Vascular disorders of the retina can cause vision loss or blindness if not properly treated. The document discusses several types of vascular disorders:
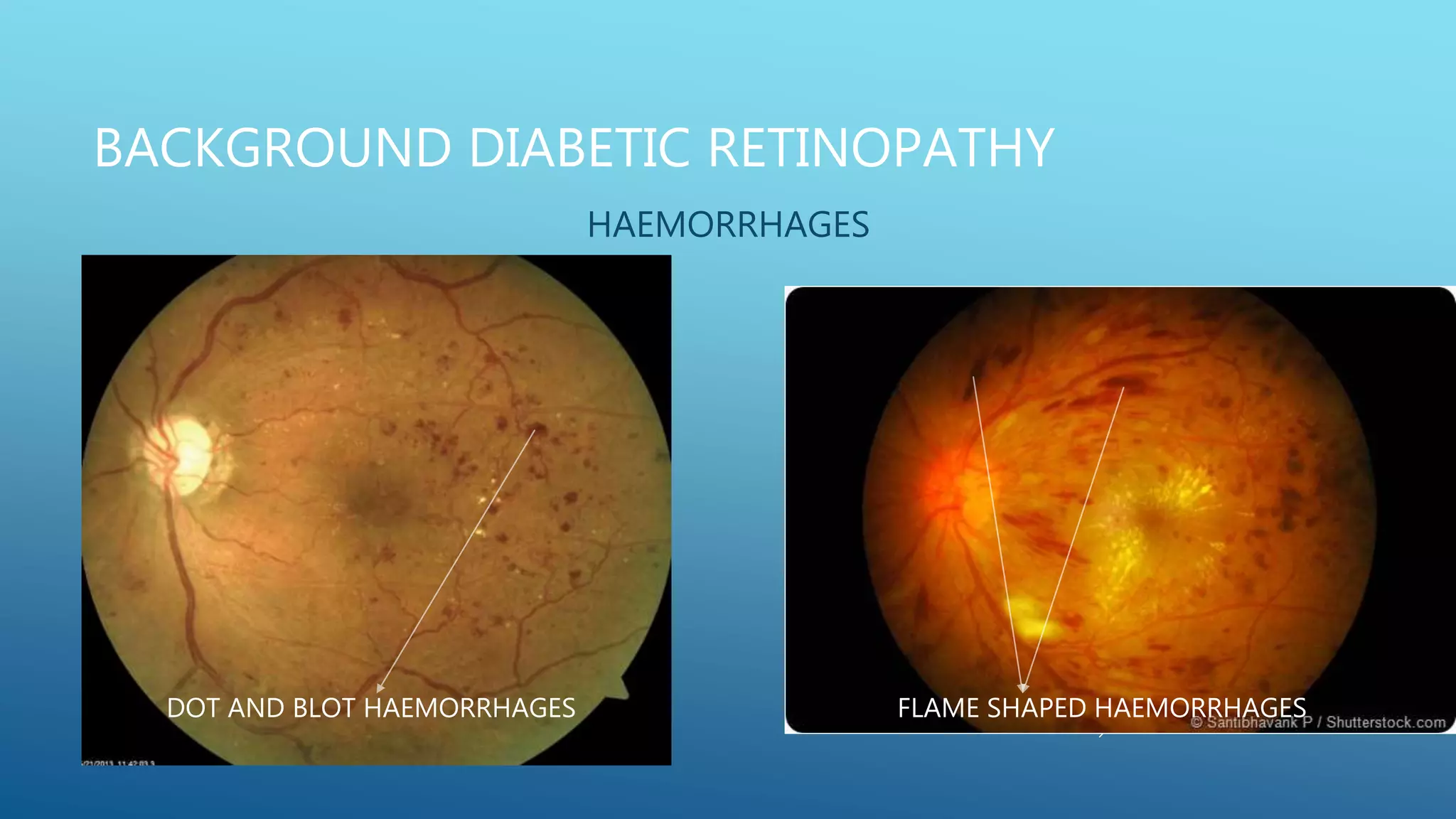
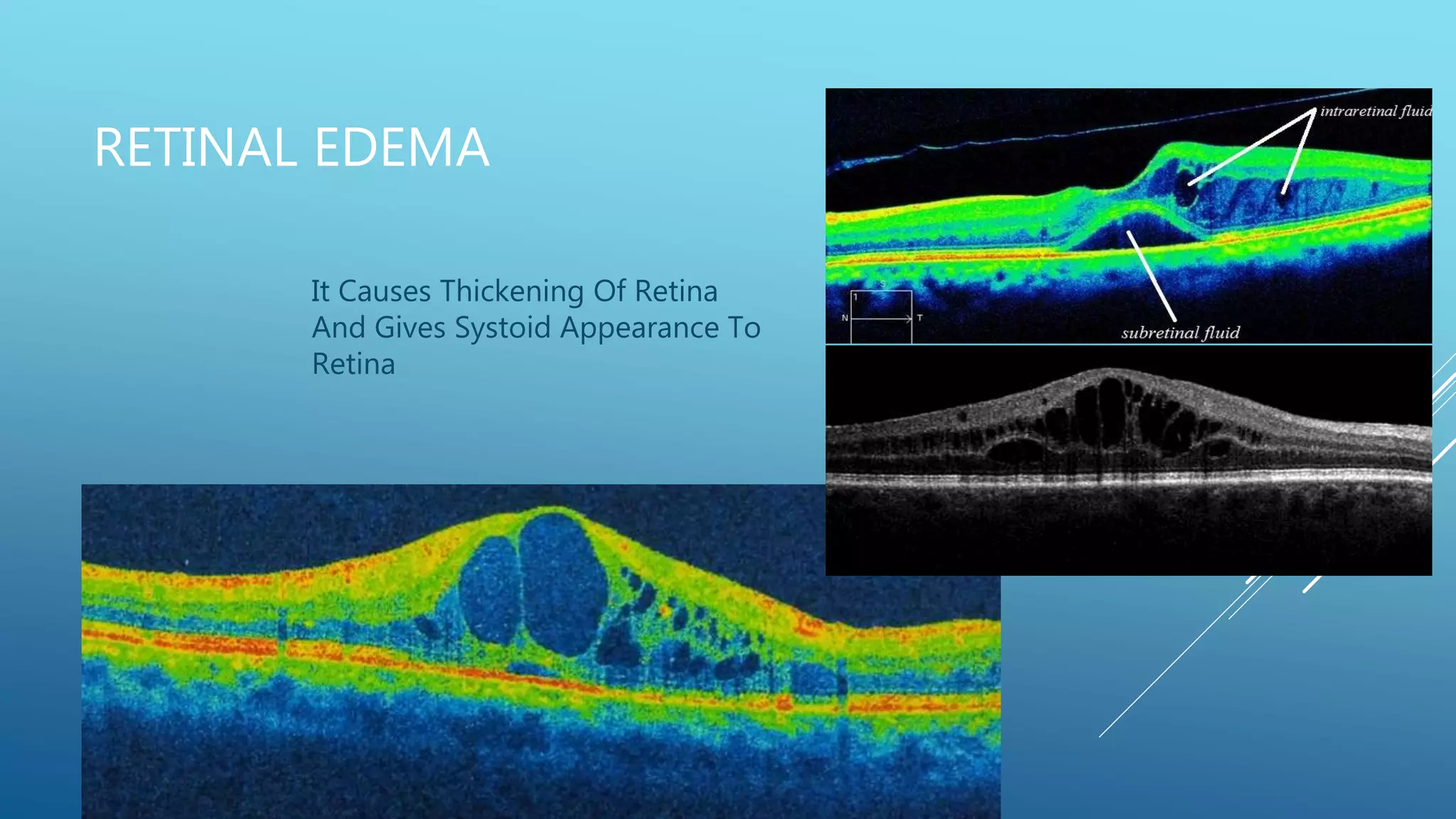
