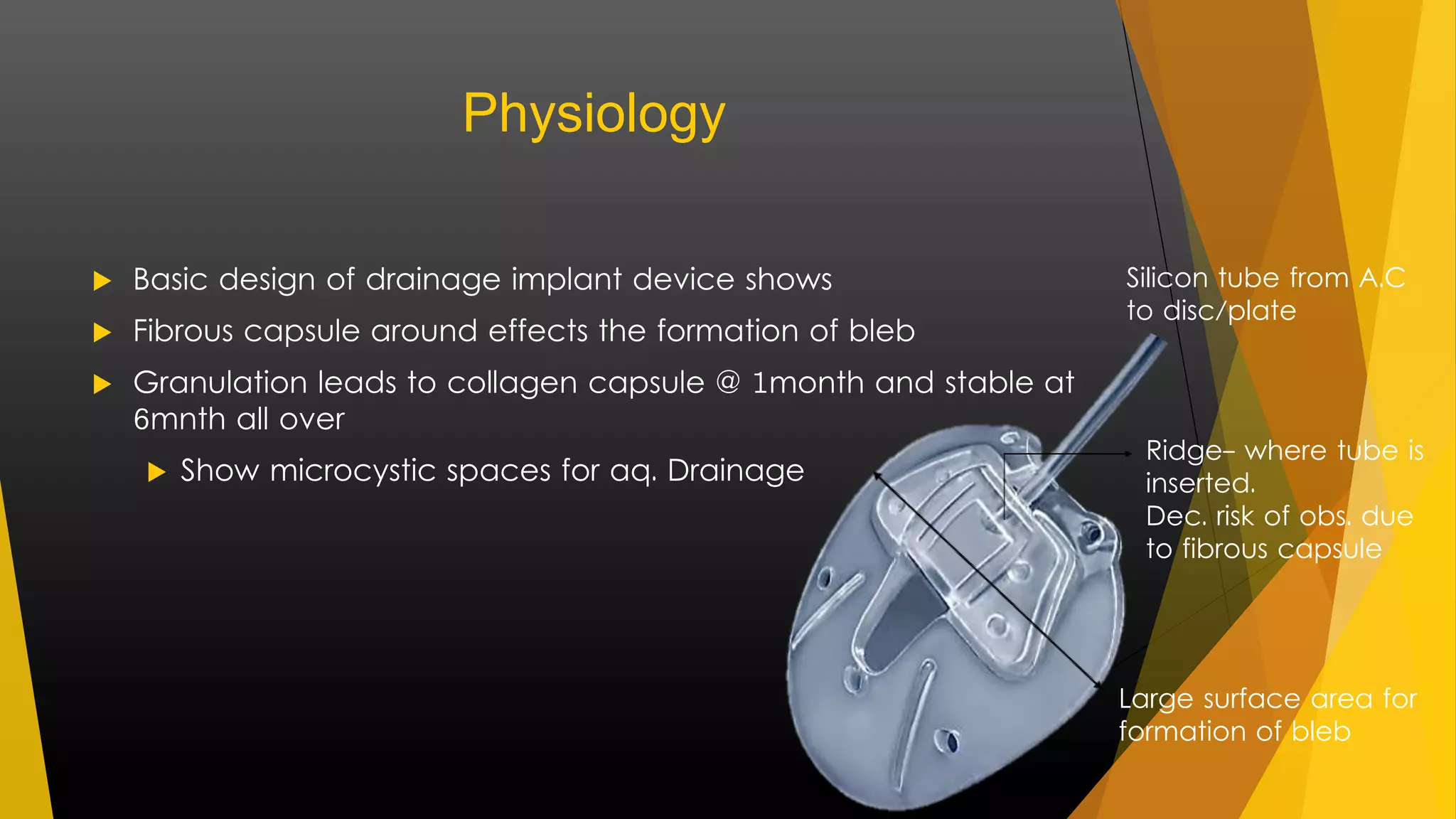
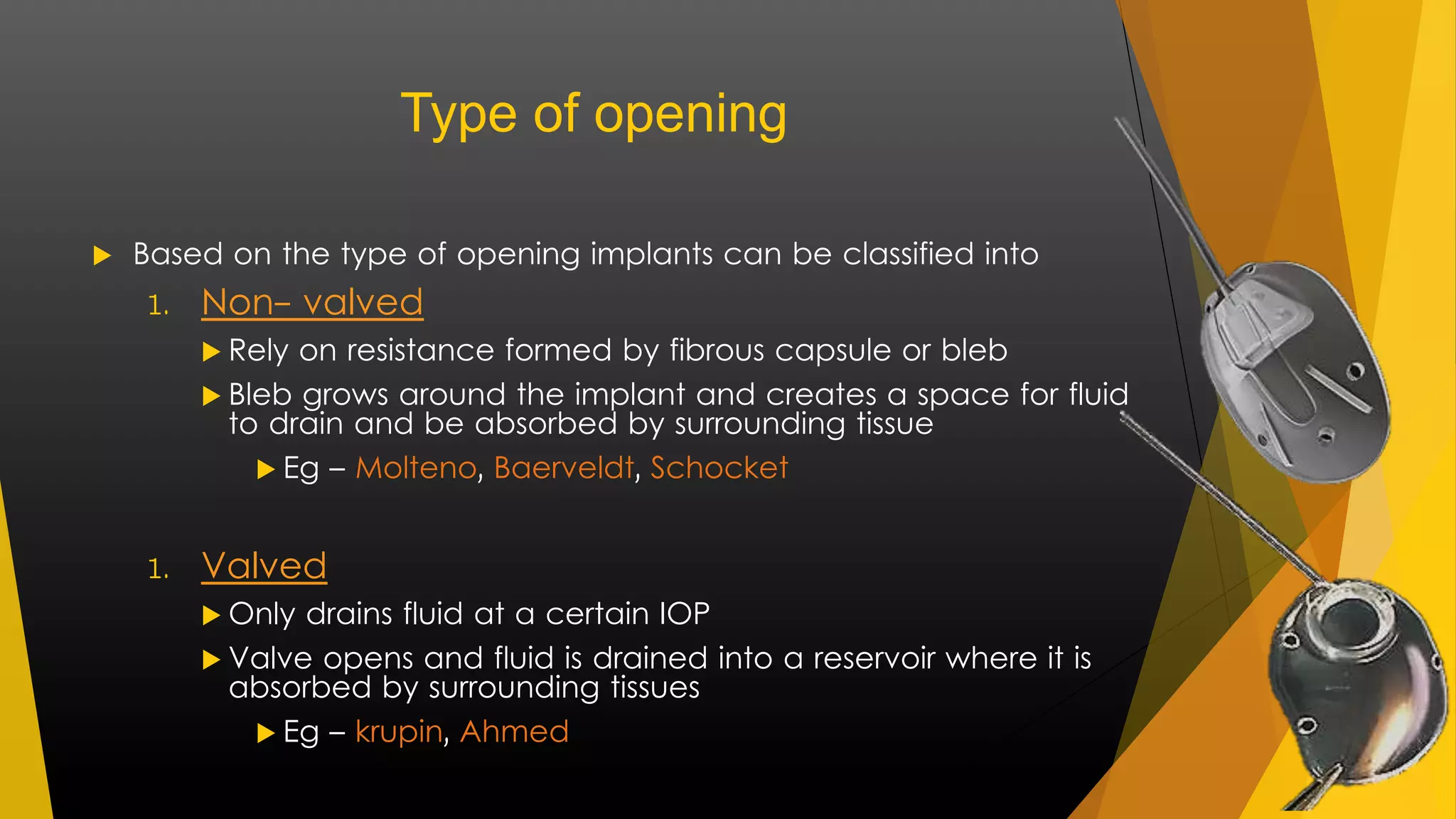
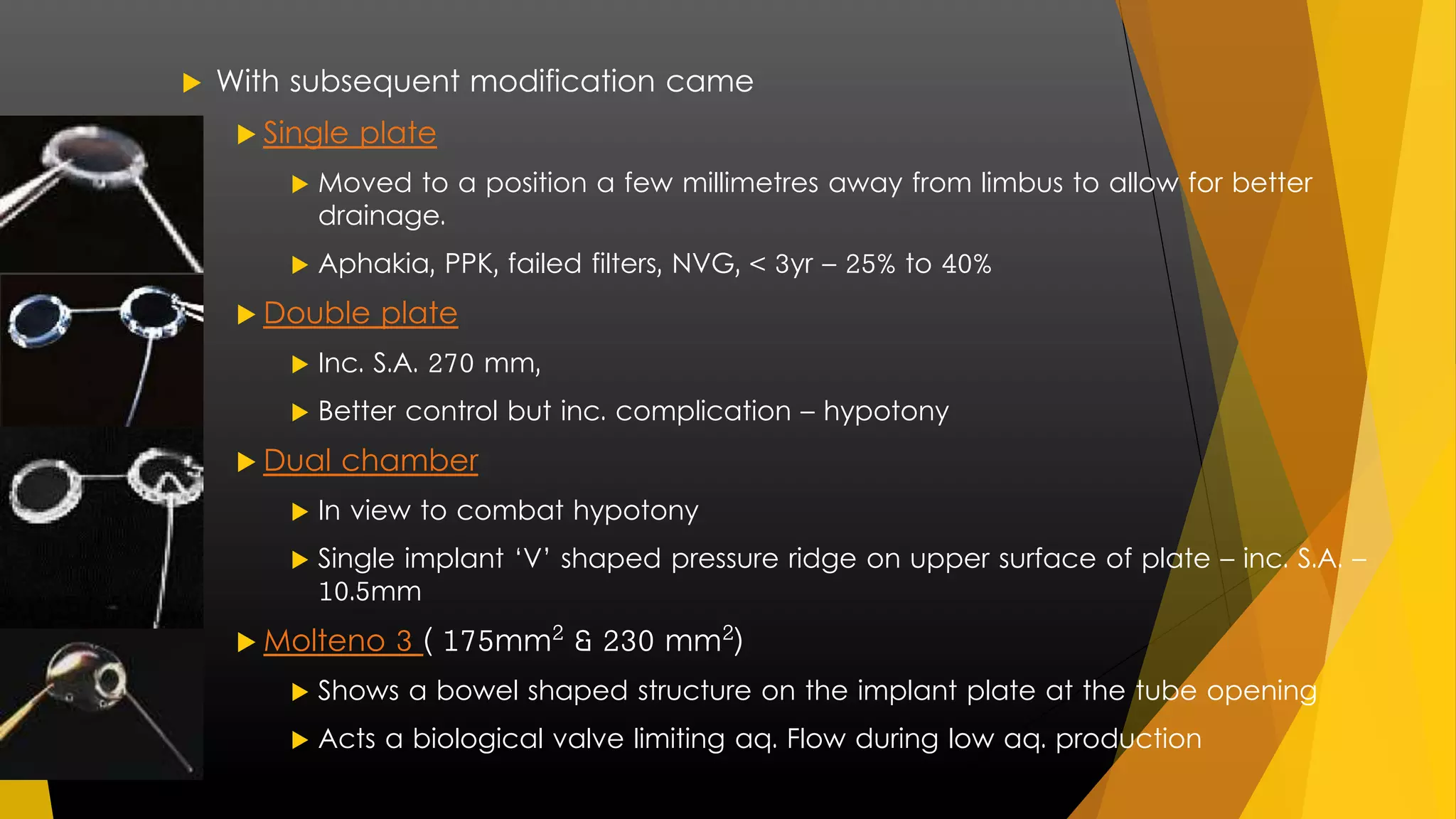
