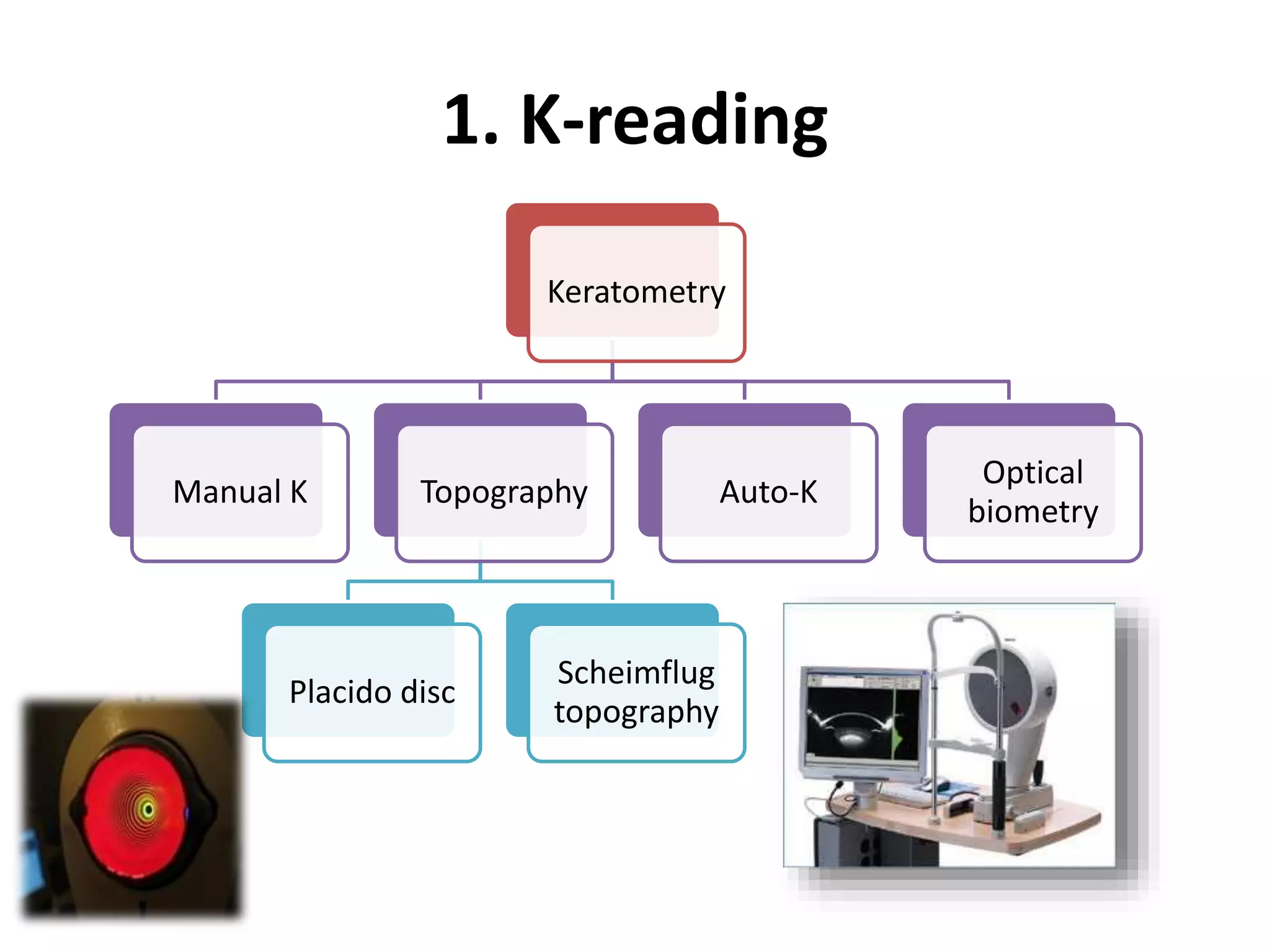
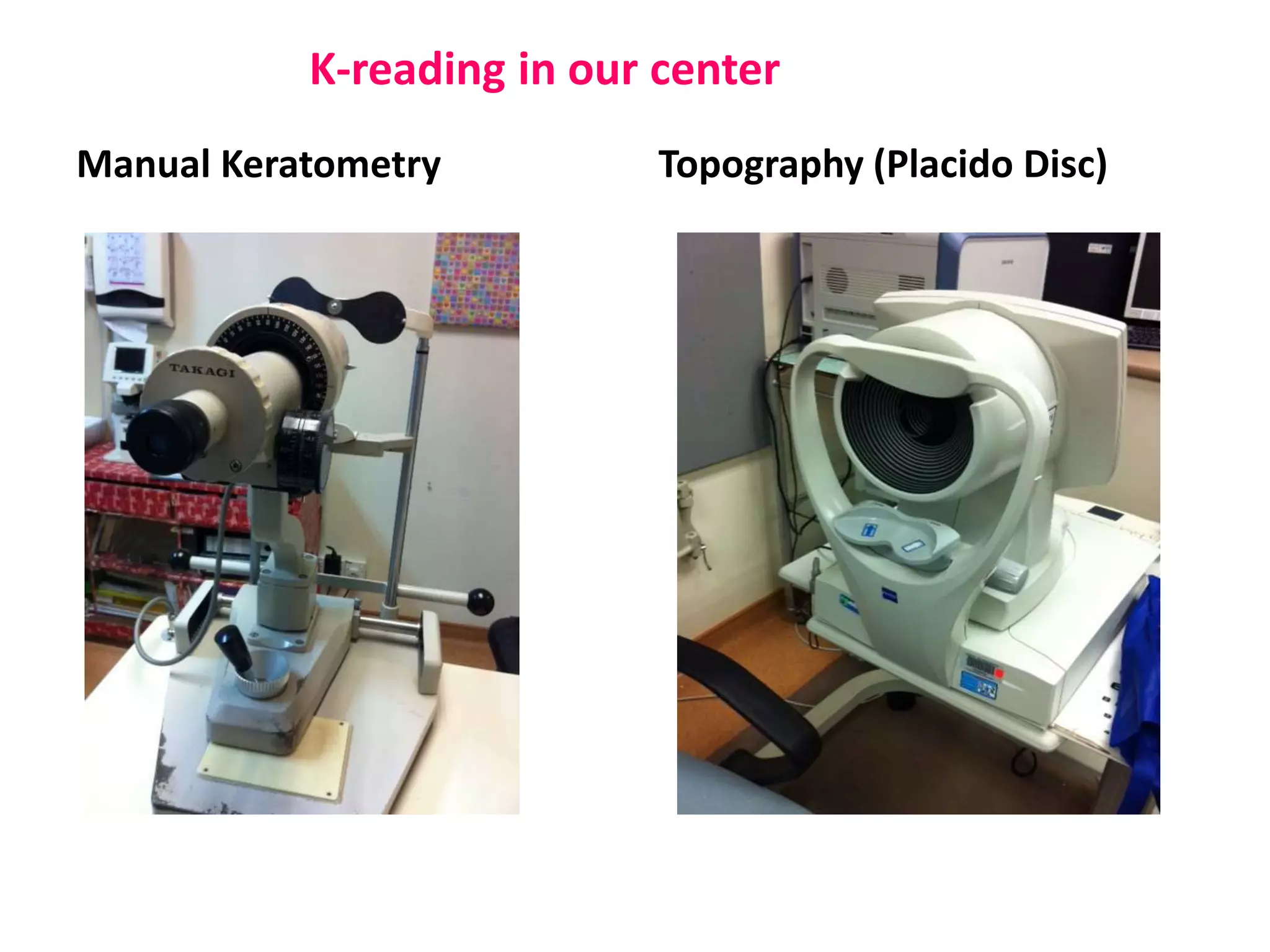
