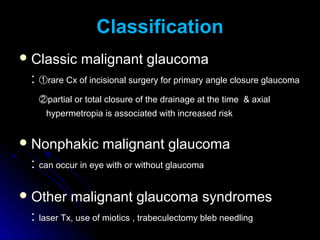
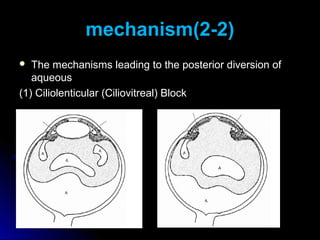
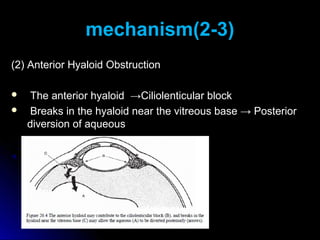
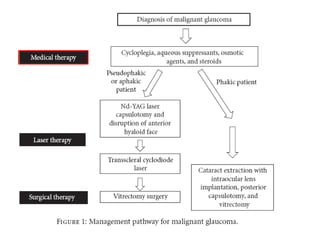
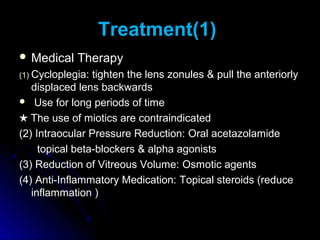
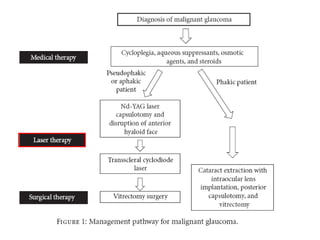
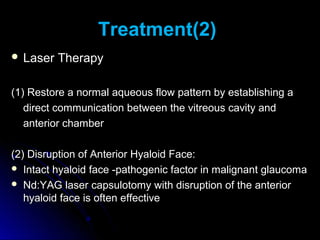
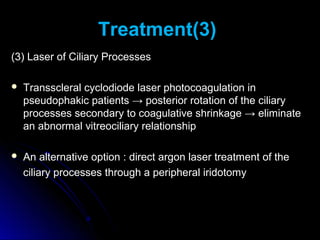
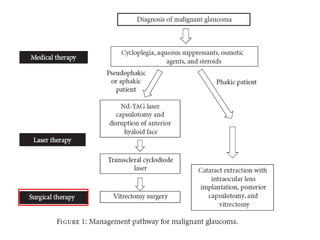
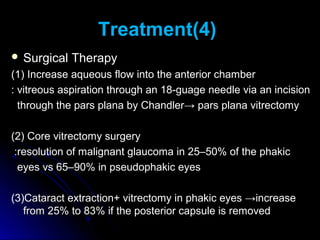
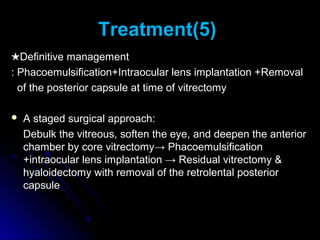
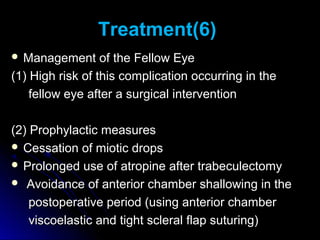
Classic malignant glaucoma is a rare complication of incisional surgery for angle-closure glaucoma where the anterior chamber shallows due to forward movement of the iris-lens diaphragm despite increased intraocular pressure. It can occur in eyes with or without glaucoma and may be triggered by laser treatment, miotics, or trabeculectomy. Treatment involves reducing pressure and vitreous volume medically or surgically with vitrectomy. Definitive management is phacoemulsification, intraocular lens implantation, and removal of the posterior capsule during vitrectomy.