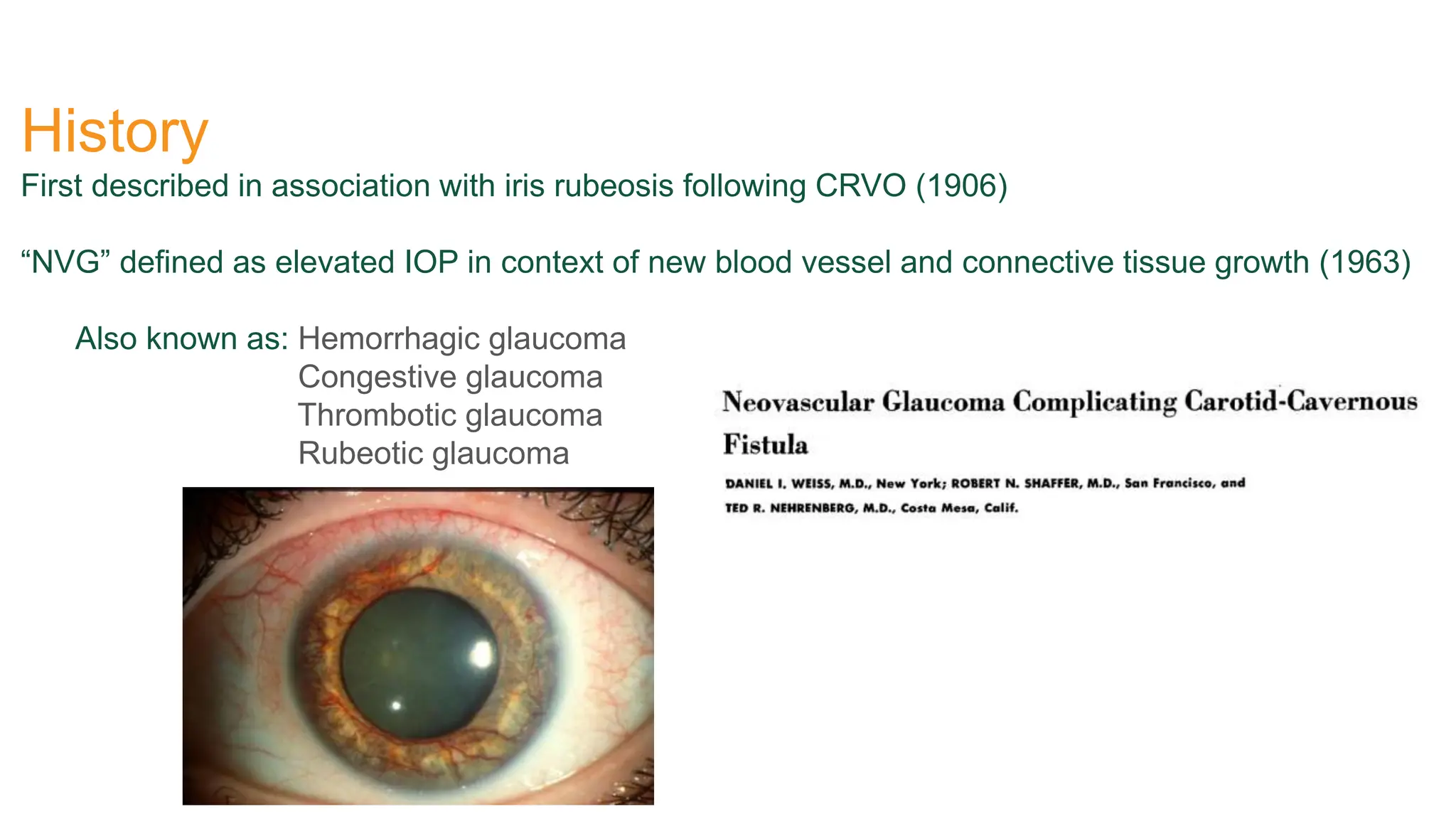
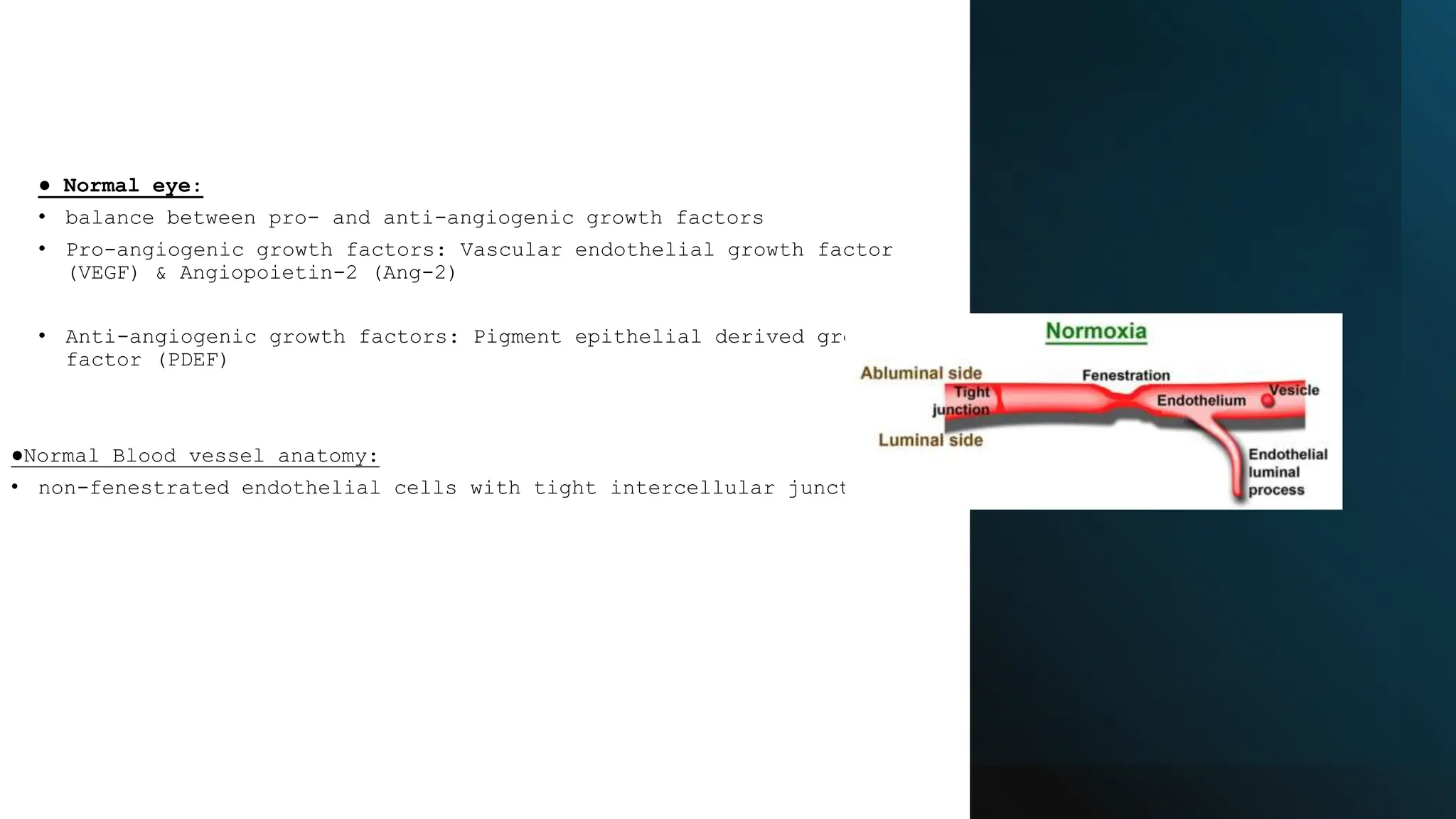
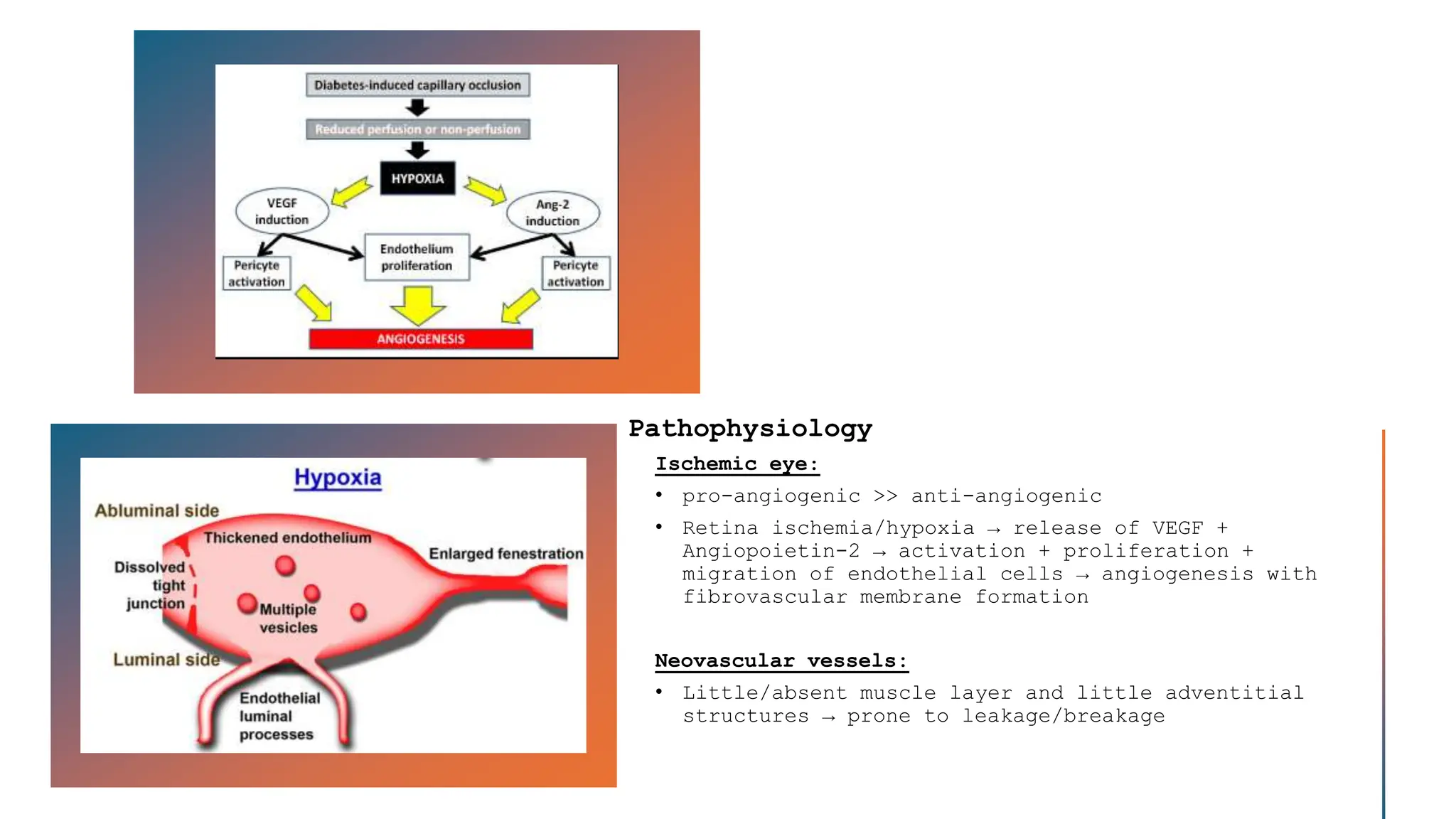