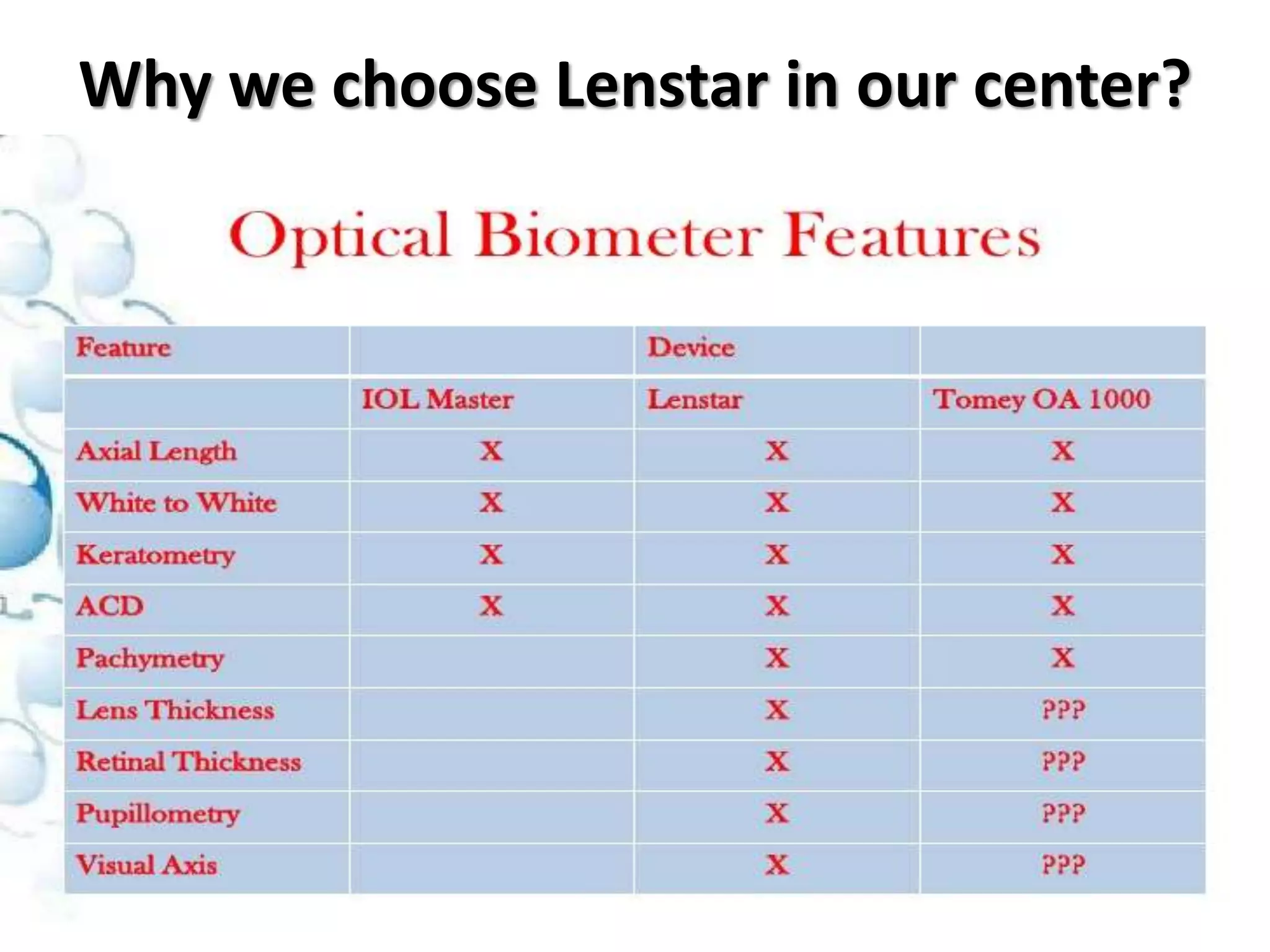
