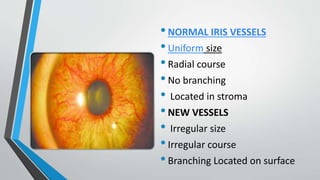
New Neovascular Glaucoma is a secondary glaucoma caused by the growth of new blood vessels on the iris and in the anterior chamber angle. It is usually caused by chronic retinal ischemia from conditions like diabetic retinopathy or central retinal vein occlusion. The new vessels cause the intraocular pressure to rise, damaging the optic nerve. Treatment involves panretinal photocoagulation to reduce the stimulus for new vessel growth, intravitreal anti-VEGF drugs to inhibit angiogenesis, glaucoma medications, and sometimes filtering surgeries or cyclodestructive procedures if pressure cannot be controlled through other means. The goal is to lower pressure to prevent further optic nerve damage while also treating the underlying cause of the retinal ischemia.