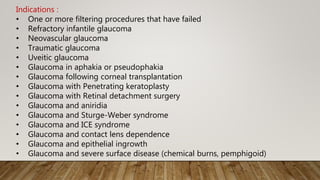
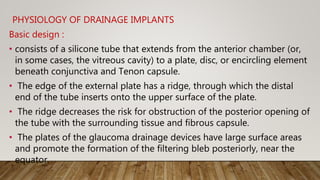
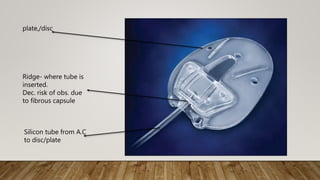
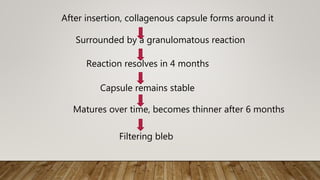
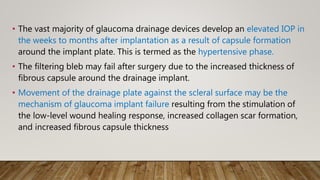
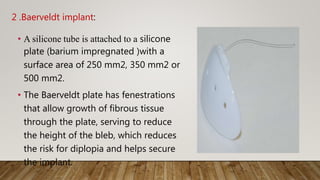
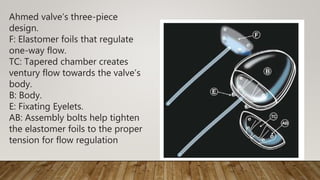
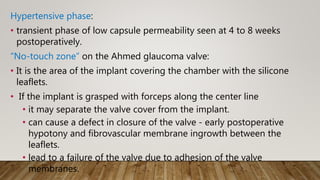
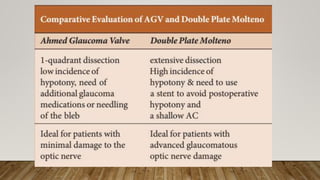
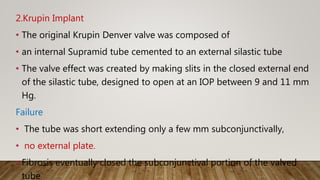
Glaucoma drainage devices (GDDs) work by creating an alternate pathway for aqueous outflow from the anterior chamber through a silicone tube to a plate under the conjunctiva where fluid is absorbed. The Ahmed valve and Baerveldt implant are two commonly used valved and non-valved devices, respectively. The Ahmed valve uses silicone leaflets to allow one-way flow above a certain pressure threshold, while the Baerveldt implant relies on a fibrous capsule formation around its plate for resistance to outflow. GDDs are indicated for refractory glaucoma when other surgeries have failed.