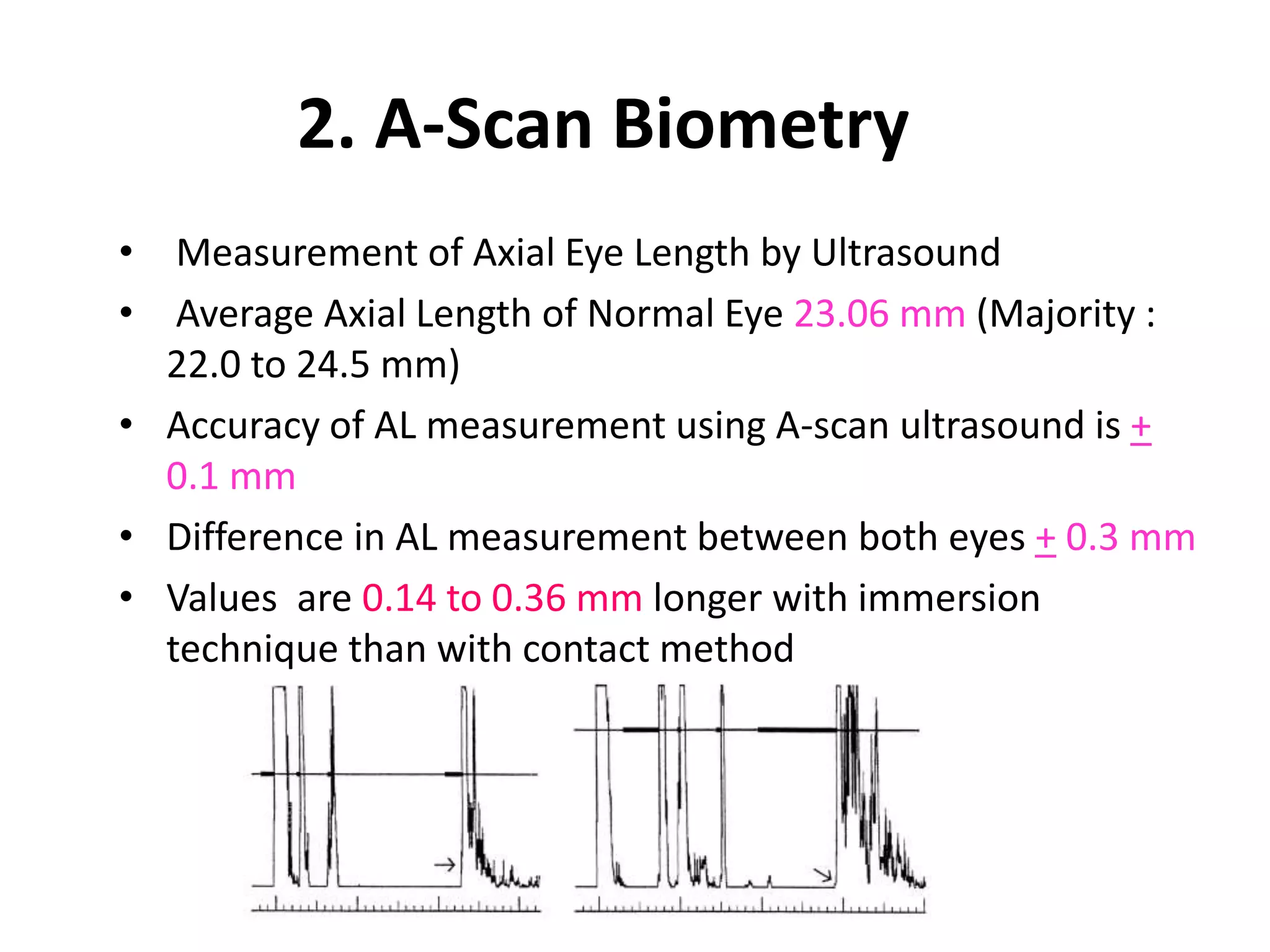
