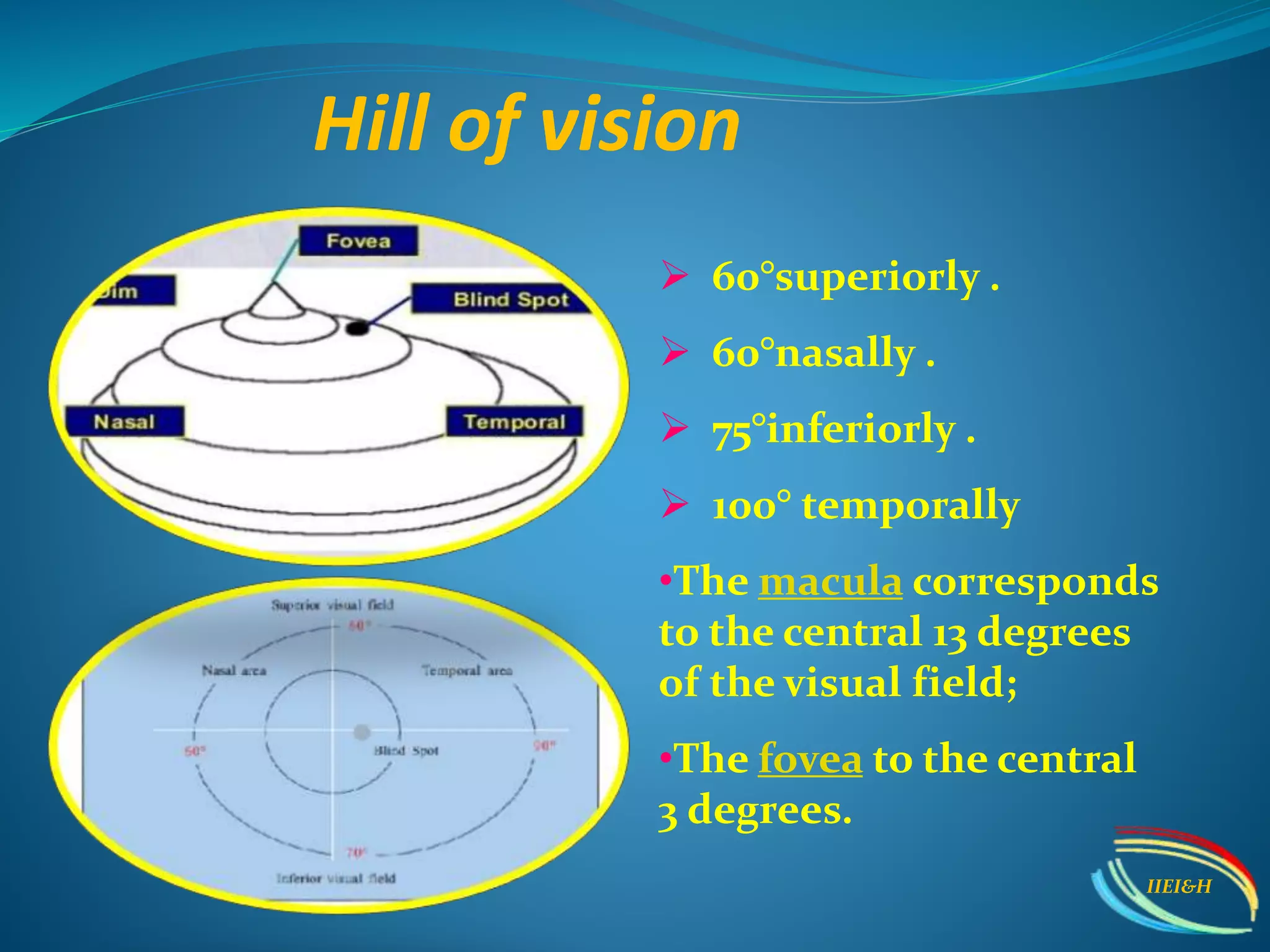
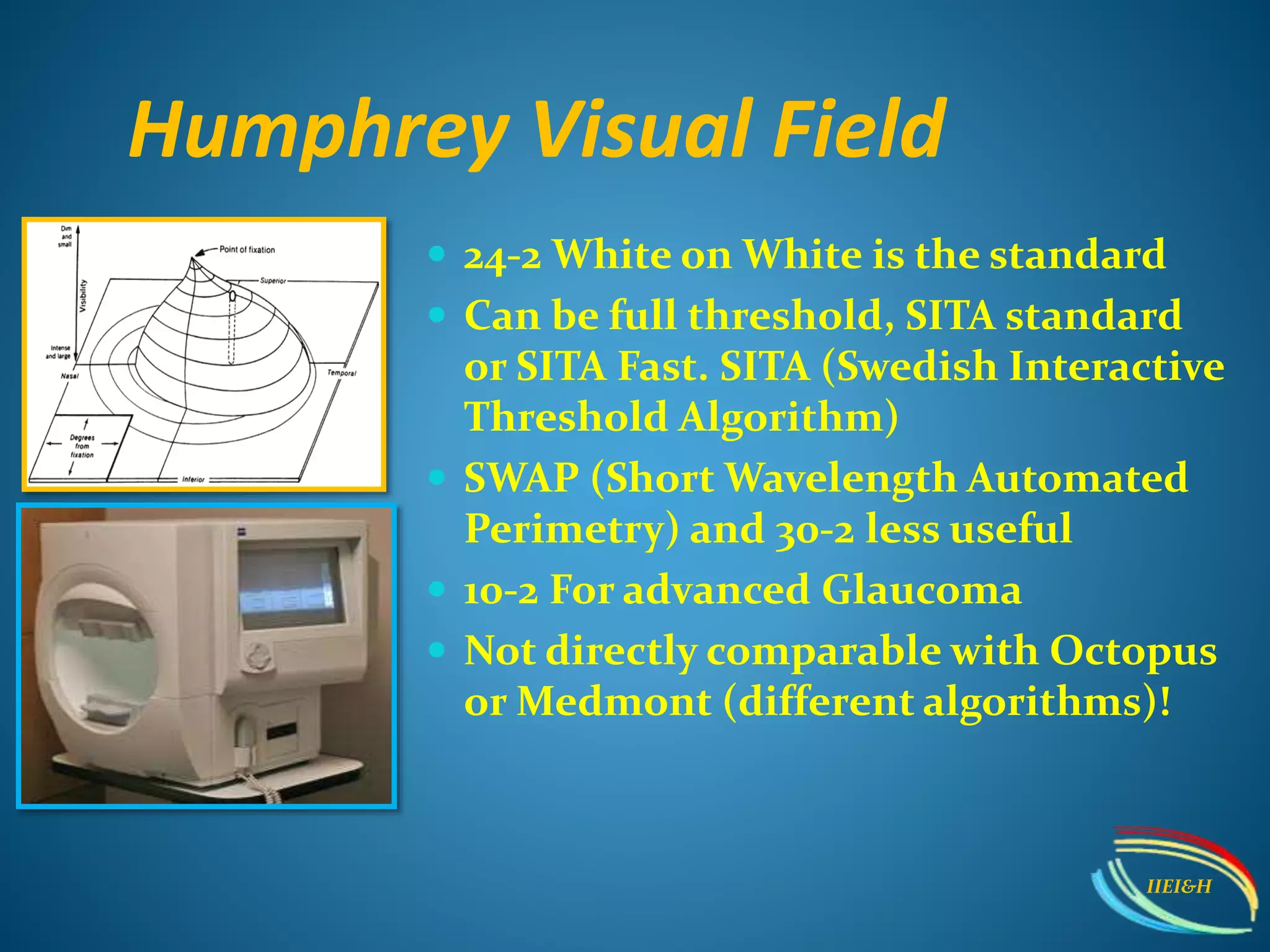
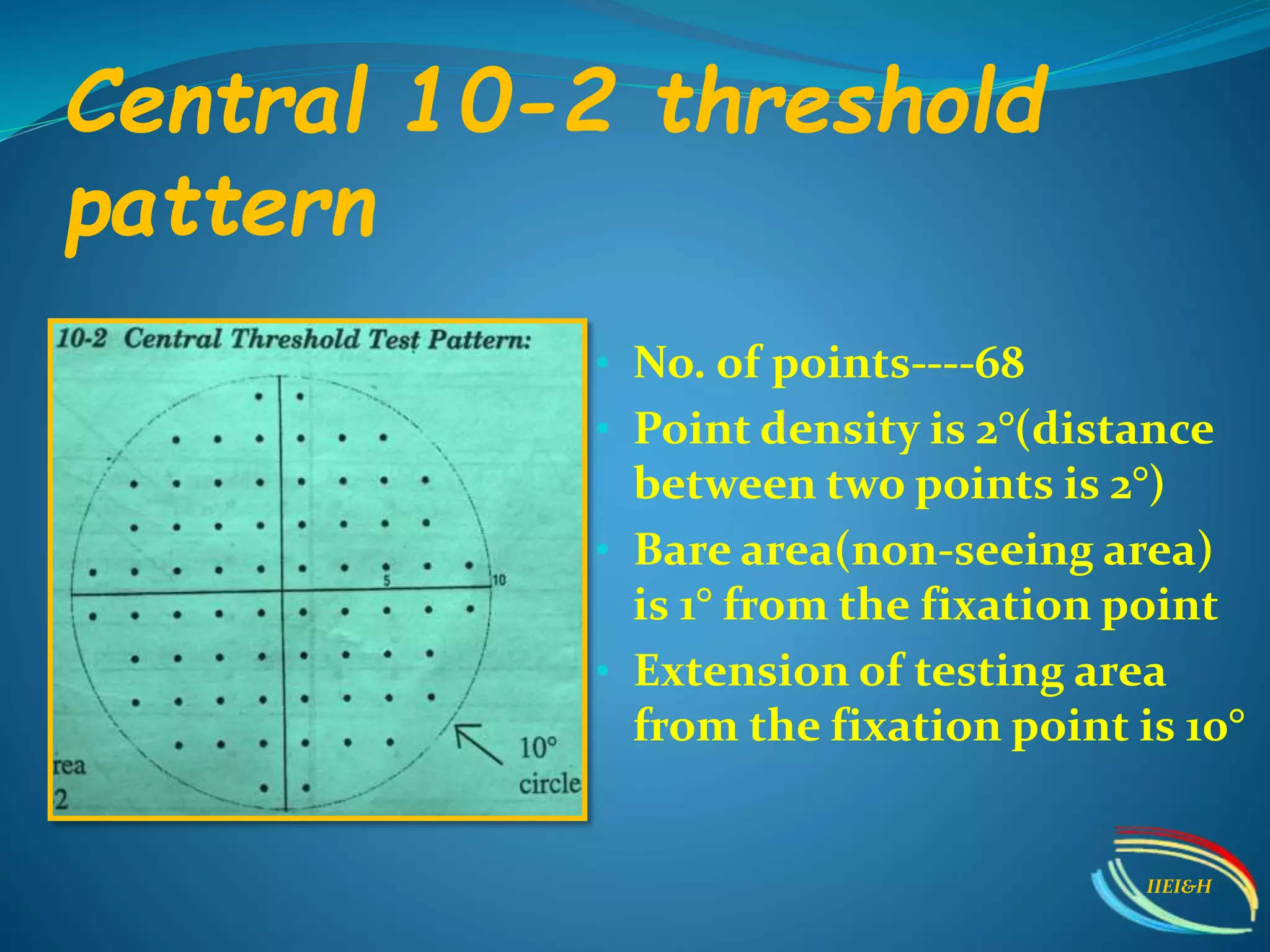