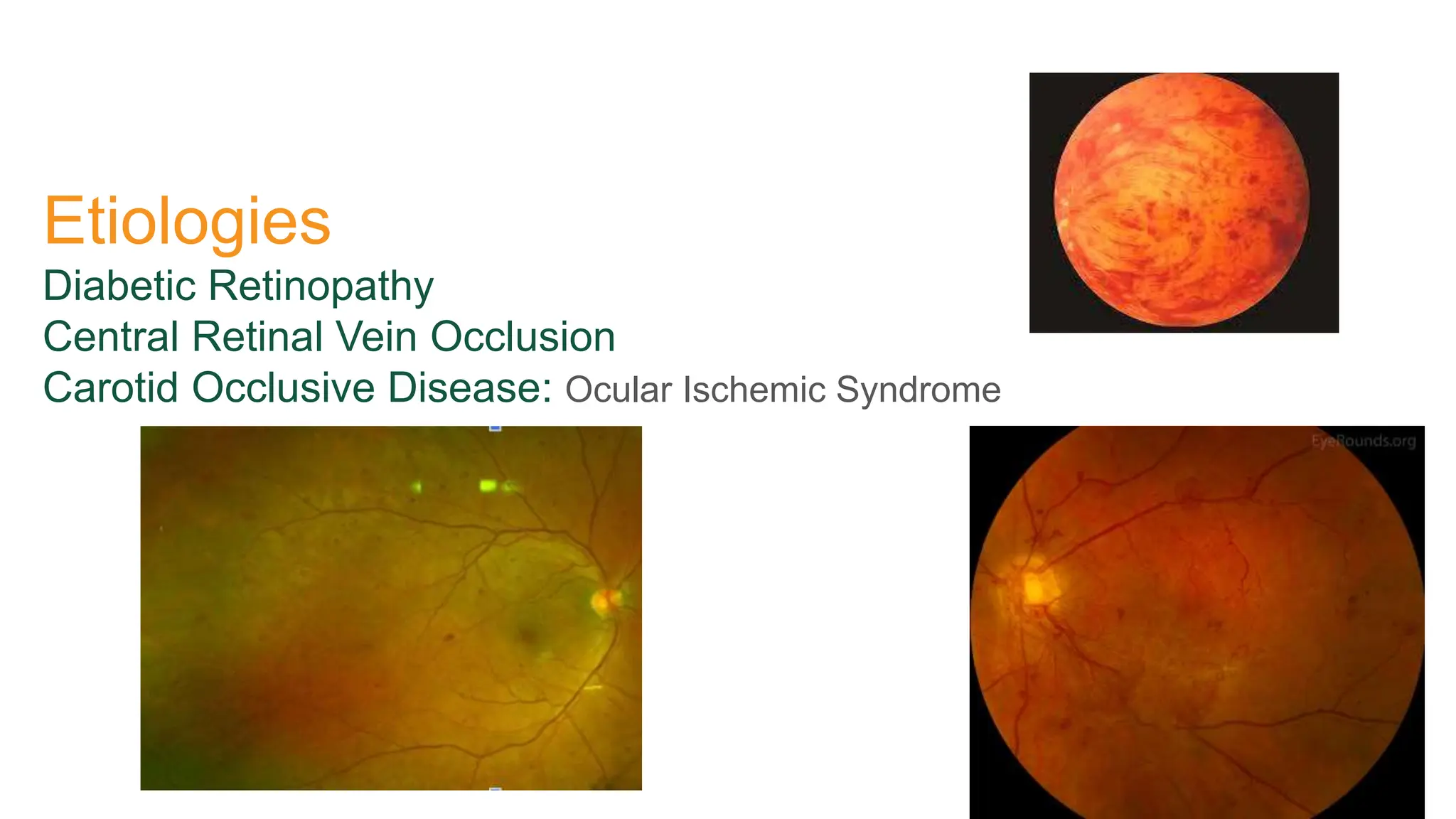
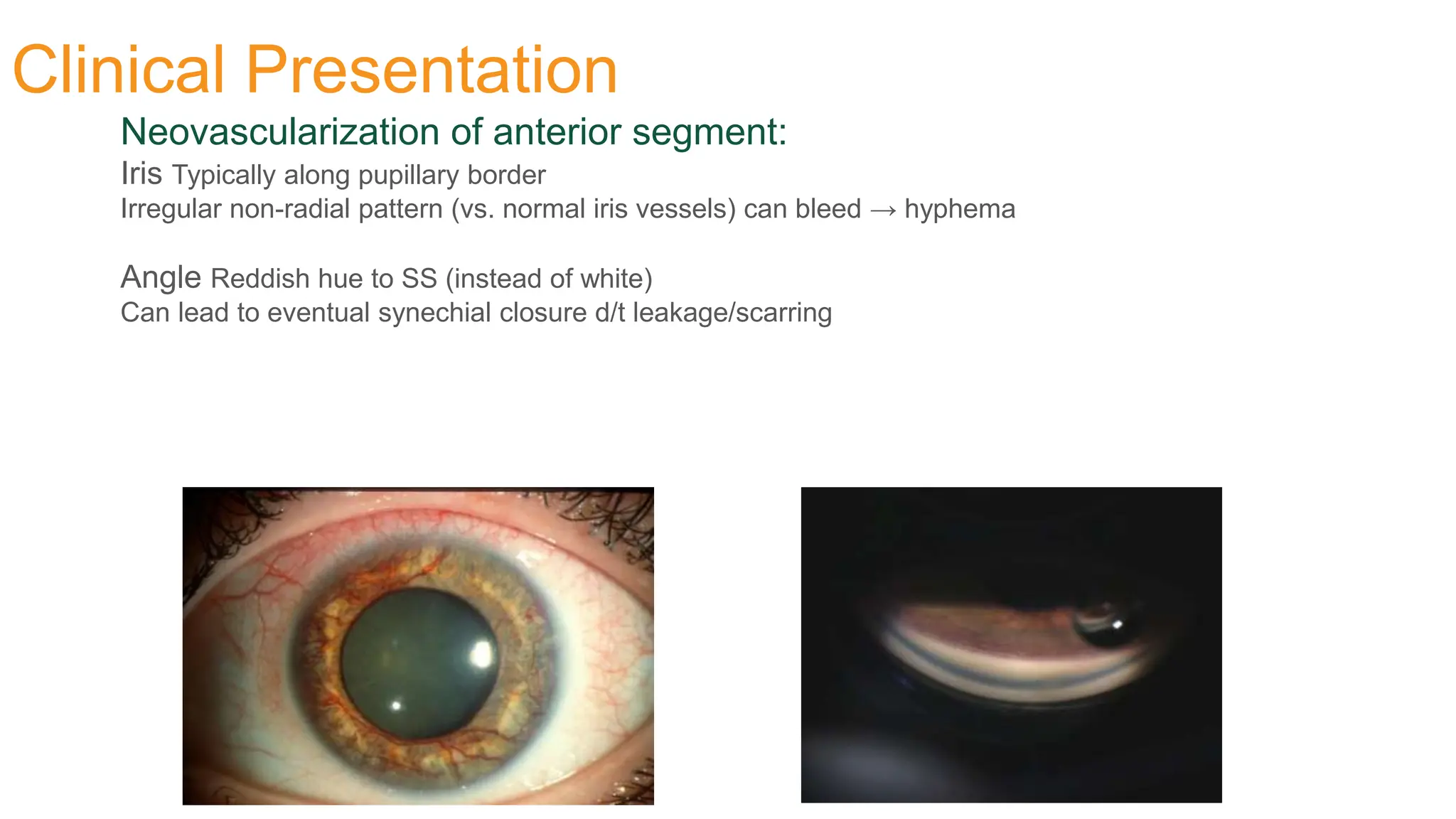
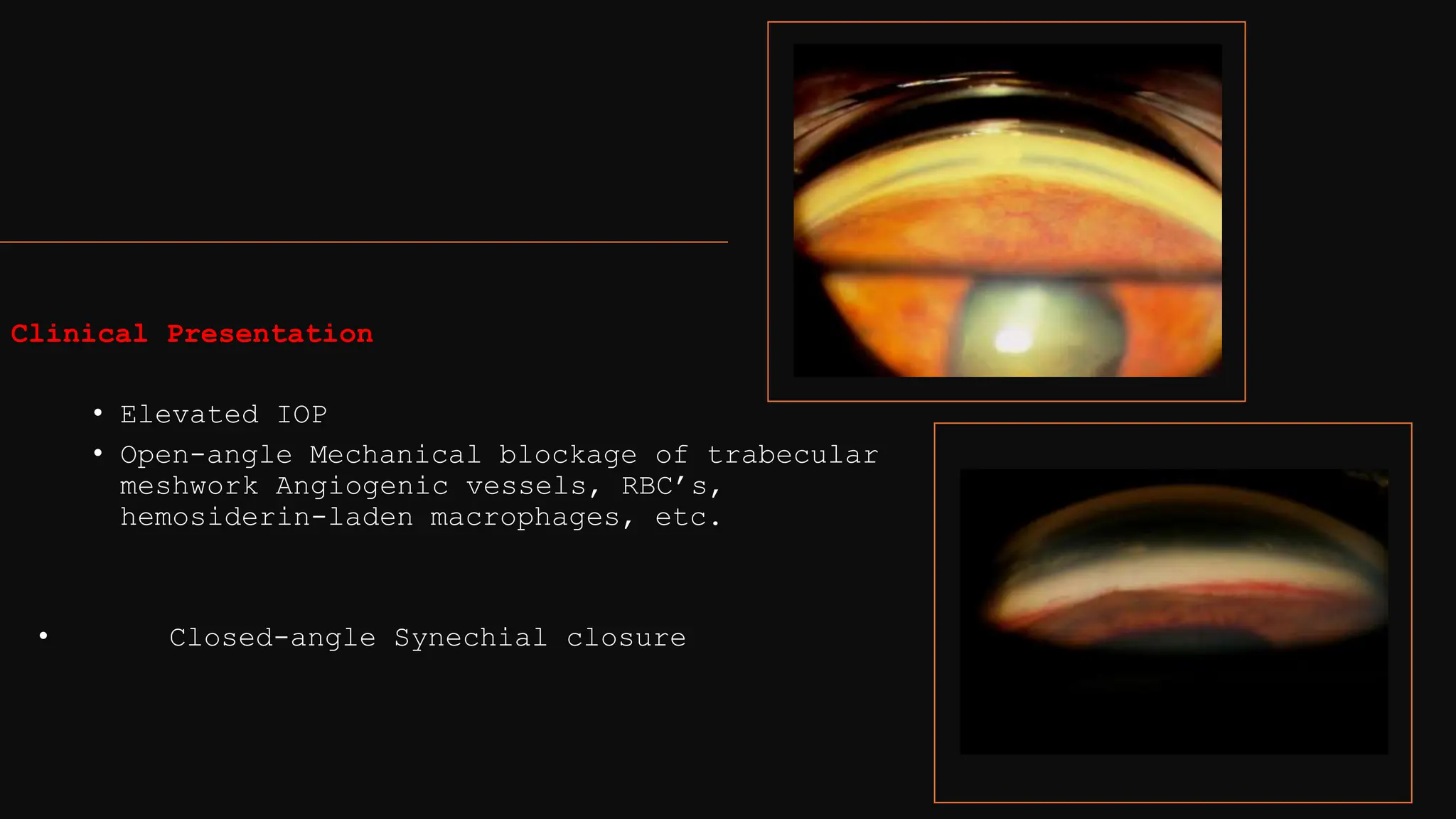