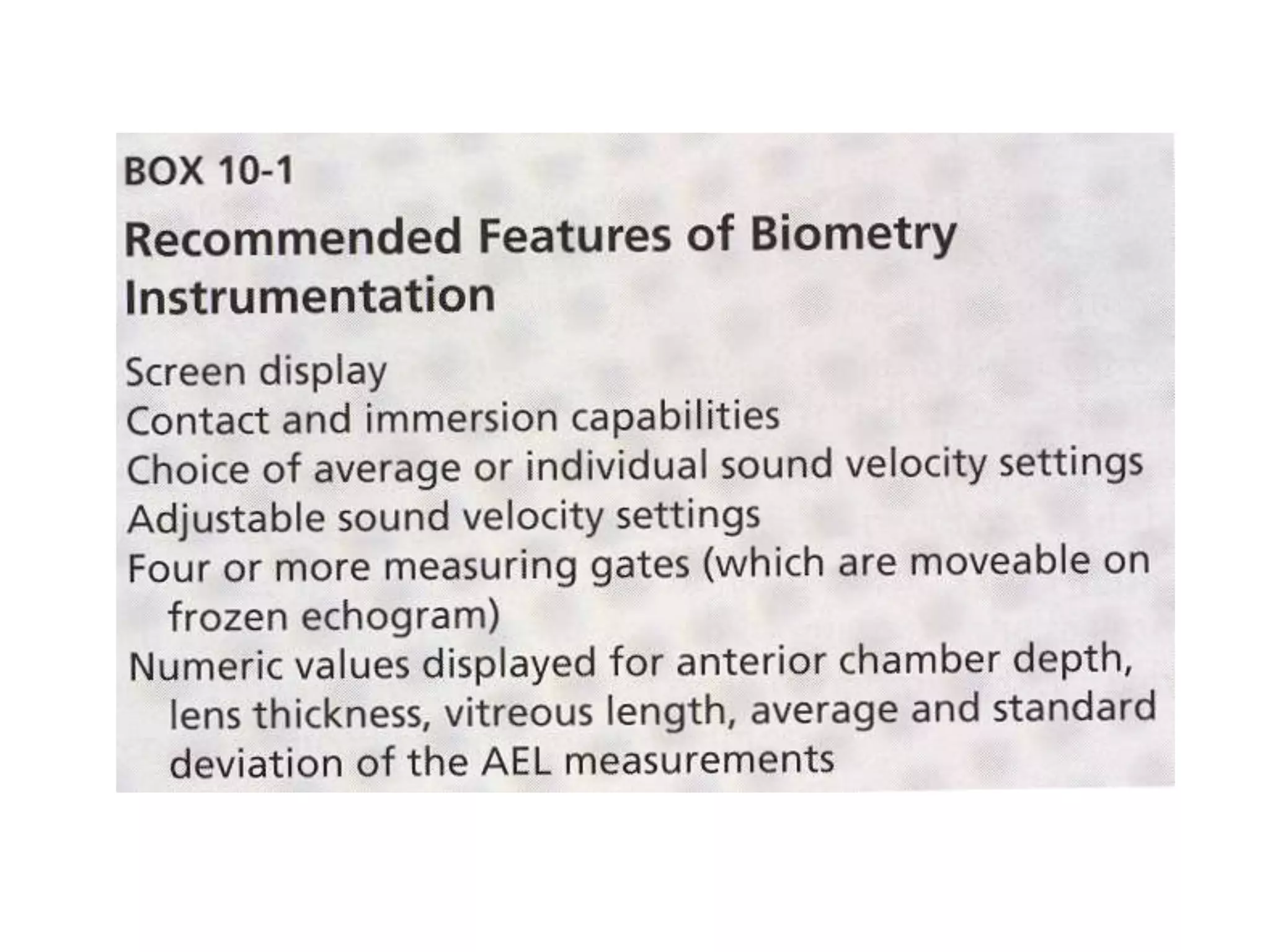
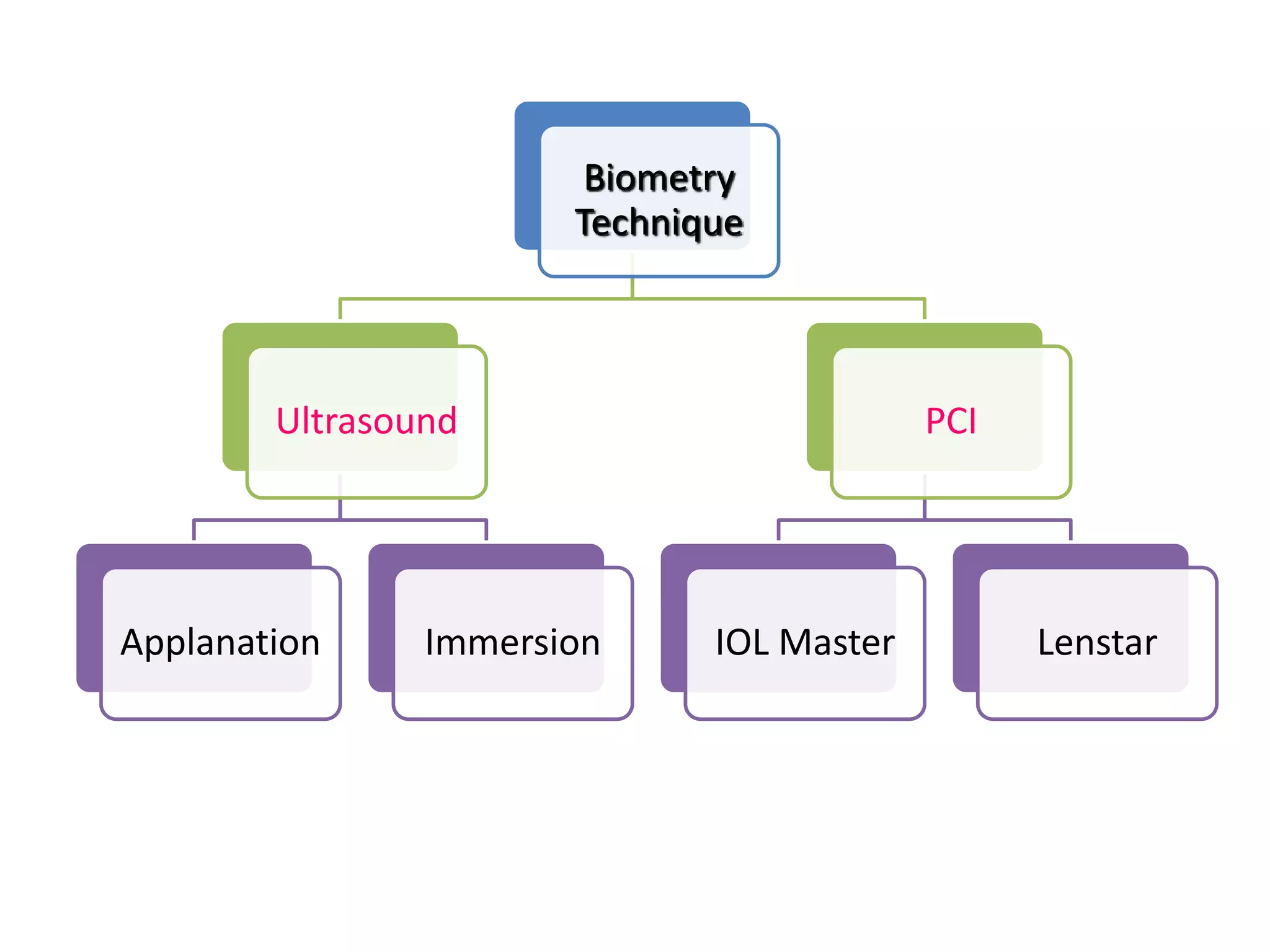
