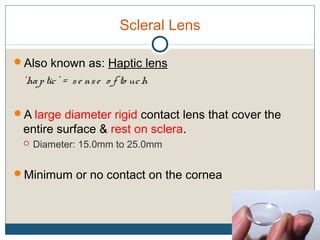
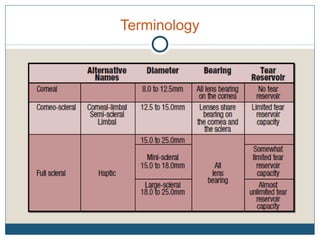
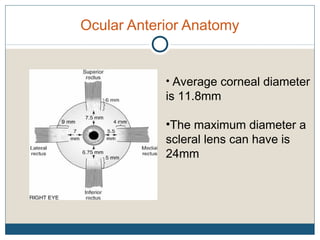
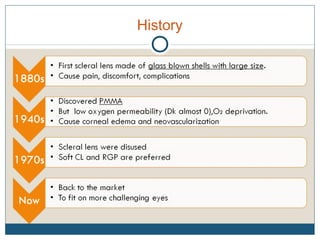
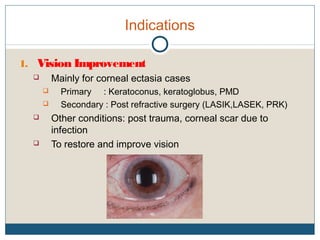
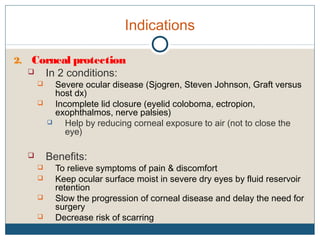
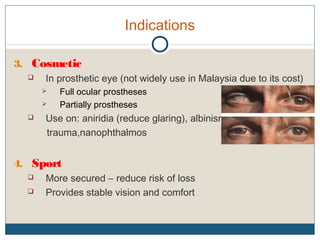
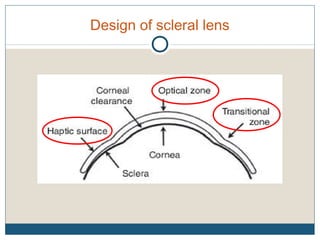
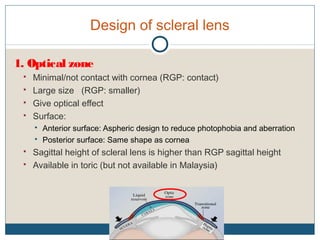
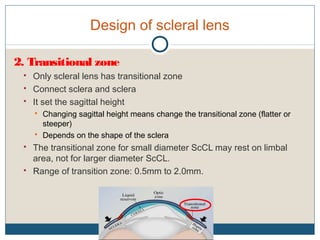
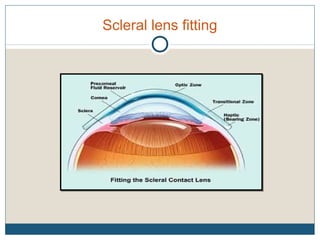
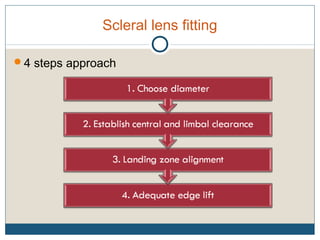
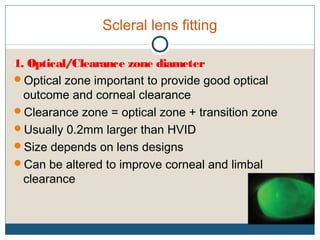
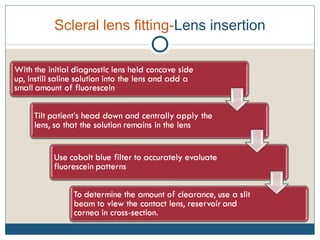
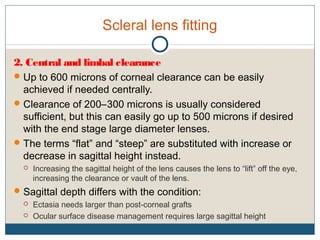
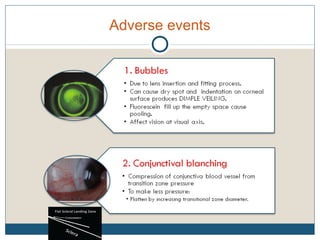
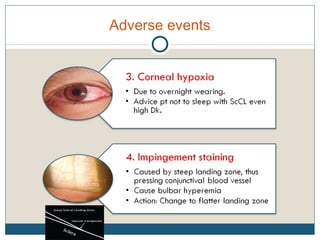
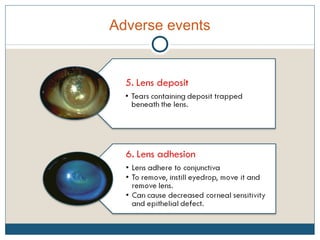
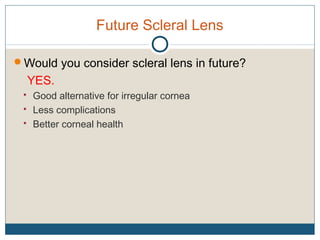
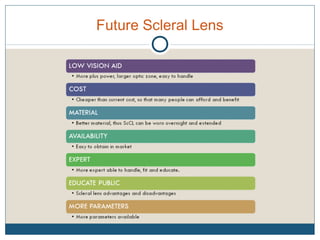
The document discusses scleral lenses, which are large diameter rigid contact lenses that rest on the sclera and are used primarily to improve vision in patients with corneal diseases. It covers the design, fitting processes, indications for use, adverse events, and patient compliance, highlighting their advantages and challenges. Scleral lenses are particularly noted for their ability to protect the cornea, provide cosmetic solutions, and deliver medication, although their high cost and fitting difficulties limit their popularity.