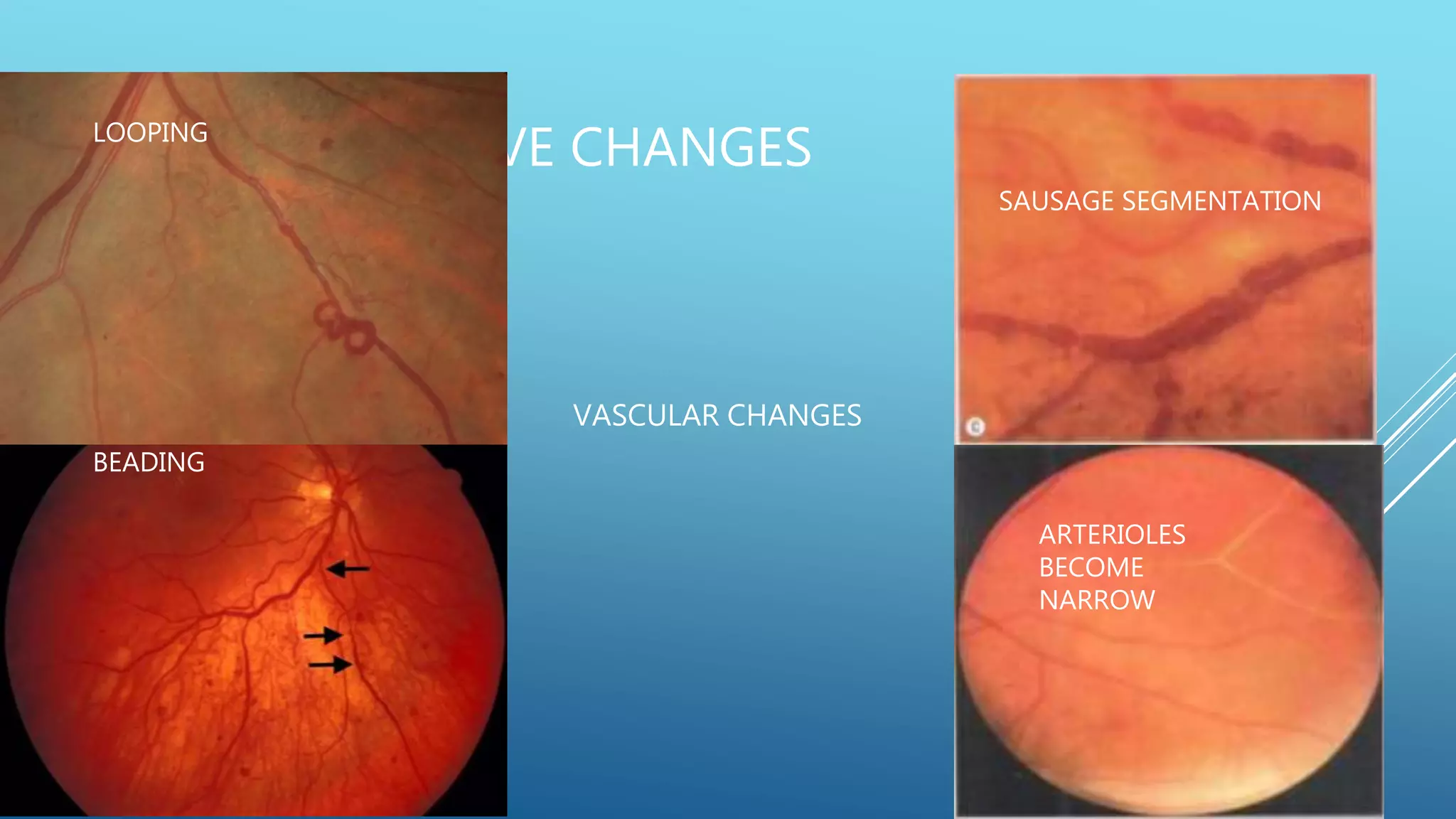
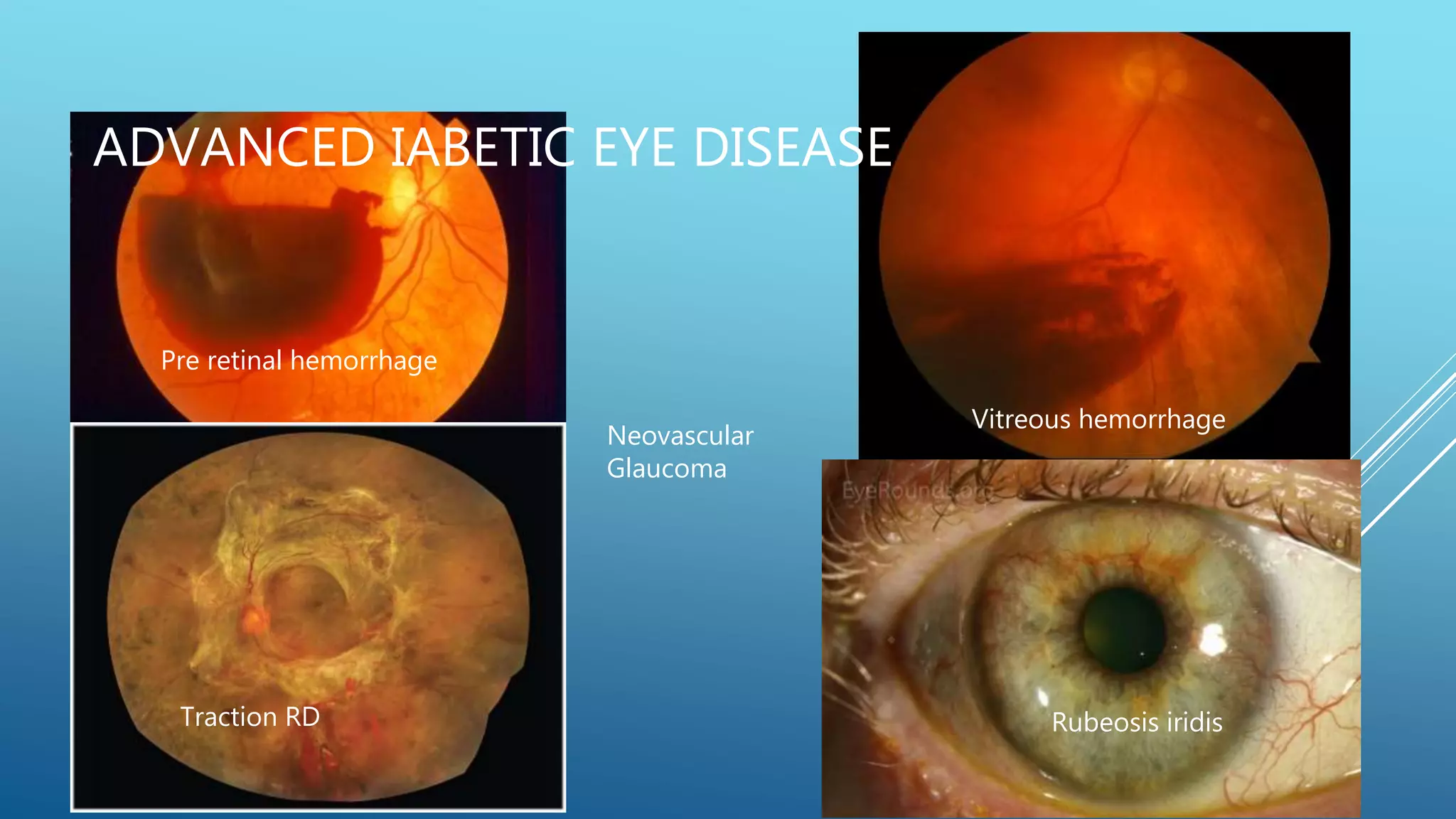
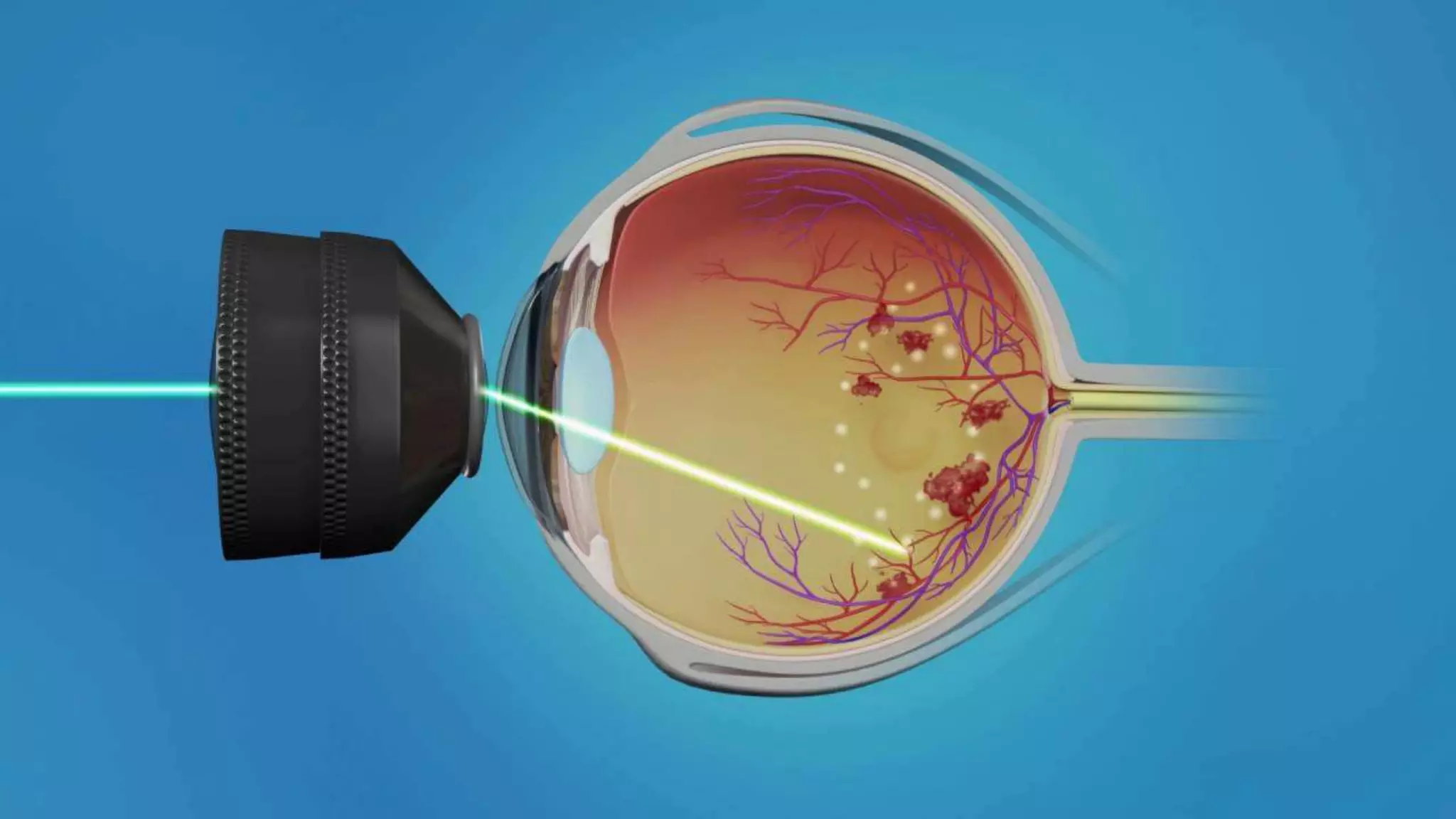
1. Diabetic