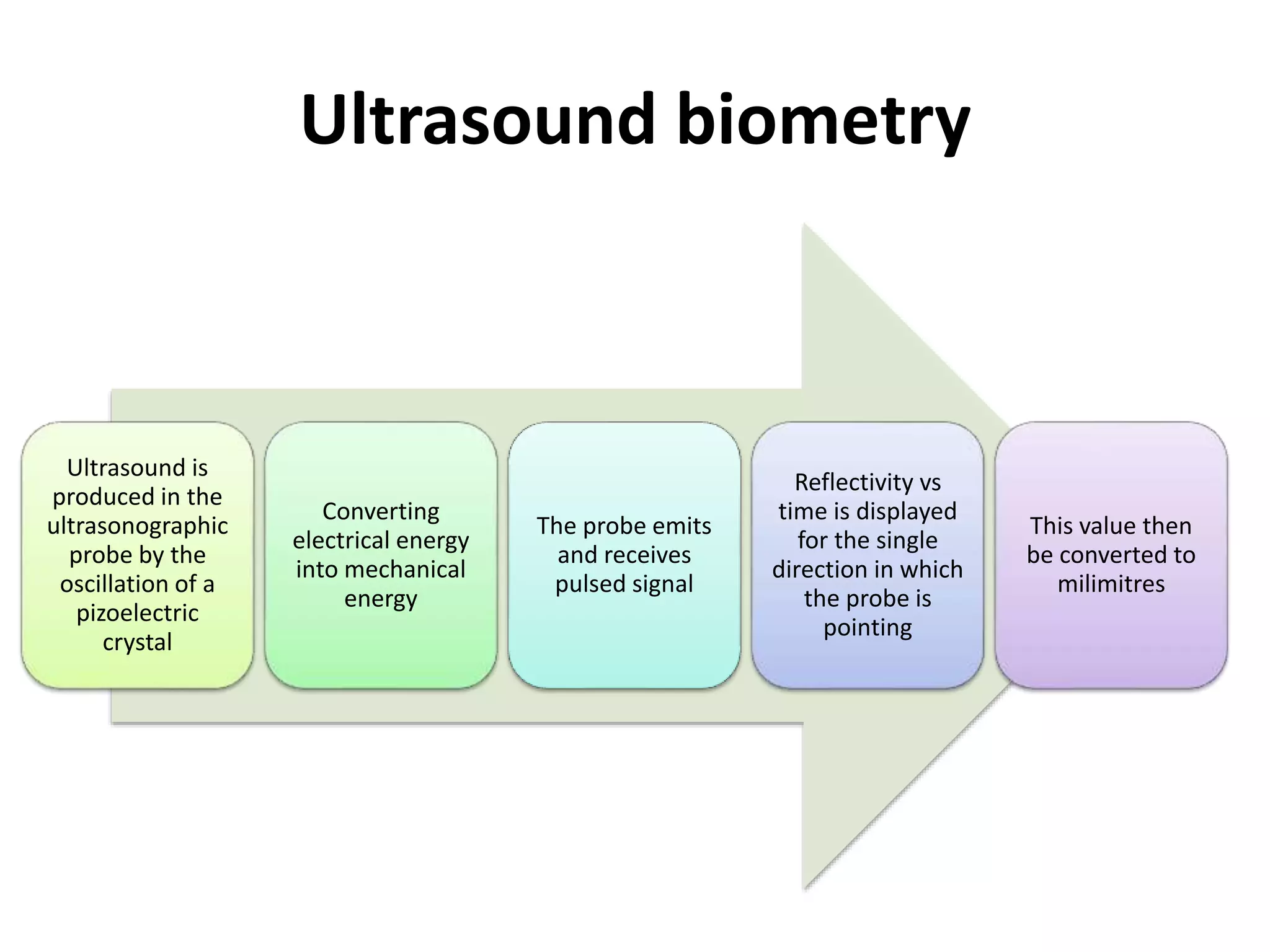
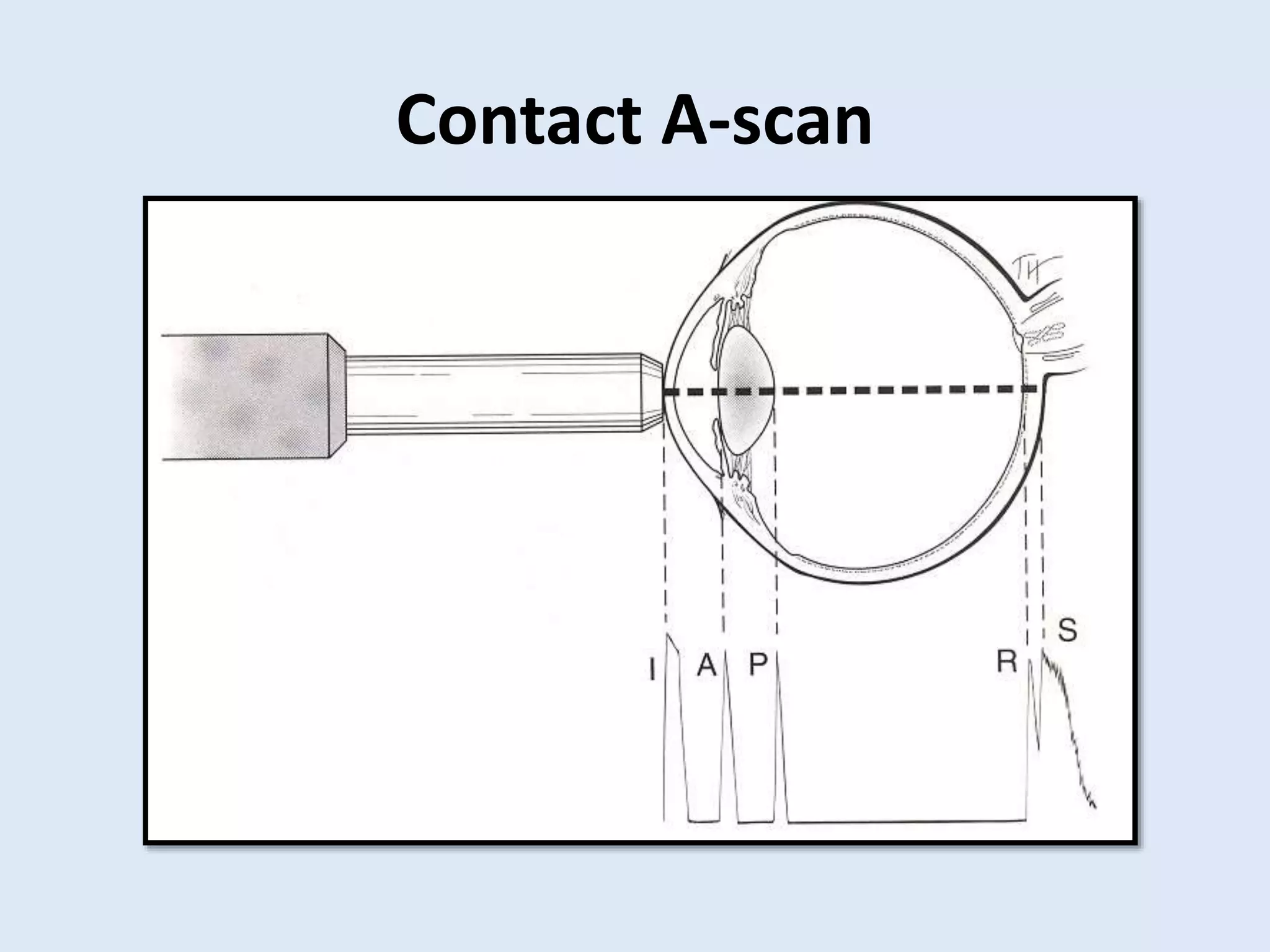
