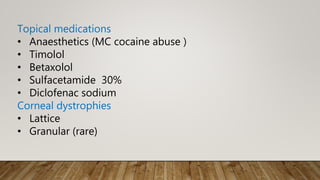
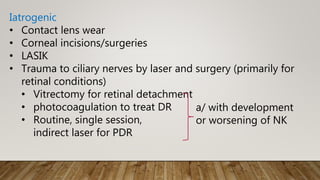
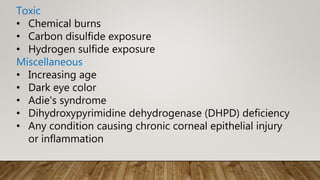
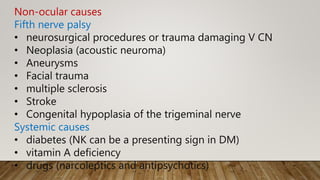
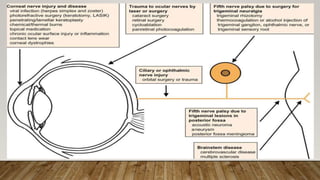
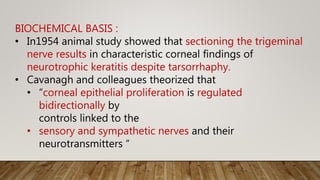
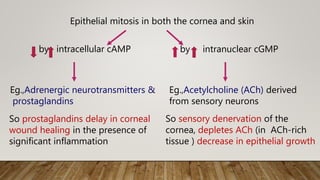
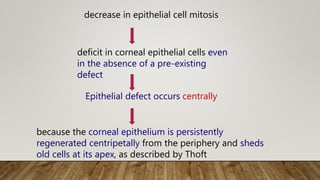
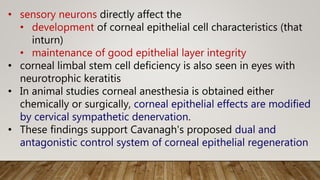
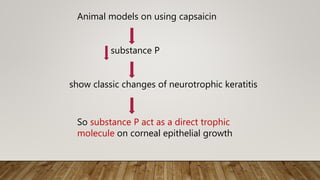
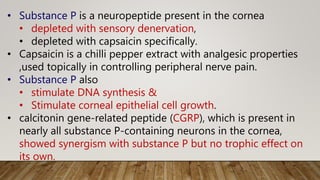
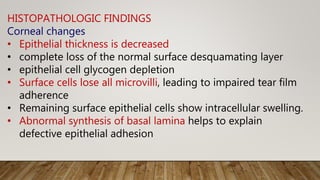
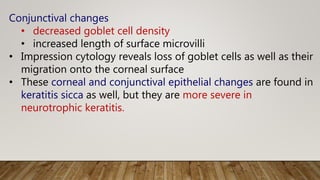
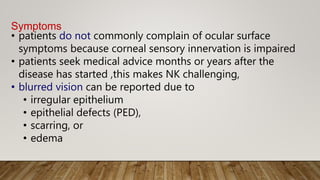
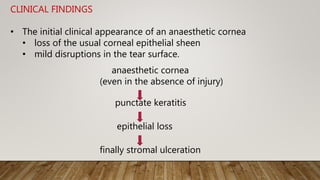
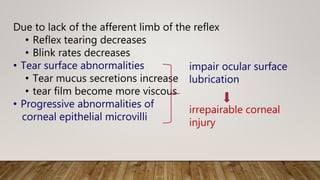
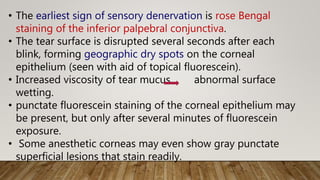
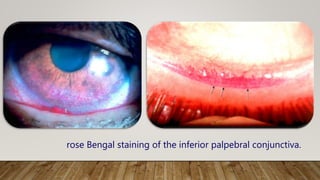
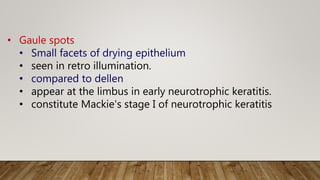
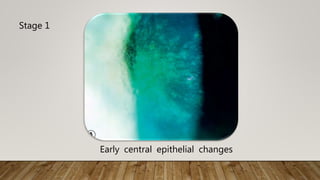
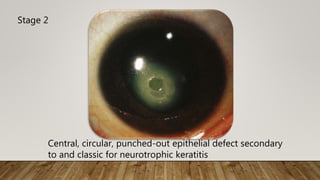
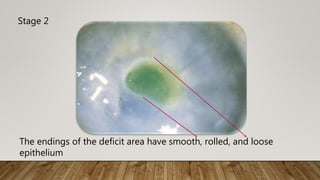
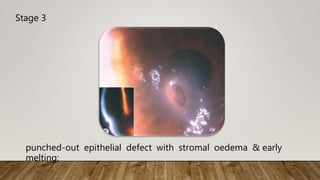
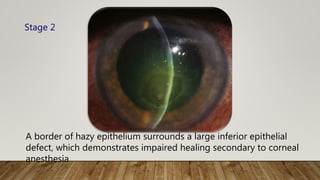
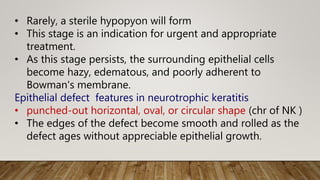