retinopathy, which affects nearly all patients with long-standing diabetes and is a leading cause of vision loss. It involves microaneurysms, hemorrhages, hard exudates, and new blood vessel growth if proliferative. Laser treatment and anti-VEGF injections can help treat it.
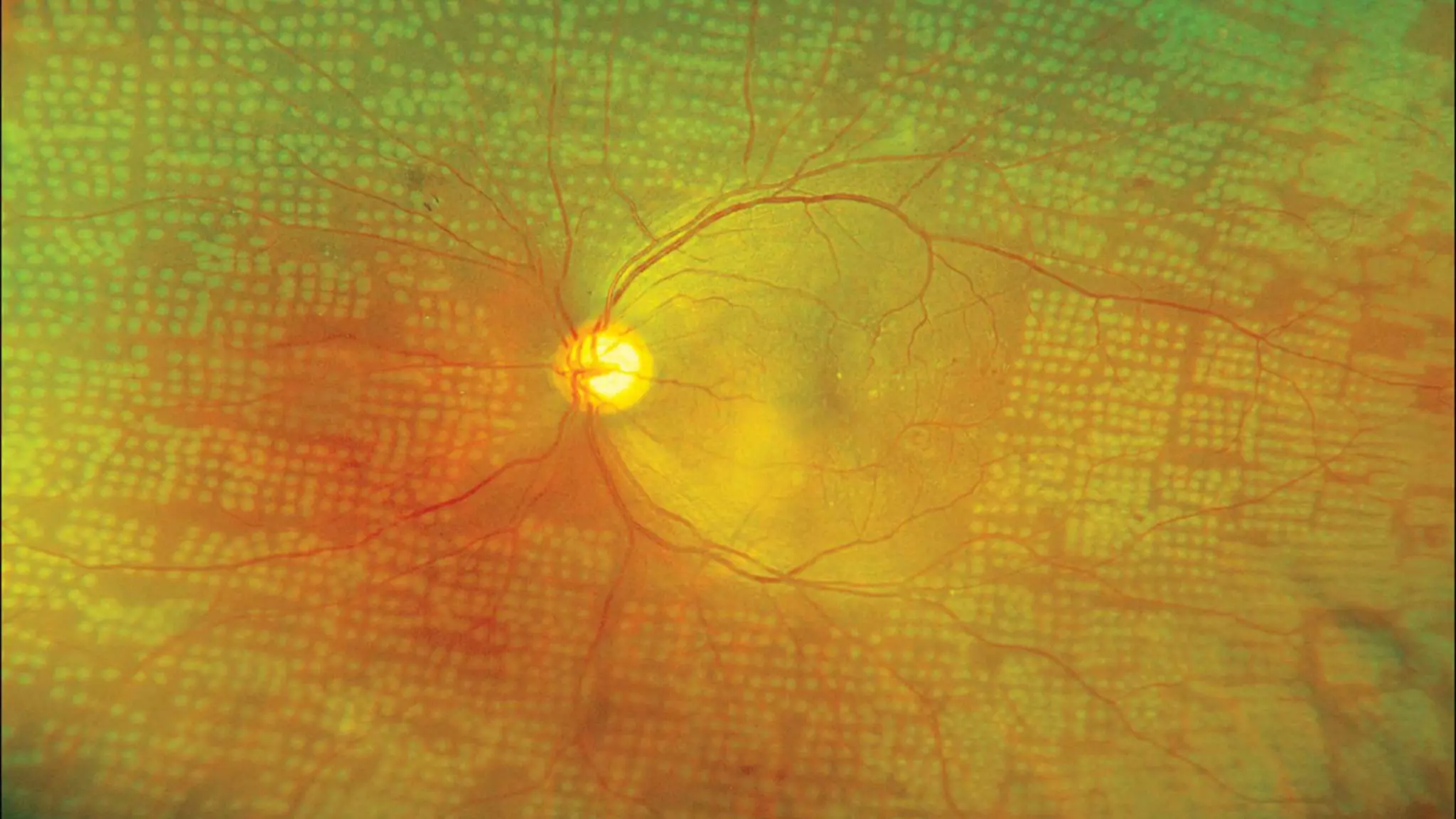
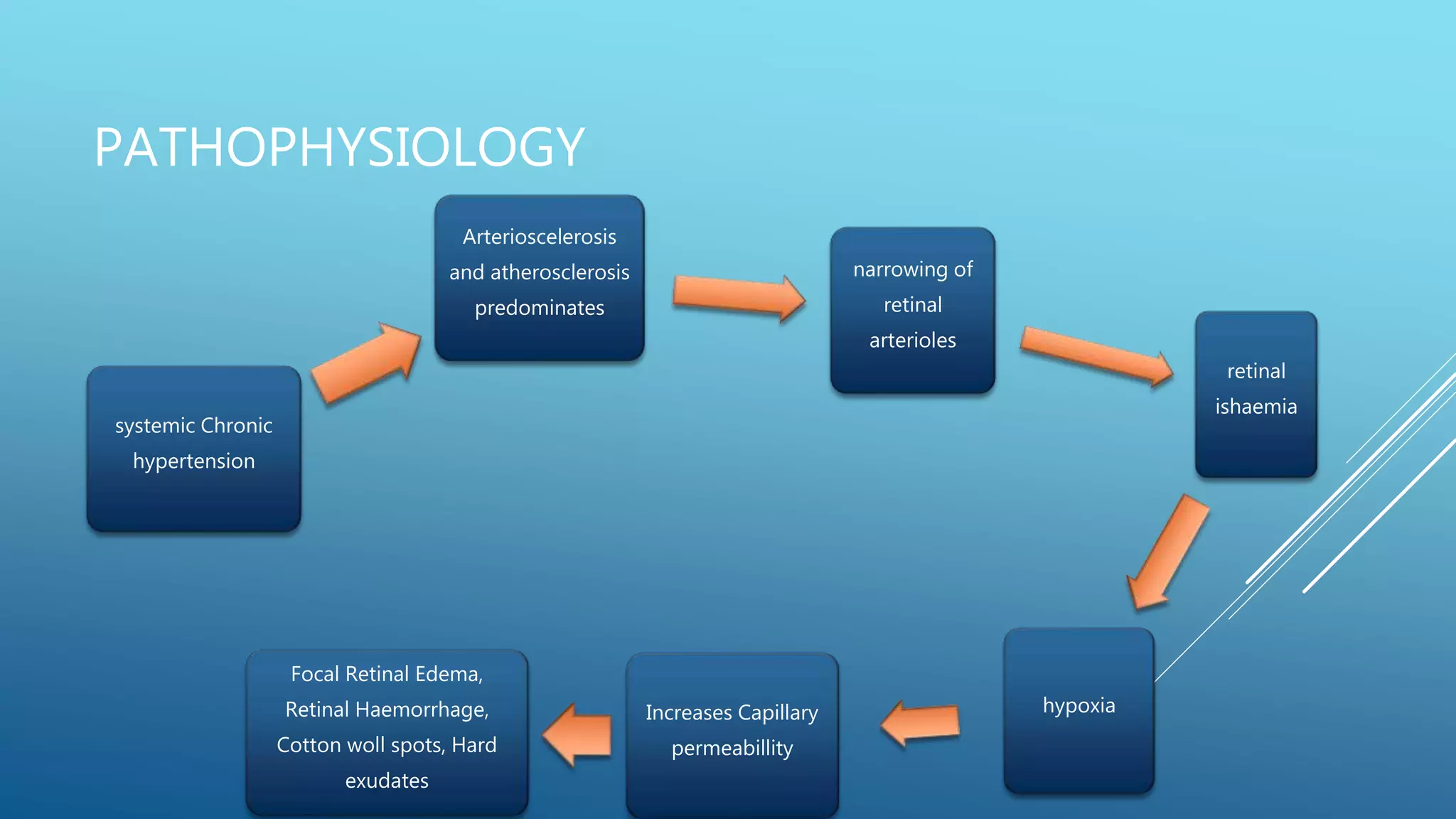
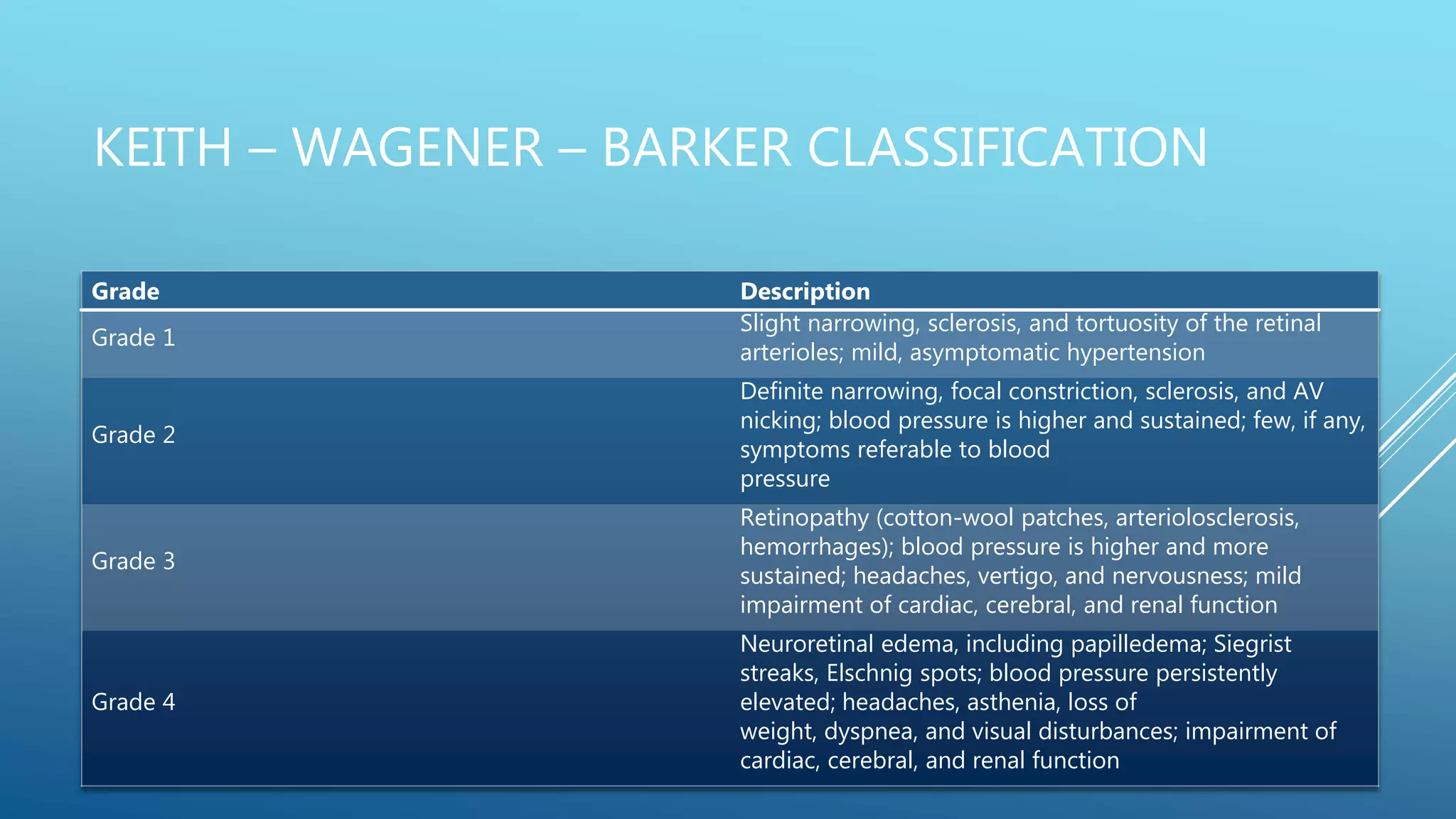