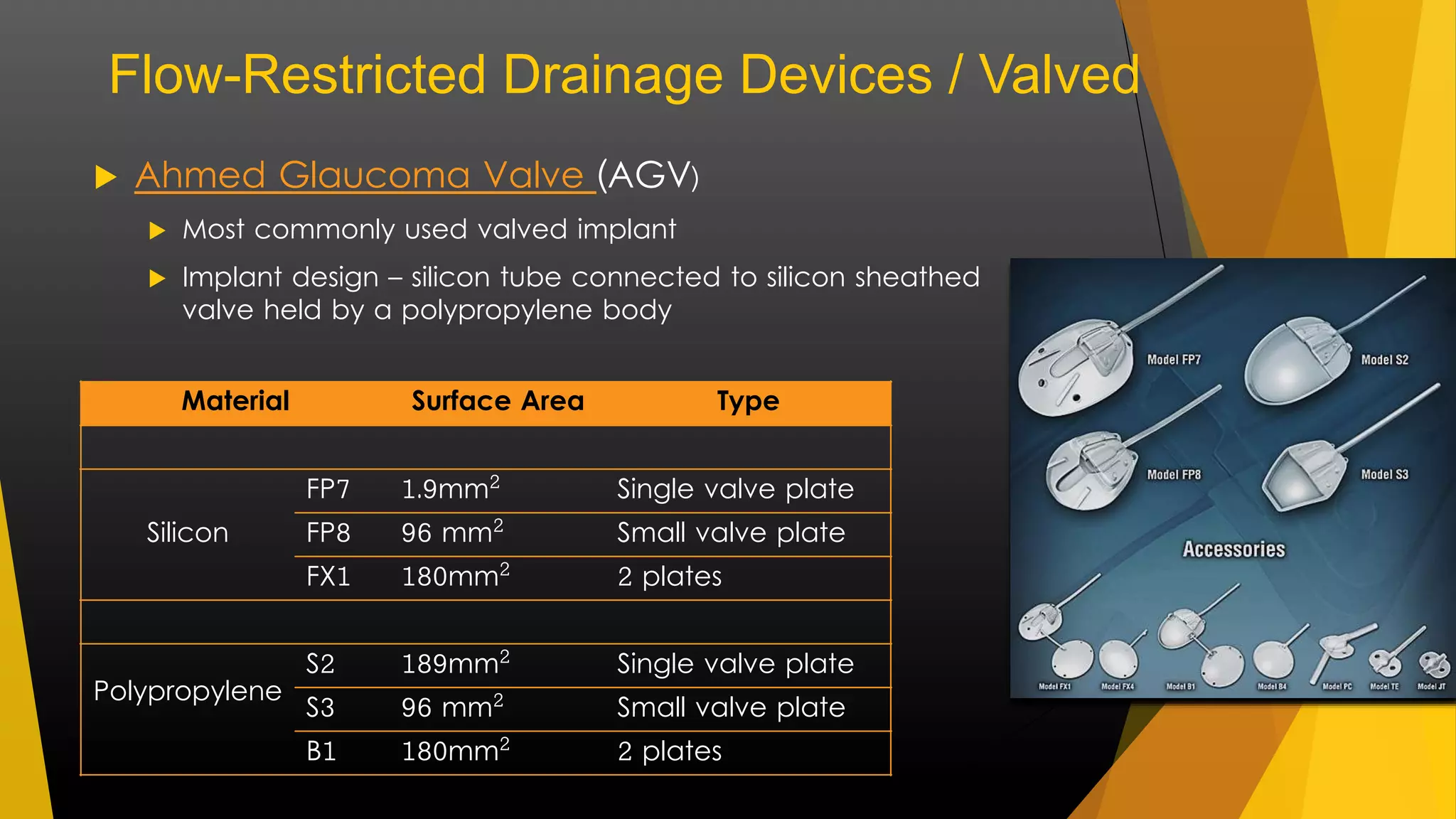
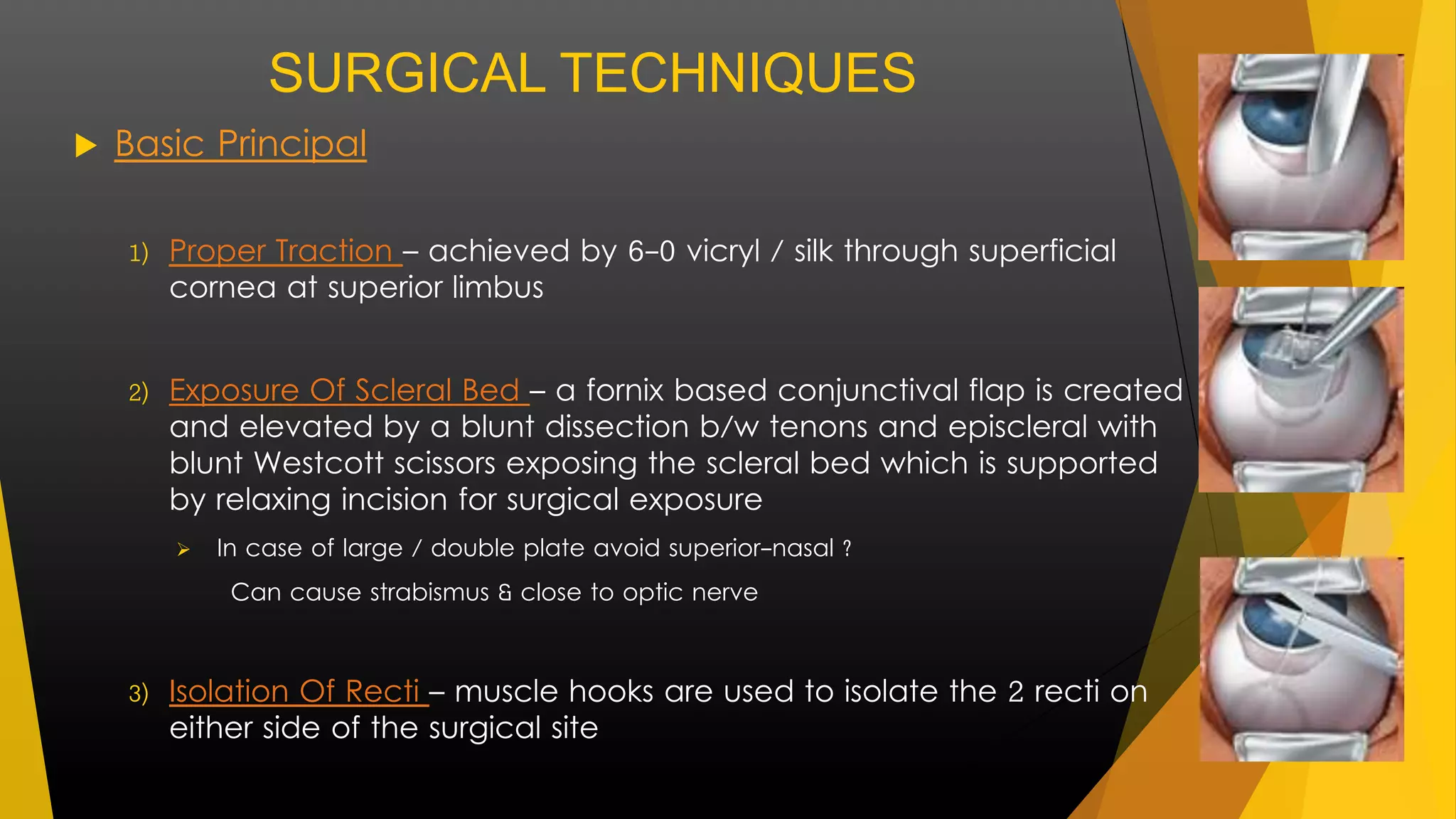
Glaucoma drainage devices (GDDs) provide an alternative pathway for aqueous humor outflow and are used to treat refractory glaucoma. The document discusses the history, design, and types of various GDDs including non-valved devices like Baerveldt and Molteno implants as well as valved devices like the Ahmed Glaucoma Valve. The key components, materials, and surgical techniques for GDD implantation are also summarized.