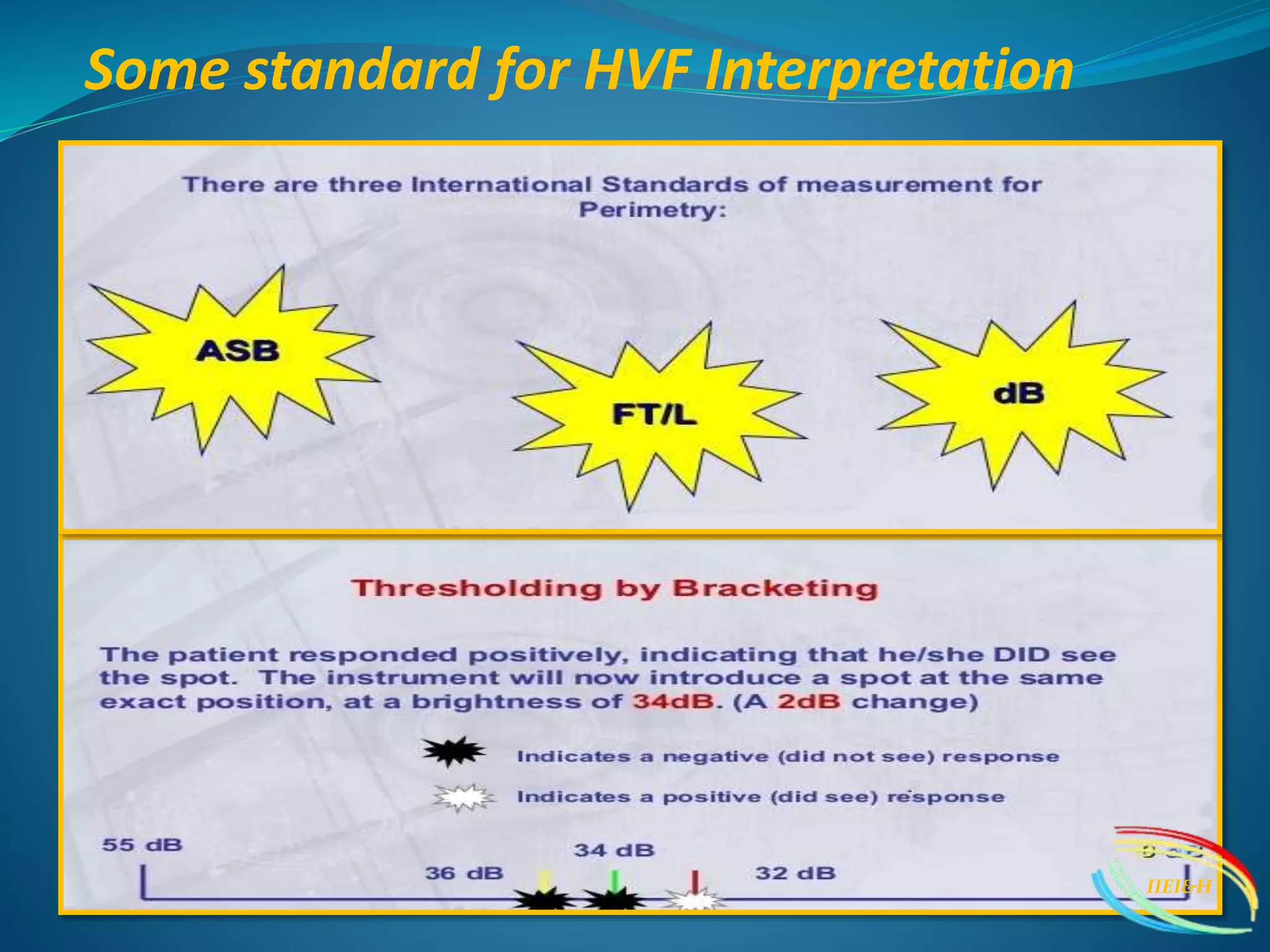
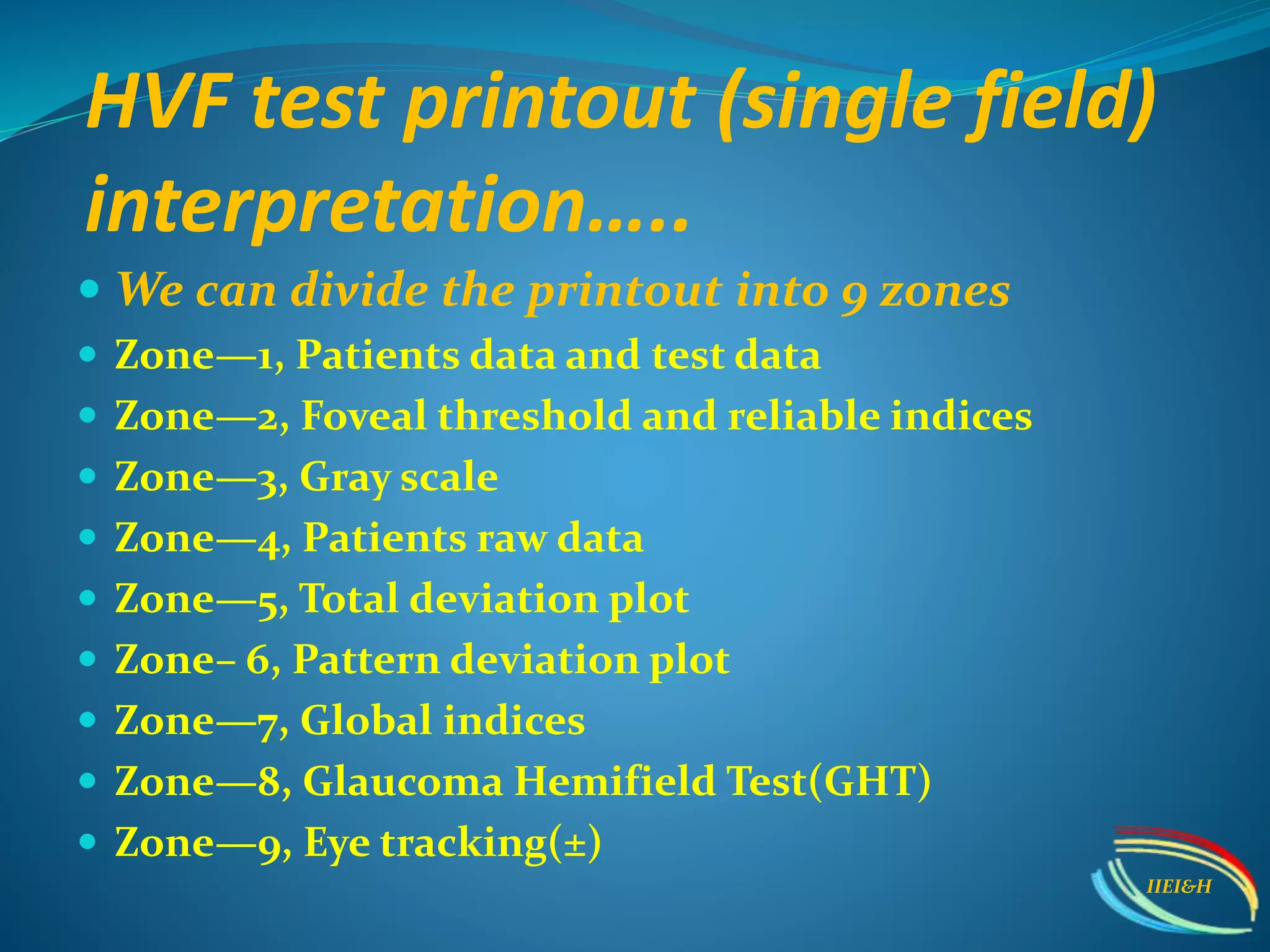
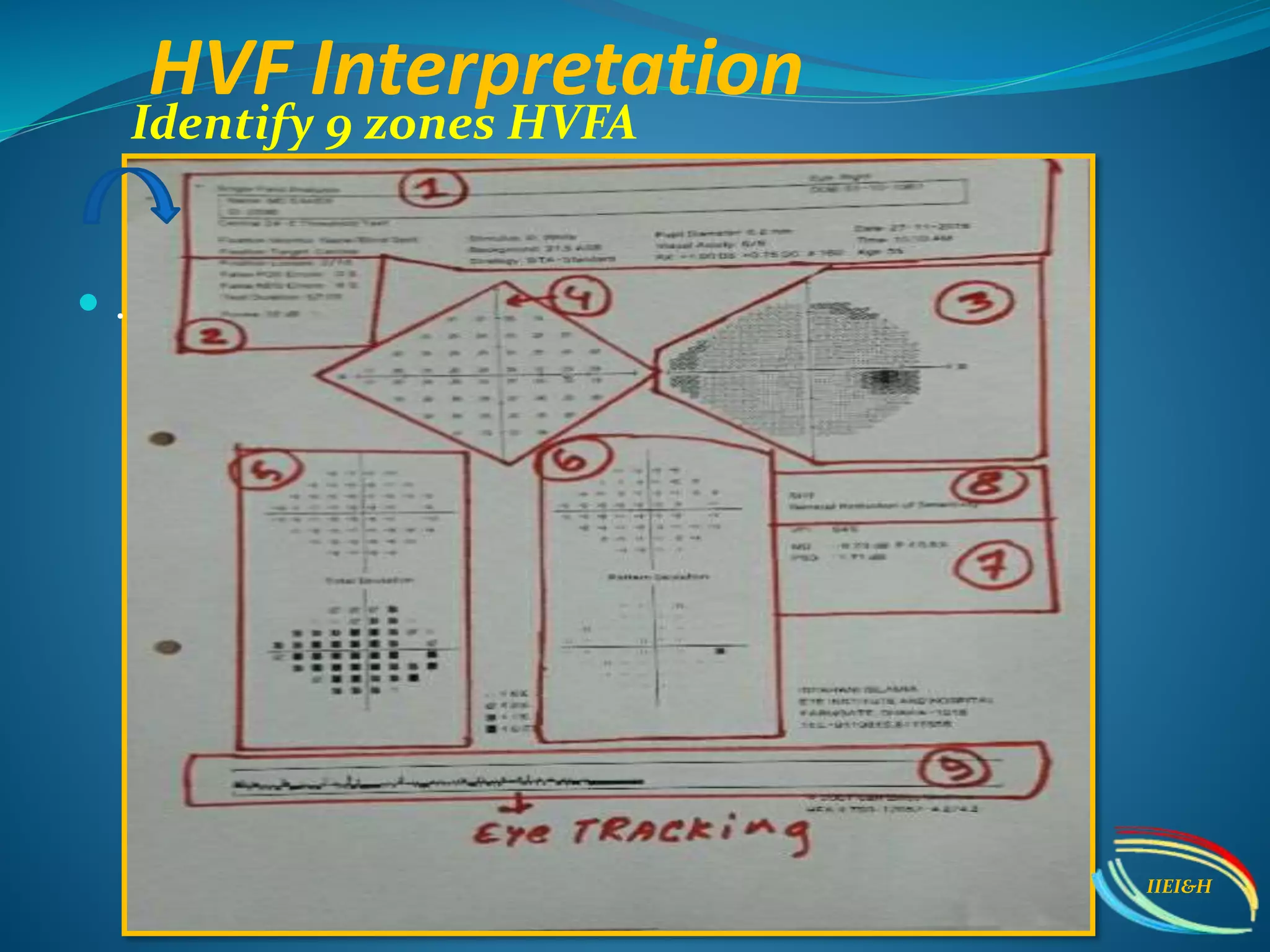