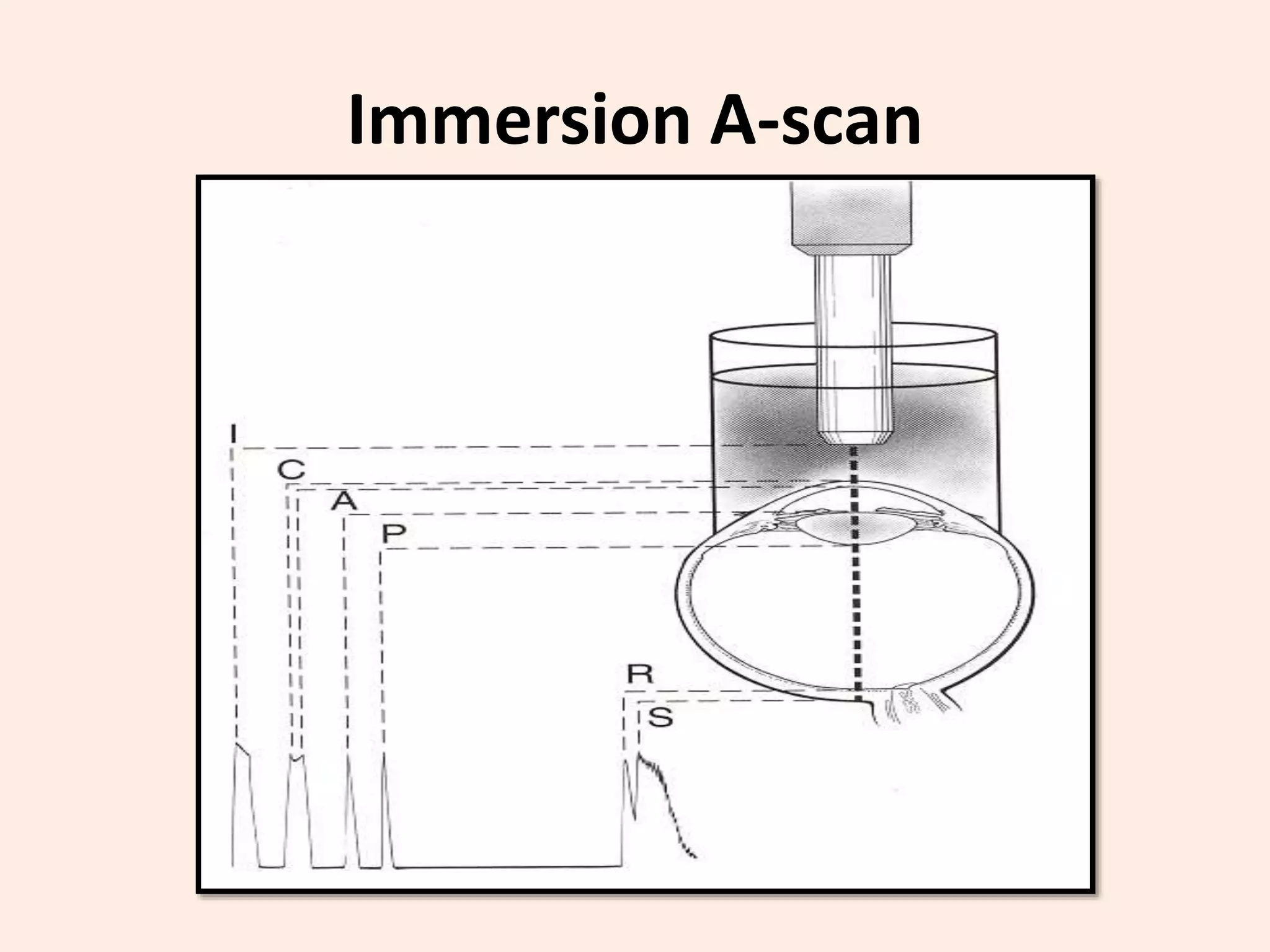
