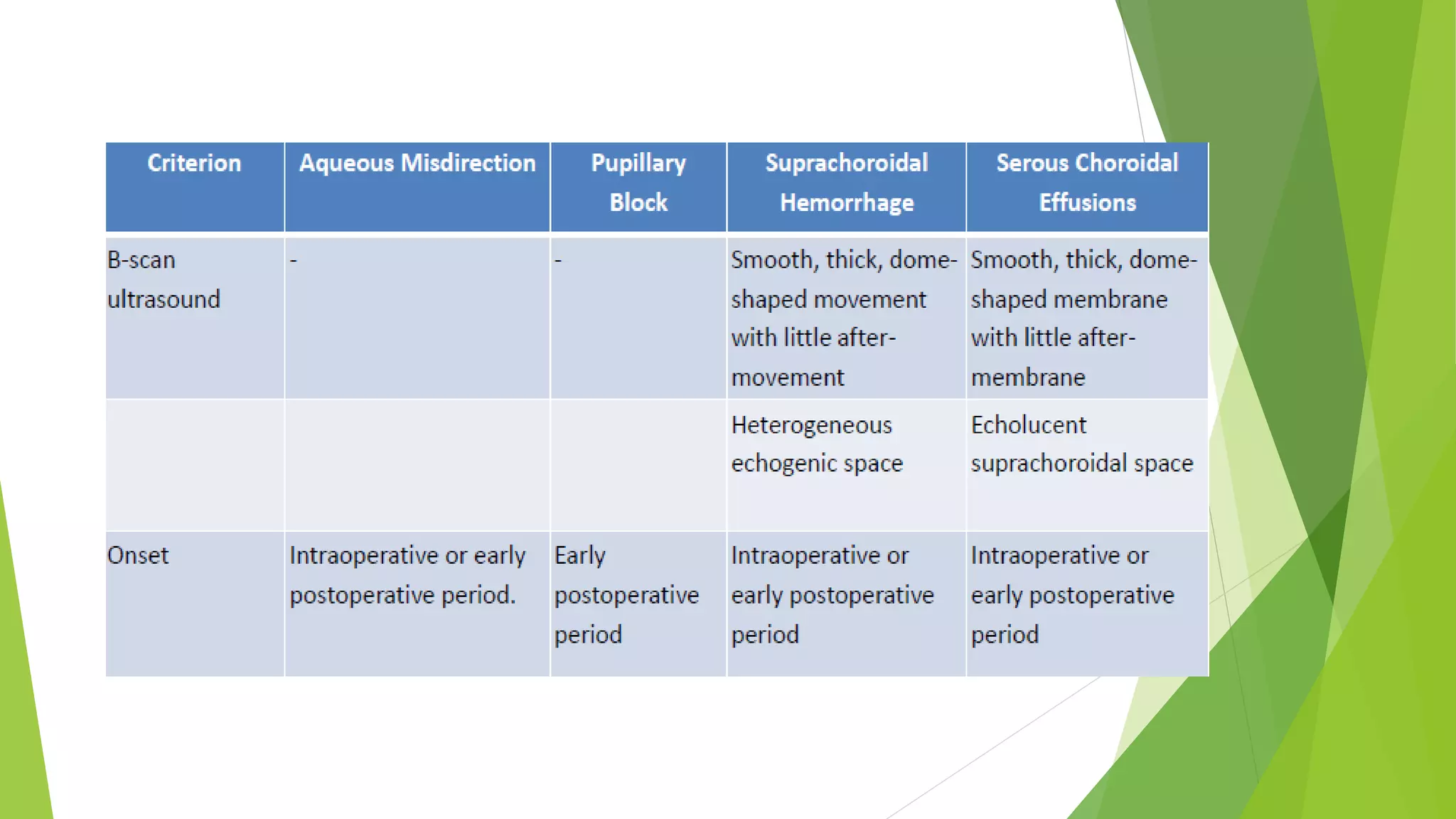
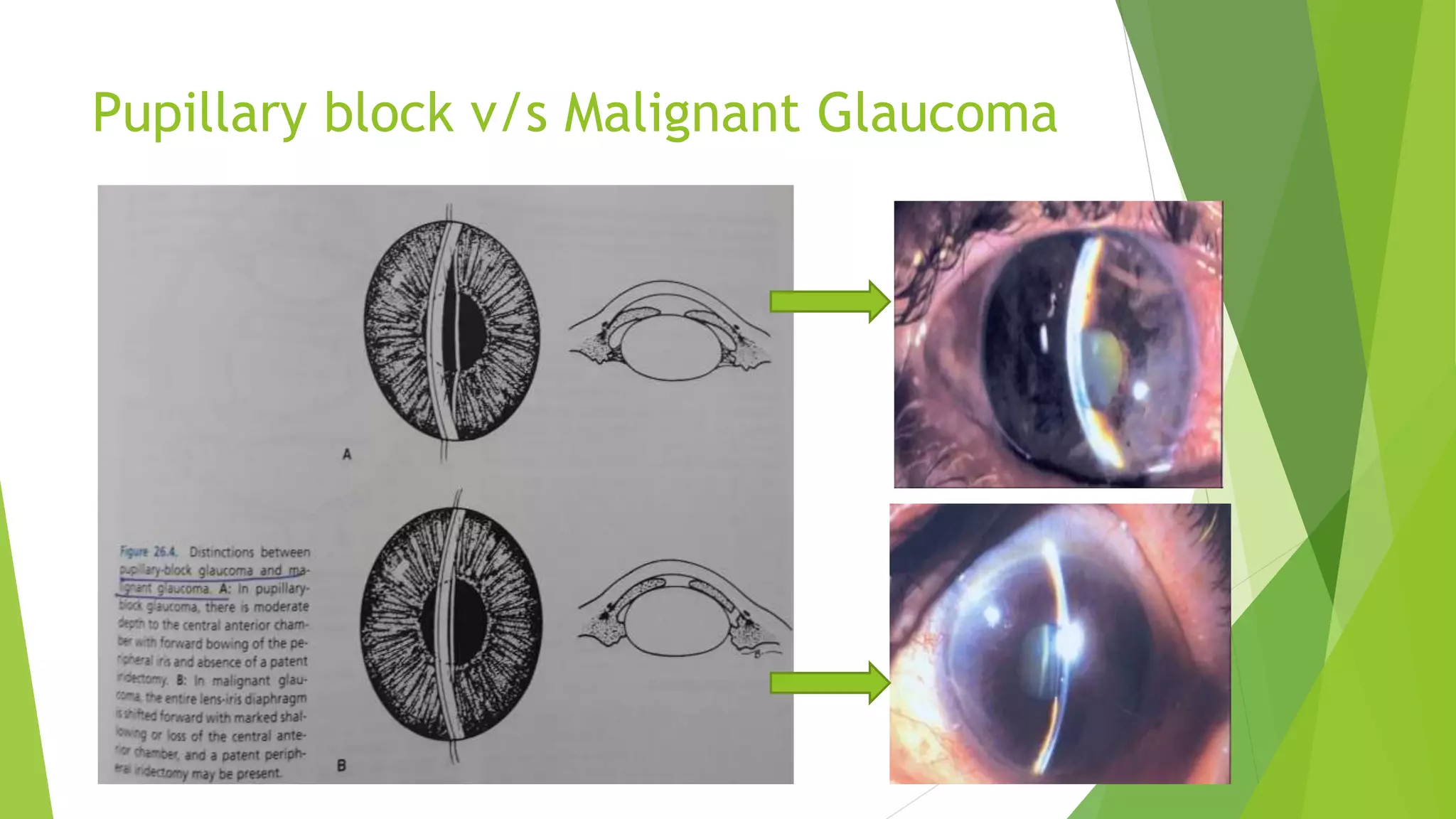
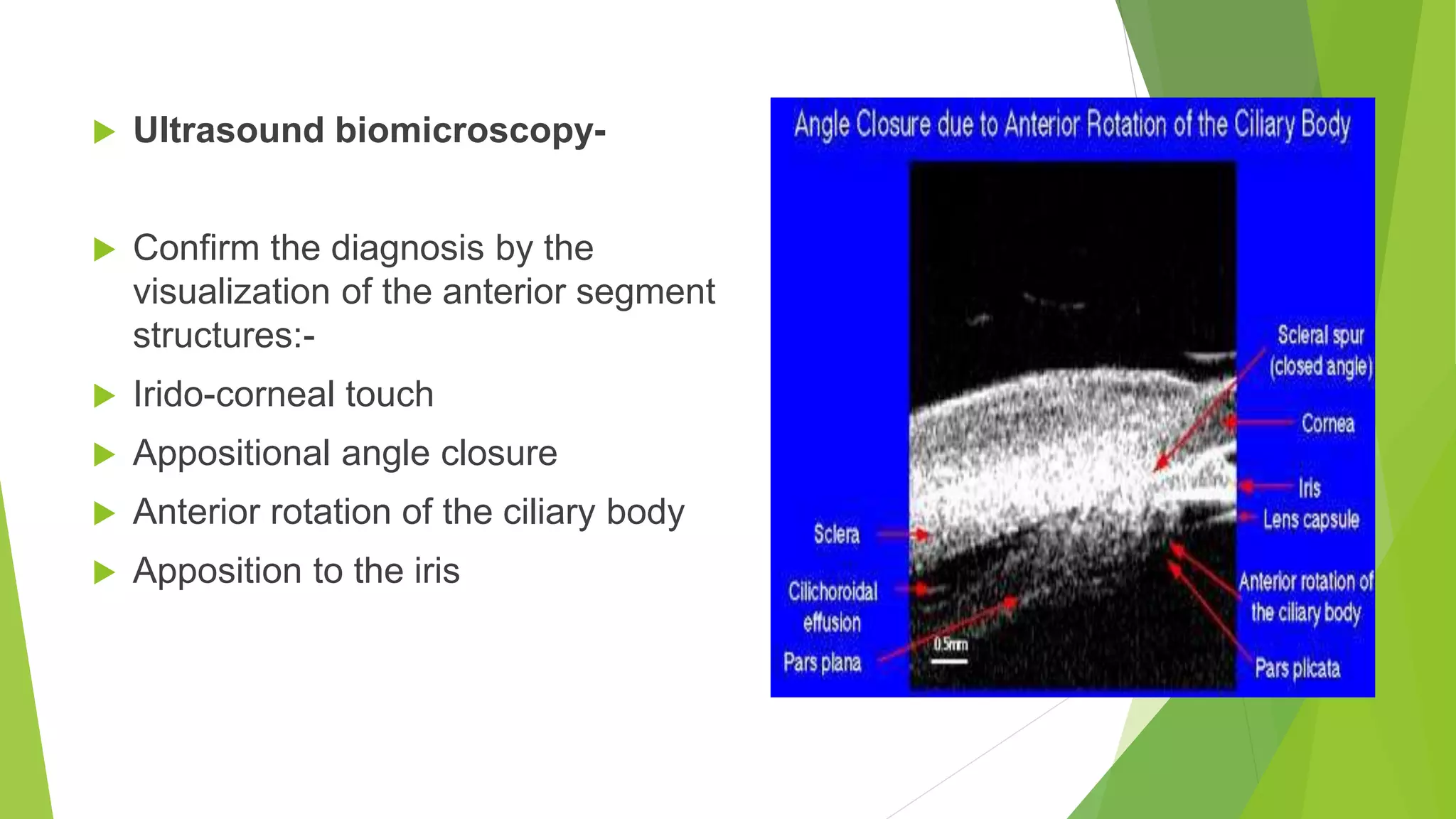
This document discusses three types of secondary glaucoma: neovascular glaucoma, aqueous misdirection syndrome, and uveitic glaucoma. Neovascular glaucoma is caused by fibrovascular proliferation in the anterior chamber angle due to underlying conditions like proliferative diabetic retinopathy. Aqueous misdirection syndrome involves aqueous flowing into the vitreous cavity rather than the anterior chamber. Uveitic glaucoma can develop in 10% of patients with uveitis and results from trabeculitis, steroid use, or neovascularization among other causes.