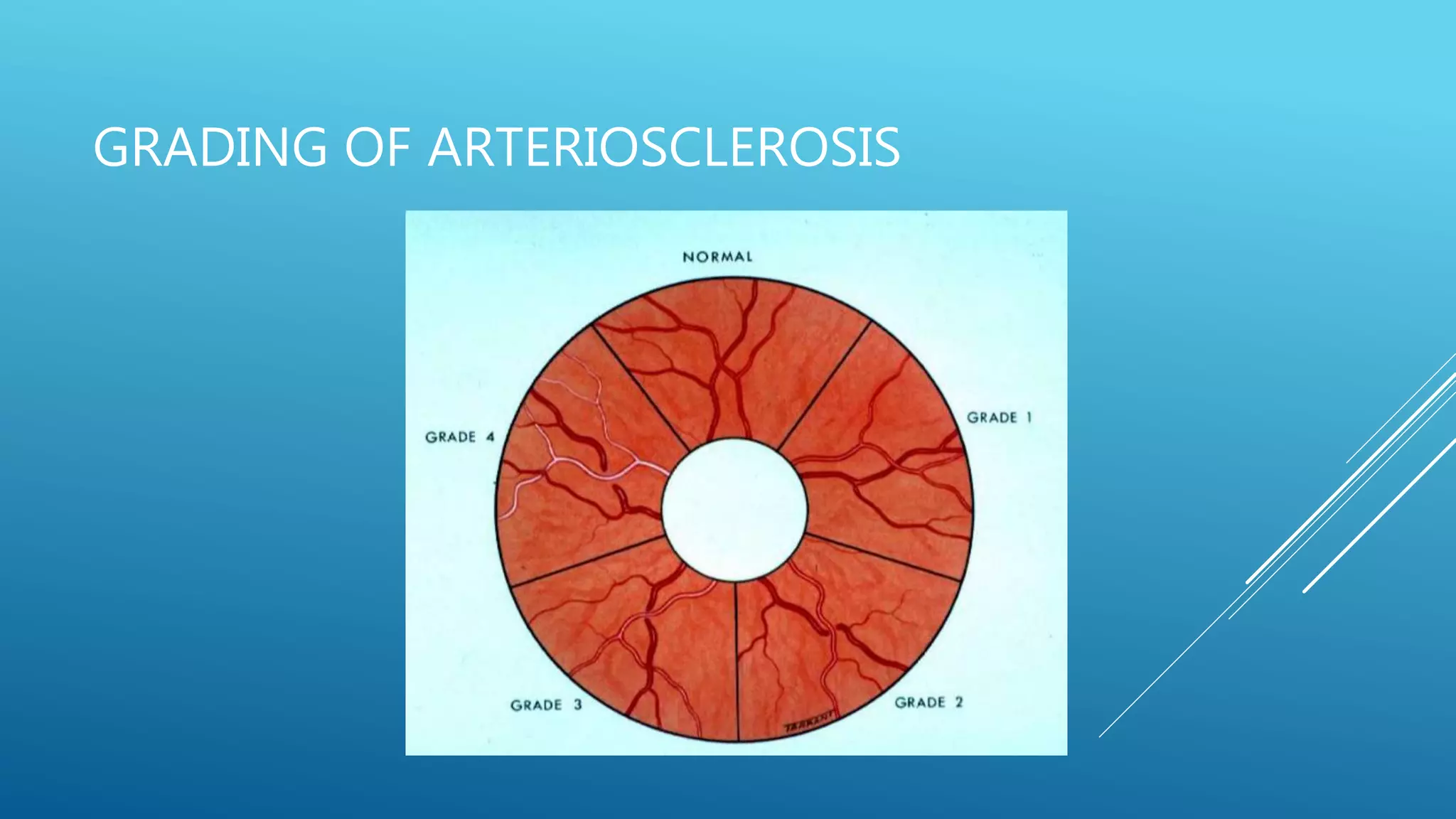
2. Hypertensive retinopathy results from high blood pressure and involves arteriolar narrowing, hemorrhages, cotton wool spots, and exudates. Grading systems describe the severity.
3. Retinal vein oc