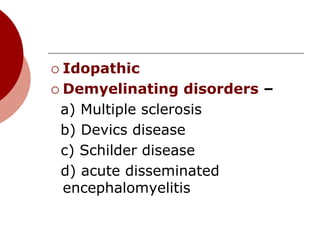
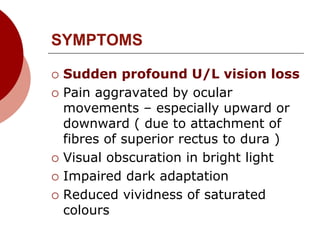
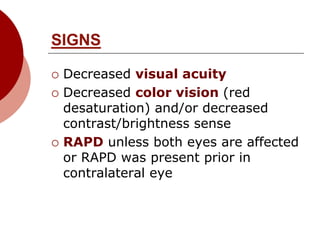
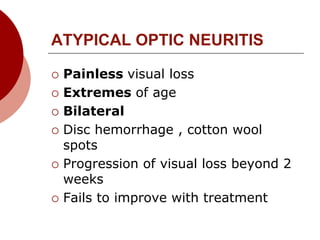
Optic neuritis is inflammation of the optic nerve that commonly presents as sudden, unilateral vision loss. It affects young females predominantly and is often the initial presentation of multiple sclerosis. Treatment with intravenous steroids followed by oral steroids accelerates visual recovery but provides no long-term benefit over oral steroids alone. Early treatment of multiple sclerosis after an initial demyelinating event such as optic neuritis can reduce future relapse rates and disability progression.