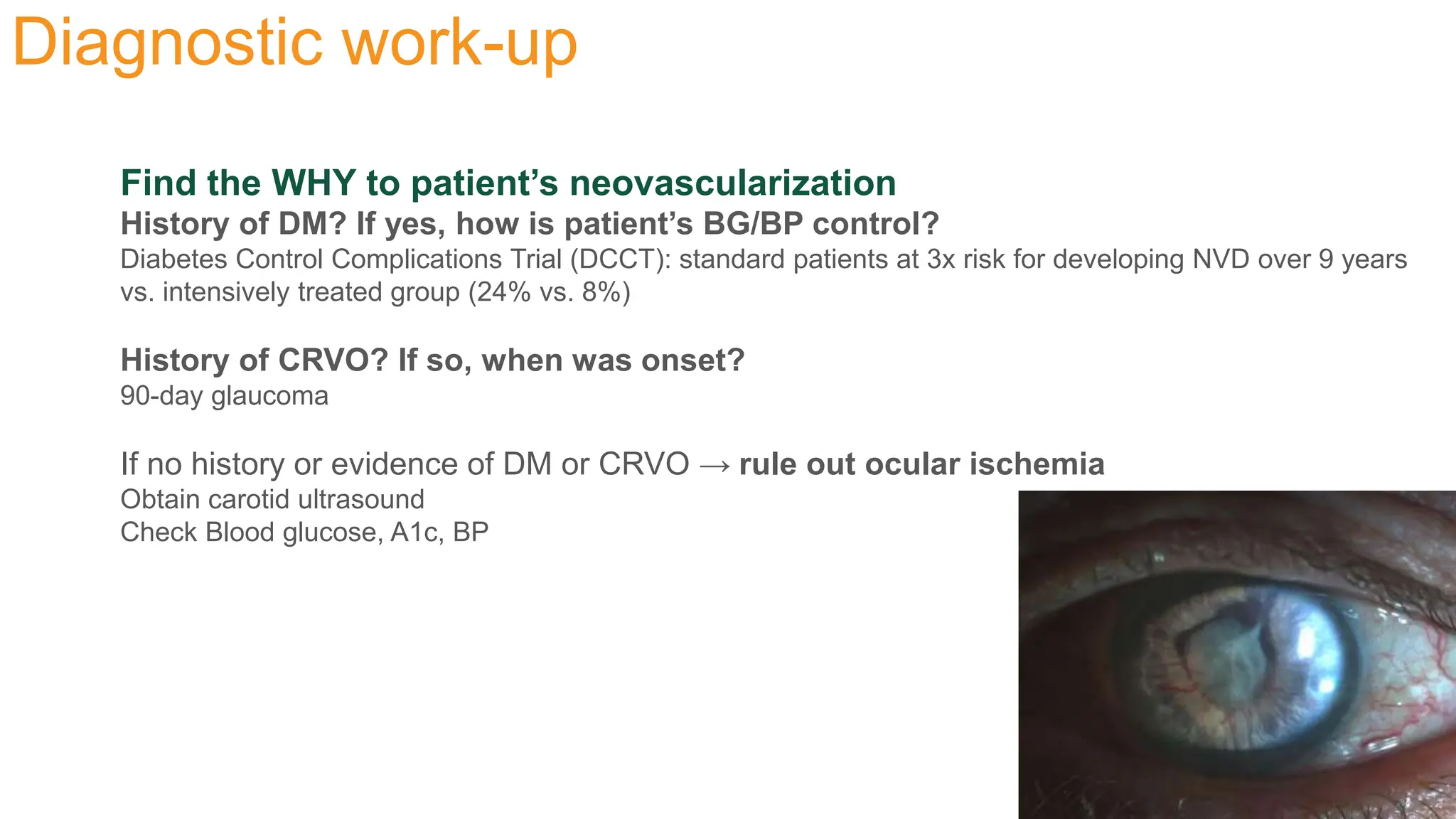
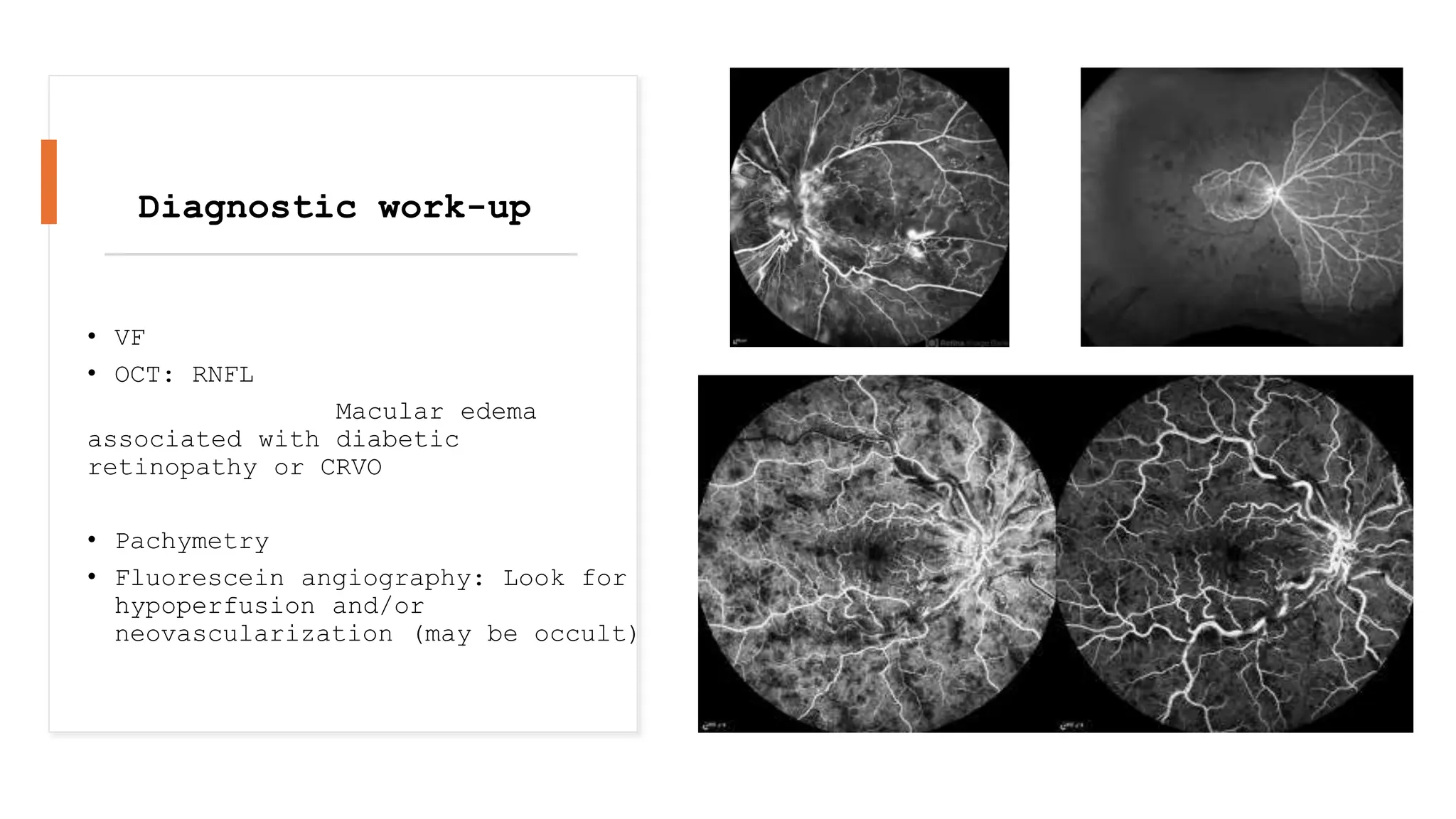
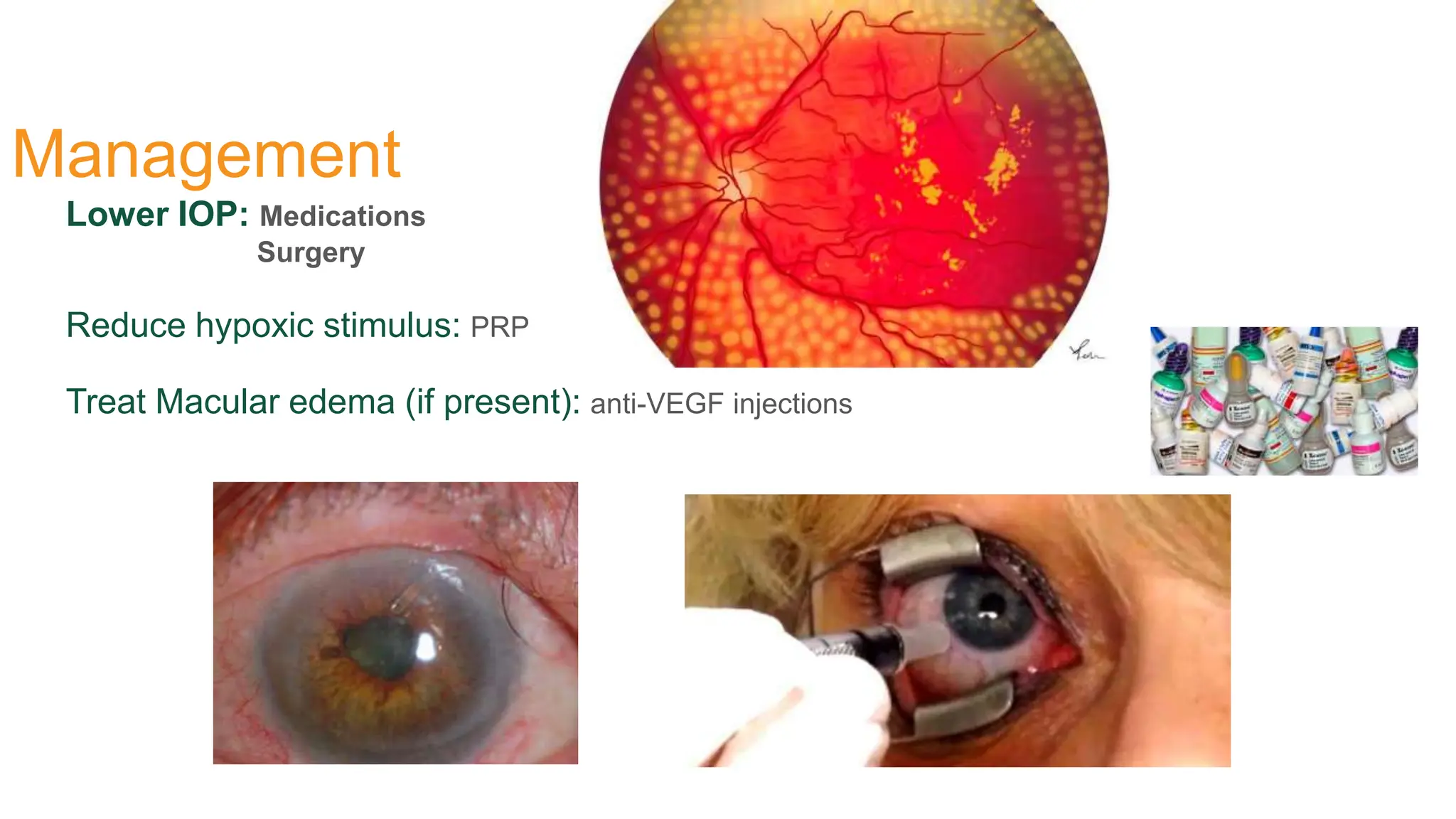
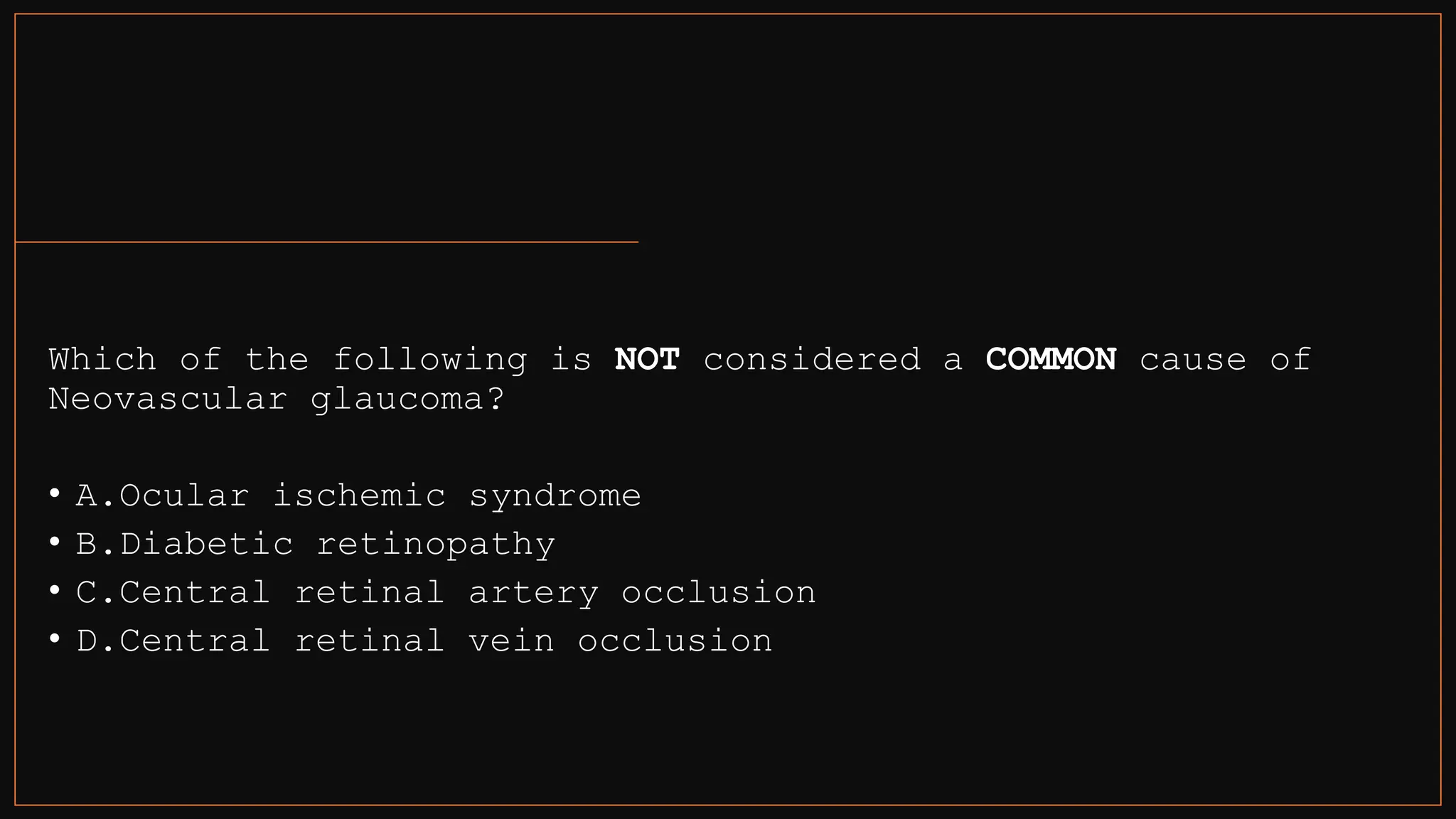