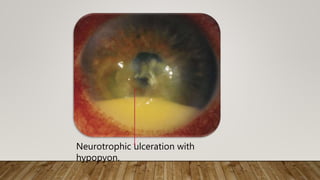
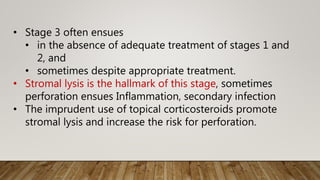
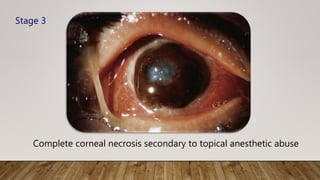
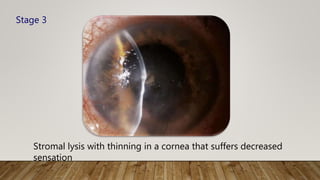
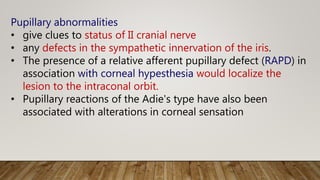
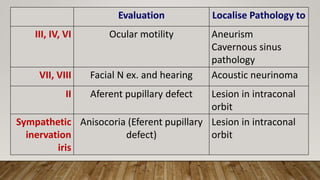
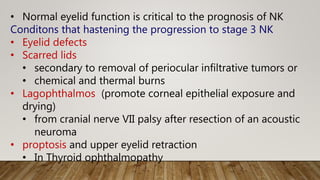
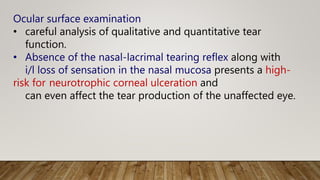
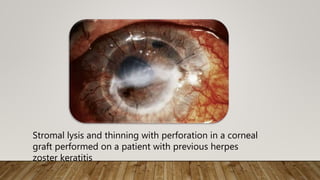
This document summarizes neurotrophic keratitis, a degenerative disease of the cornea characterized by impaired healing due to loss of corneal sensation. It discusses the causes including infections, medications, trauma and systemic diseases. Three stages of the condition are described from early punctate keratitis and epithelial defects to stromal ulceration and potential perforation. The role of sensory innervation in maintaining the corneal epithelium is explained through animal studies. Diagnosis involves rose Bengal staining and fluorescein evaluation, while treatment aims to promote re-epithelialization in early stages to prevent progression to stromal melting and perforation.