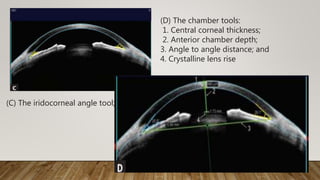
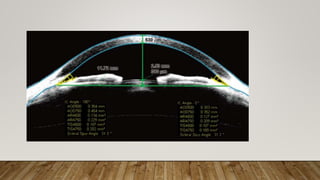
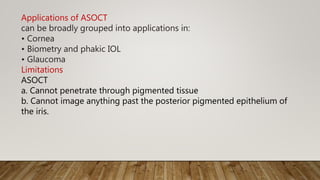
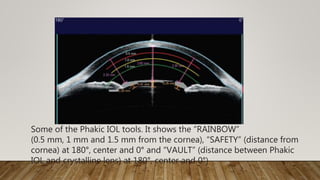
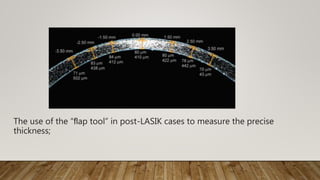
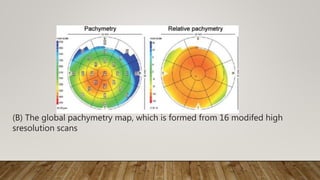
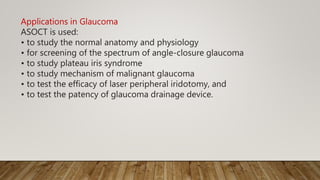
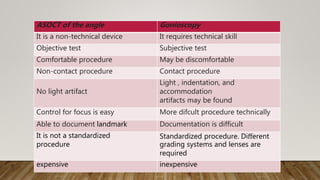
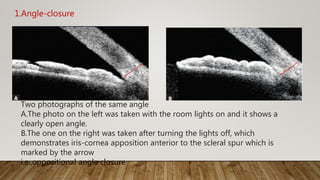
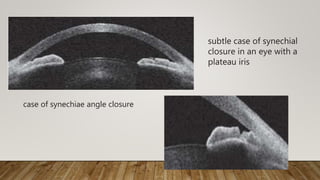
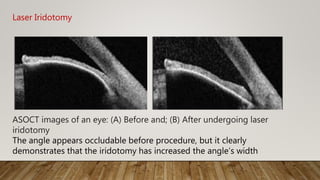
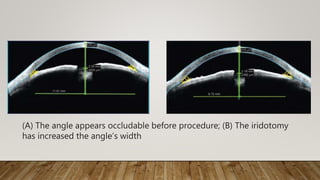
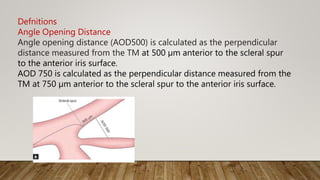
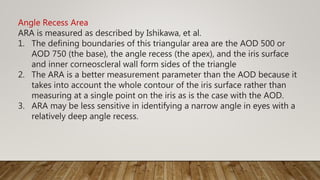
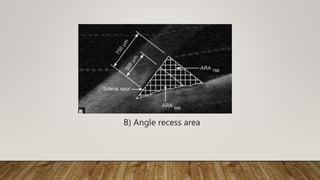
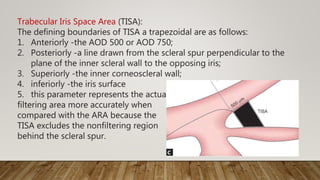
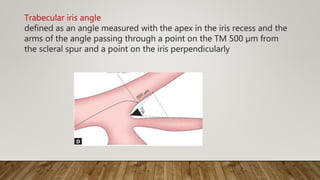
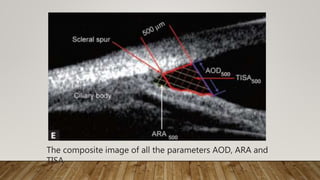
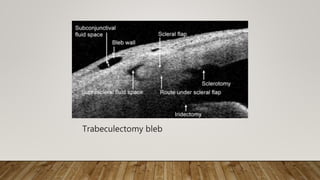
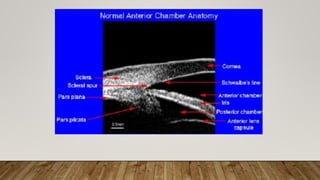
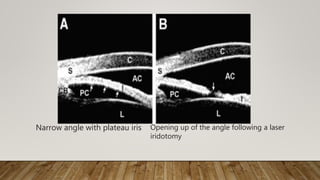
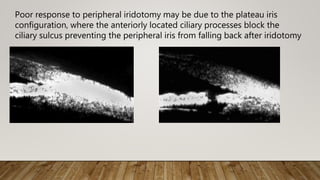
UBM and ASOCT provide high-resolution cross-sectional images of the anterior segment including the cornea, anterior chamber, angle, and iris. ASOCT uses optical coherence tomography with a wavelength of 1310nm for improved penetration and reduced retinal damage compared to posterior segment OCT. It allows high-speed imaging of dynamic structures. ASOCT has applications in assessing corneal diseases and procedures, glaucoma (including angle anatomy and iridotomy evaluation), and intraocular lens implantation. Measurements of angle width parameters help evaluate angle closure risk. While valuable for objective angle assessment, ASOCT cannot image all anatomical structures involved in glaucoma.