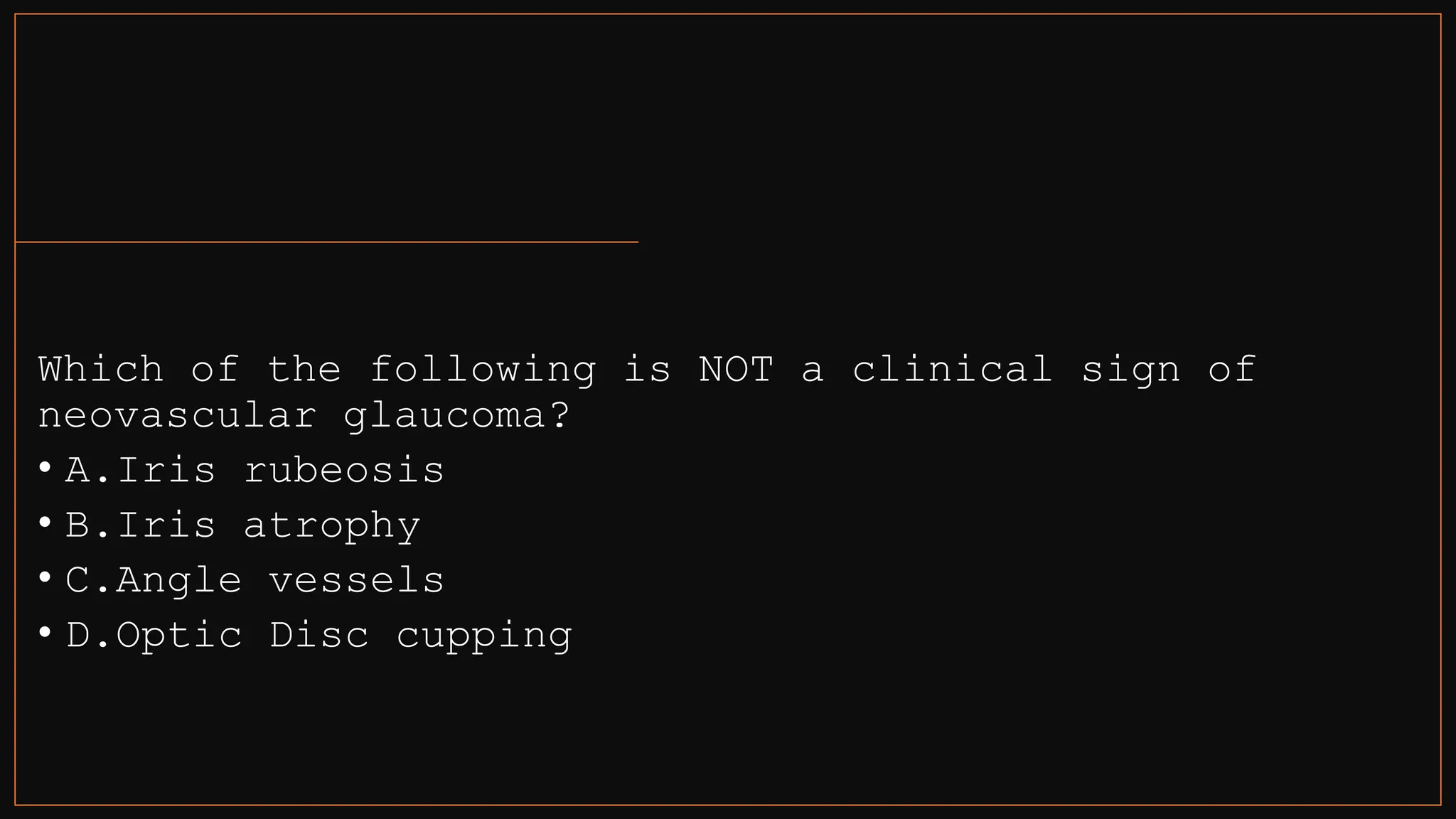
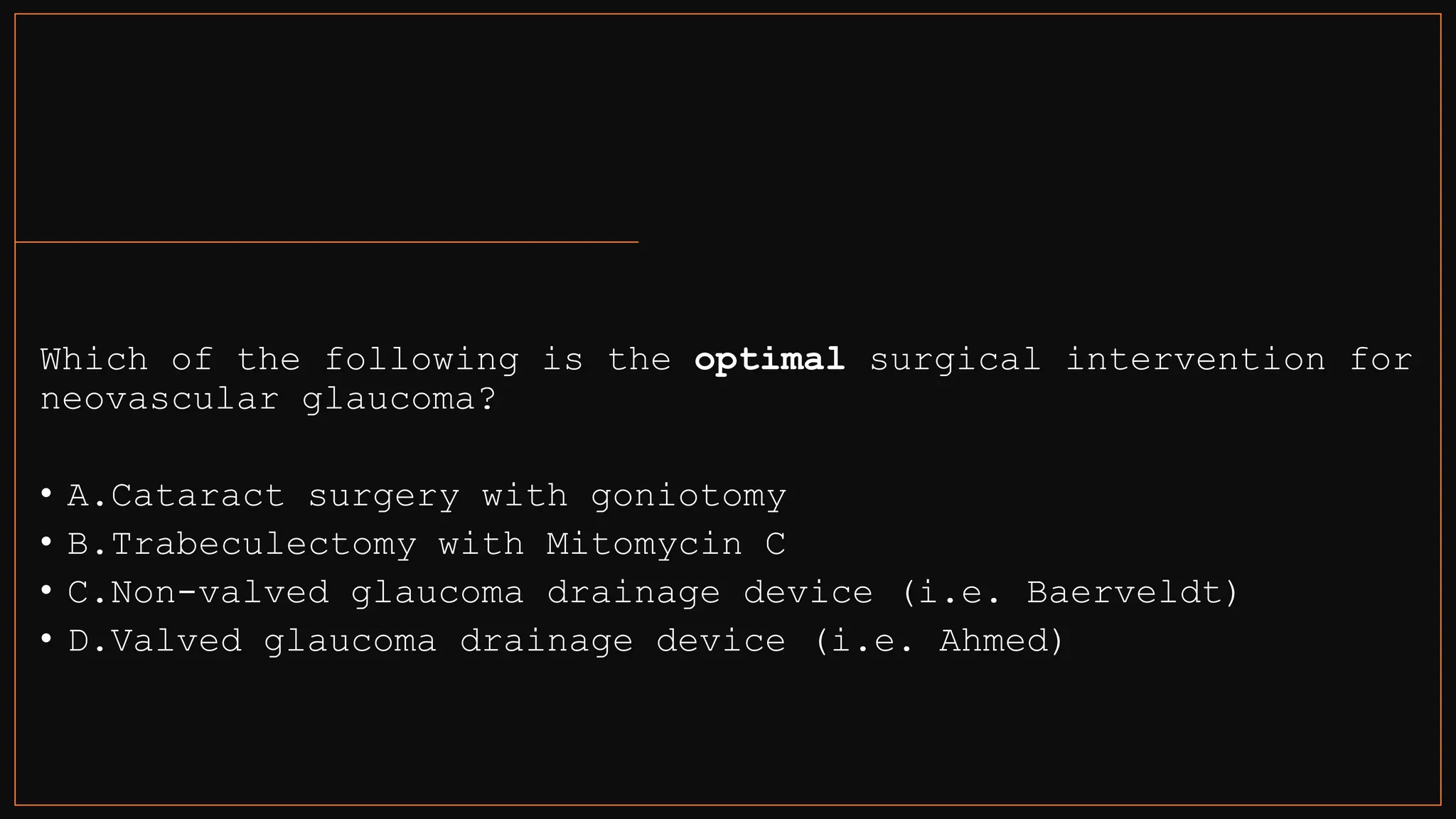
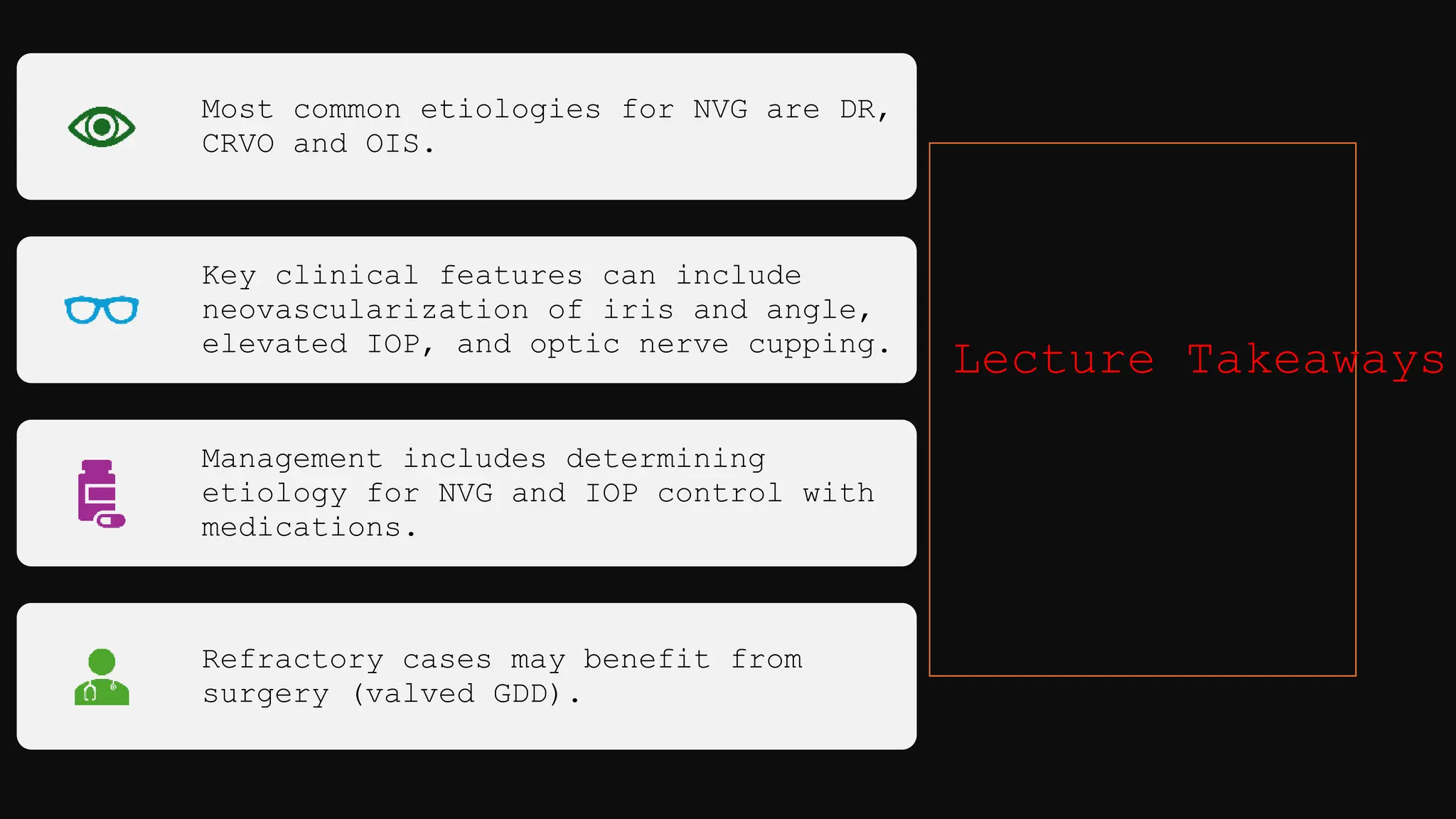
Neovascular glaucoma (NVG) is characterized by elevated intraocular pressure due to new blood vessel growth associated with conditions like diabetic retinopathy and central retinal vein occlusion. Key clinical features include neovascularization of the iris and angle, elevated IOP, and optic nerve cupping, with management focusing on identifying the underlying cause and controlling IOP through medication and potentially surgery. Refractory cases may require valved glaucoma drainage devices for effective treatment.