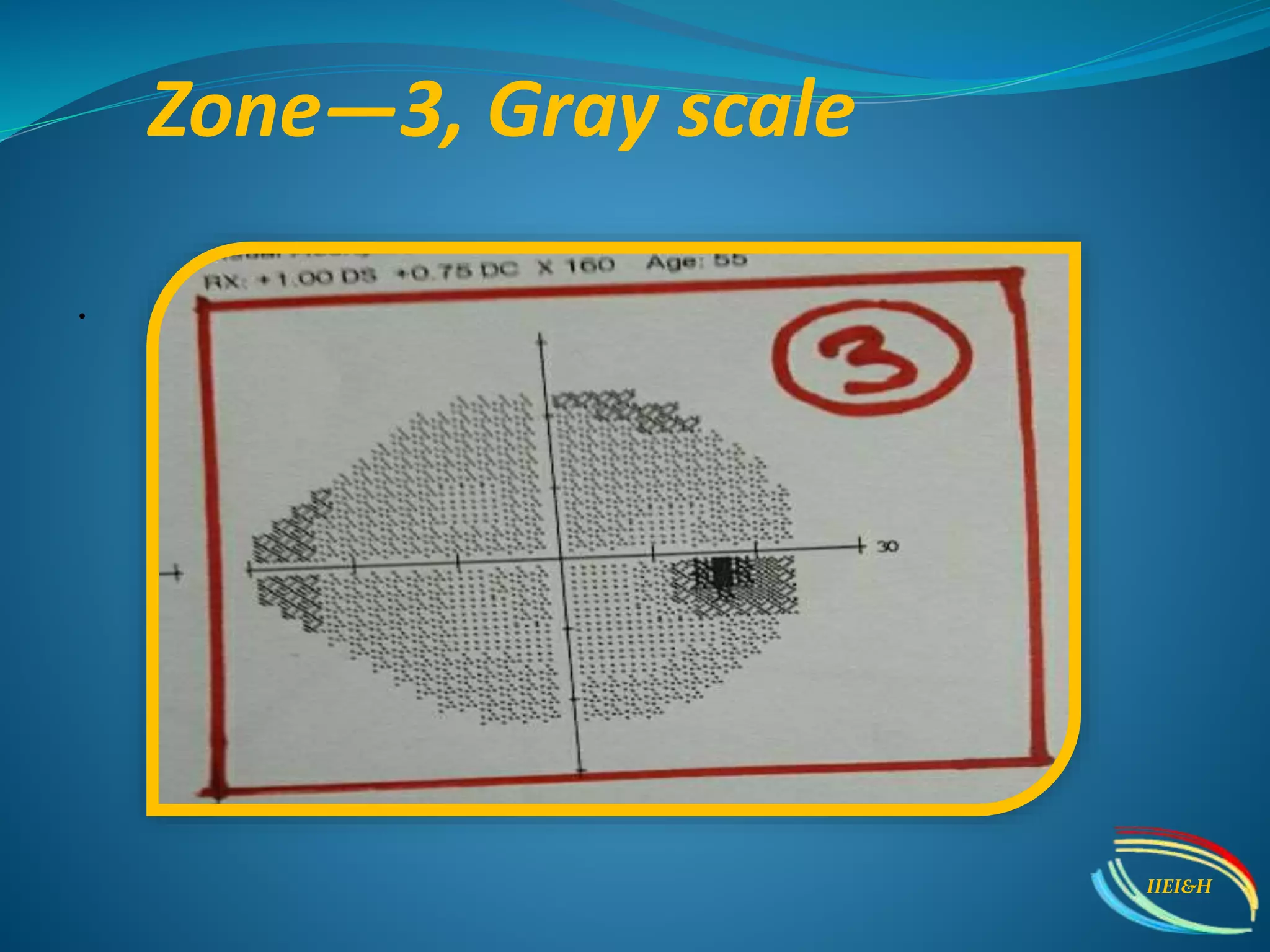
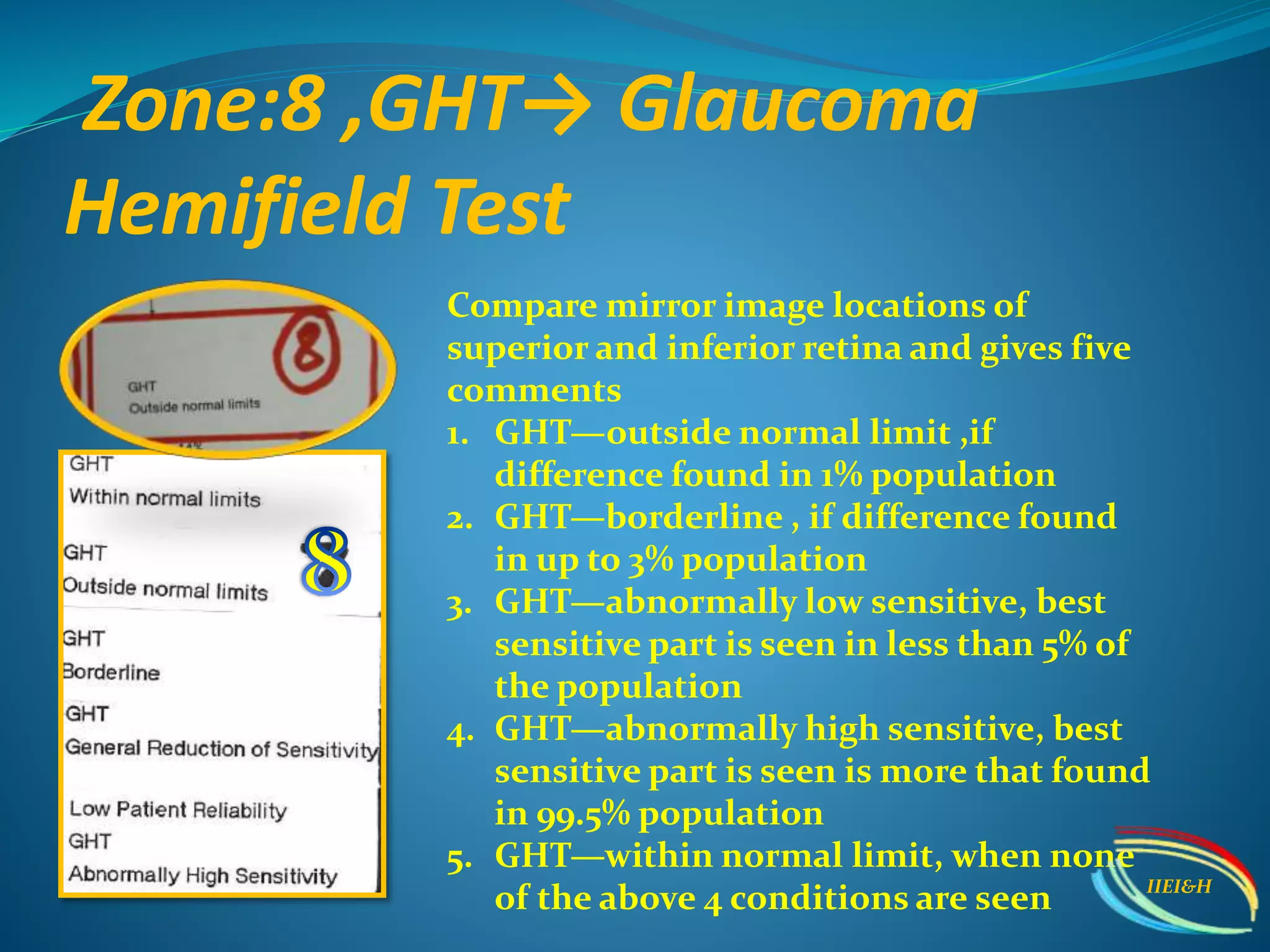