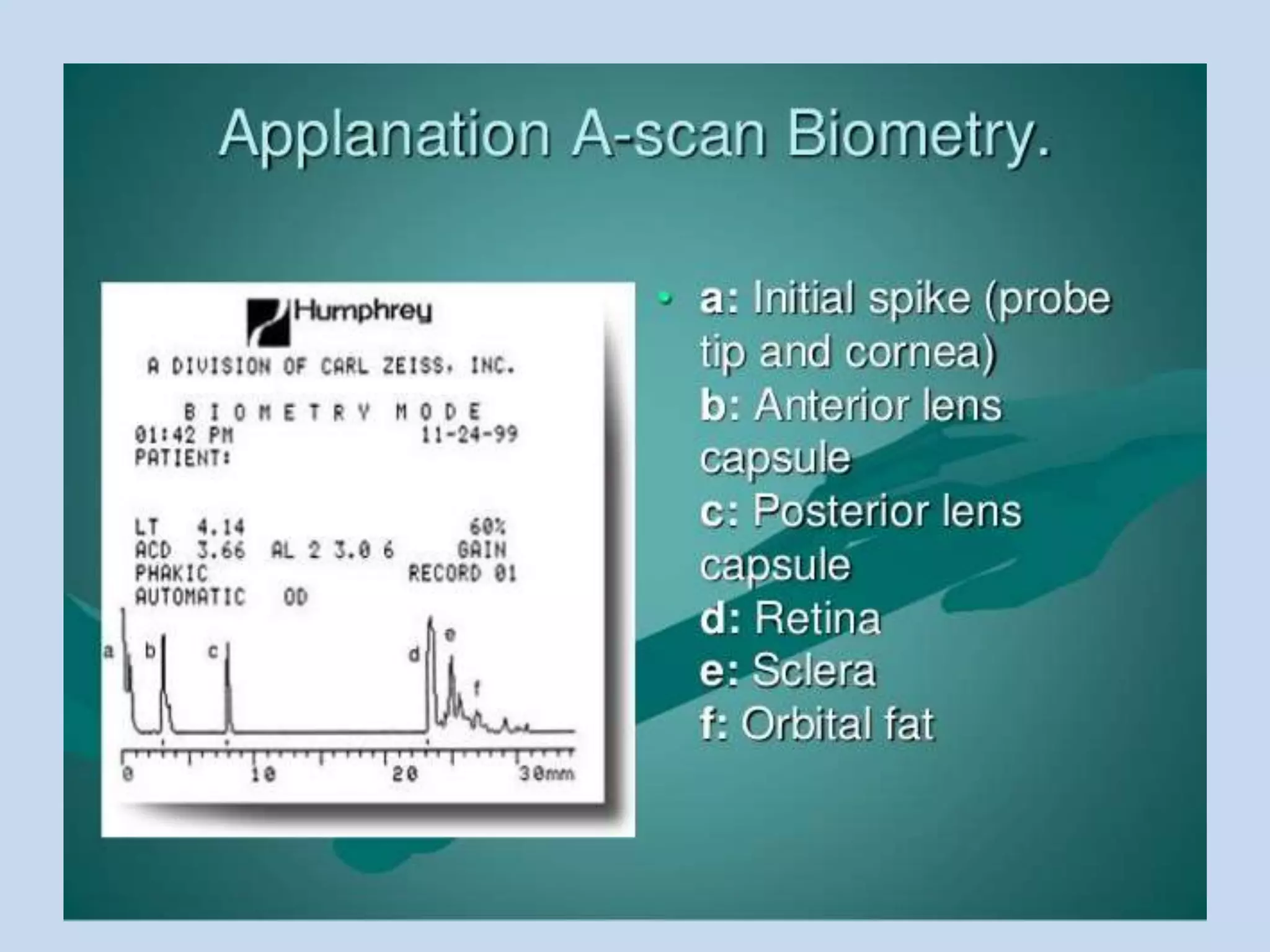
