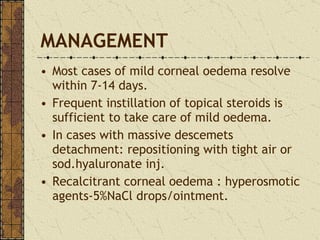
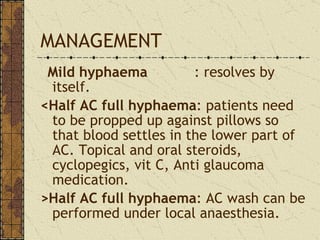
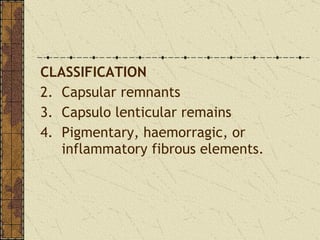
Early complications of intraocular lens (IOL) surgery include corneal edema, wound leak, shallow anterior chamber, hyphaema, retained lens matter, and uveitis. Late complications include posterior capsular opacification, cystoid macular edema, endophthalmitis, and retinal detachment. Post-operative endophthalmitis is a vision-threatening complication that is treated with topical, systemic, and intravitreal antibiotics along with steroids. Posterior capsular opacification occurs in 10-50% of cases due to proliferation of lens epithelial cells.