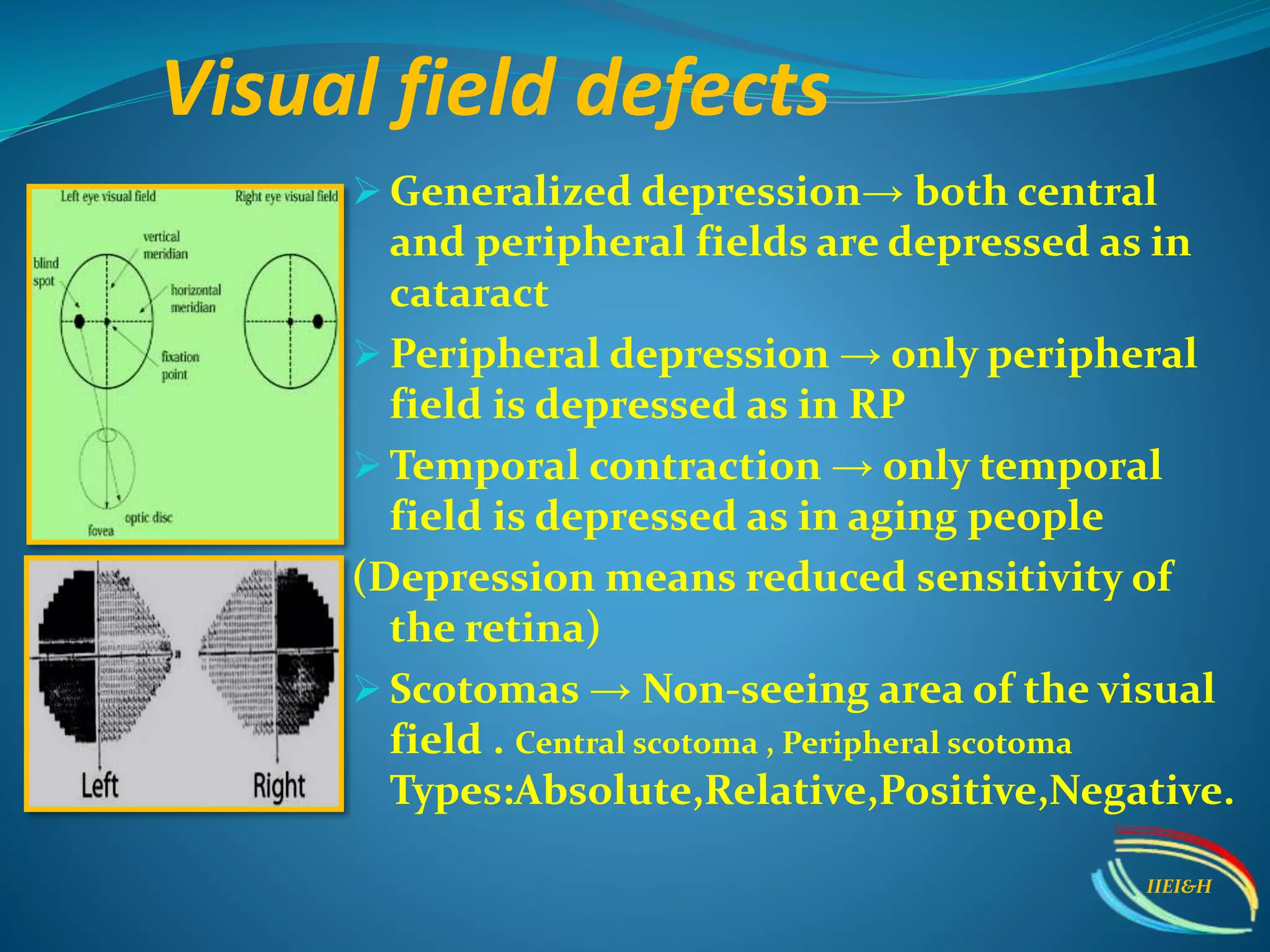
The document provides an overview of perimetry, focusing on the types, techniques, and interpretation of visual field tests used in identifying glaucoma and neurological lesions. It discusses kinetic and static perimetry, detailing the standards and methods such as Humphrey Visual Field tests, including classifications and interpretation of results. Additionally, it highlights common errors in testing and emphasizes that not all visual field defects indicate glaucoma, stressing the importance of monitoring progression over time.