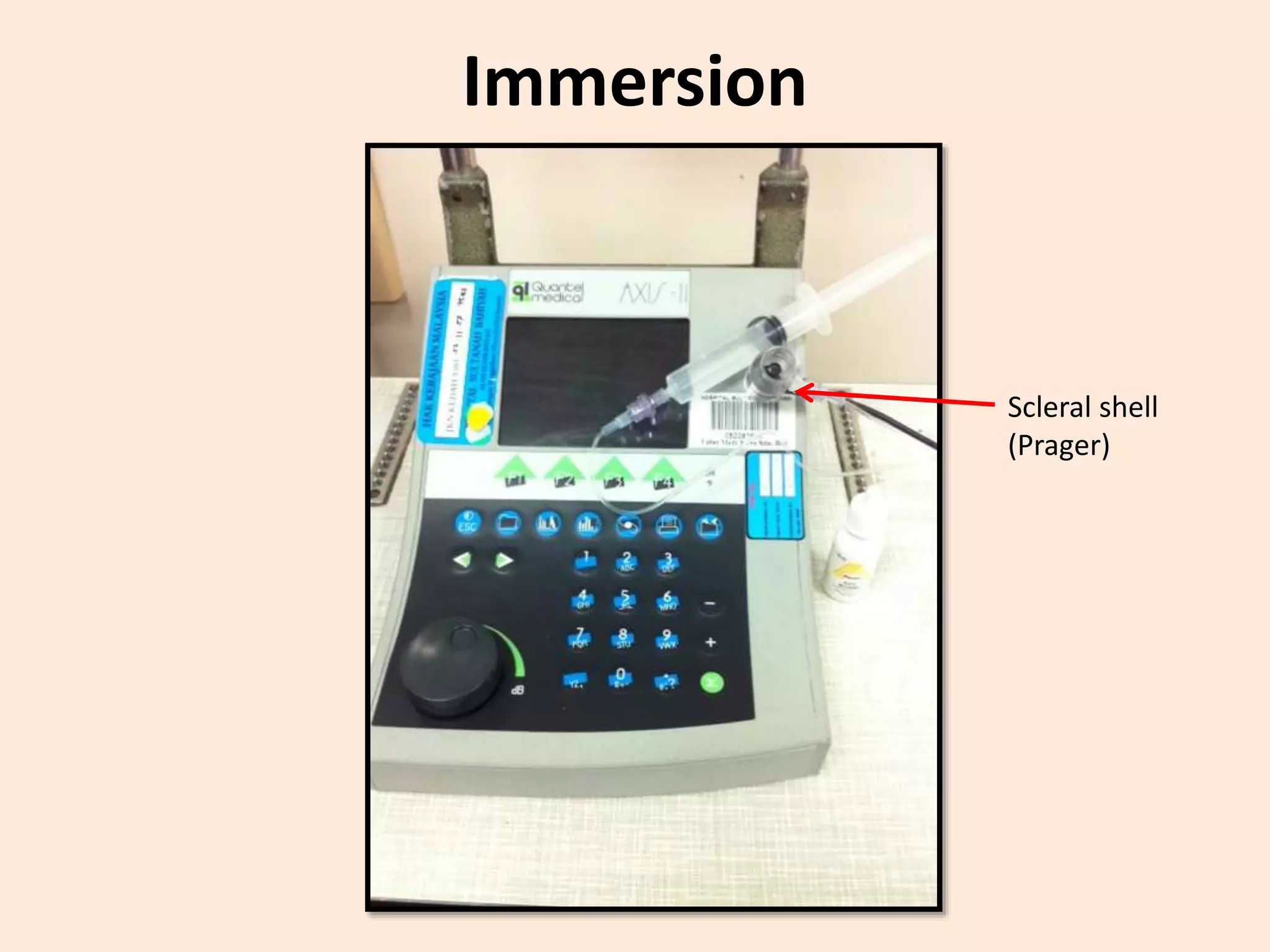
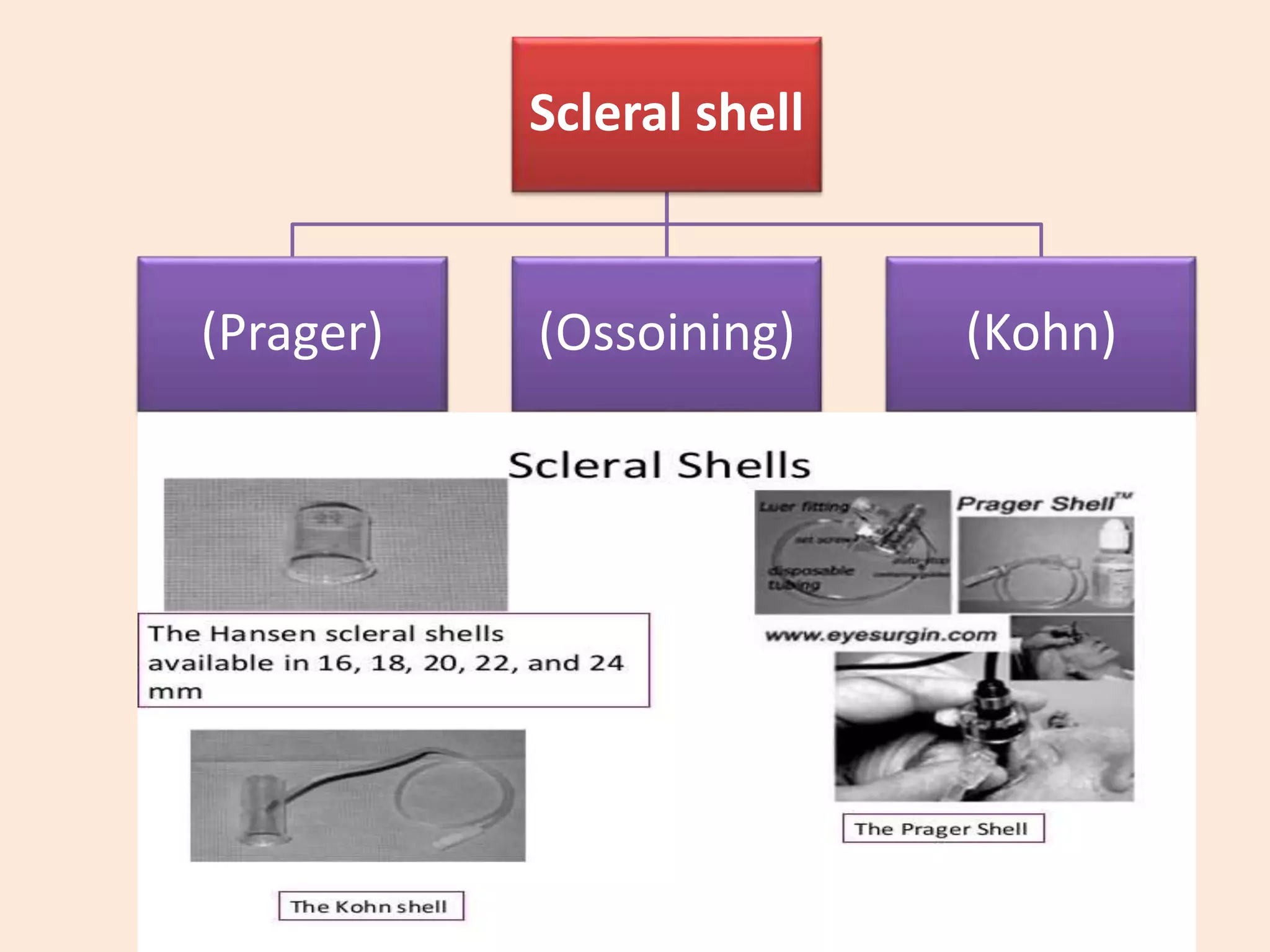
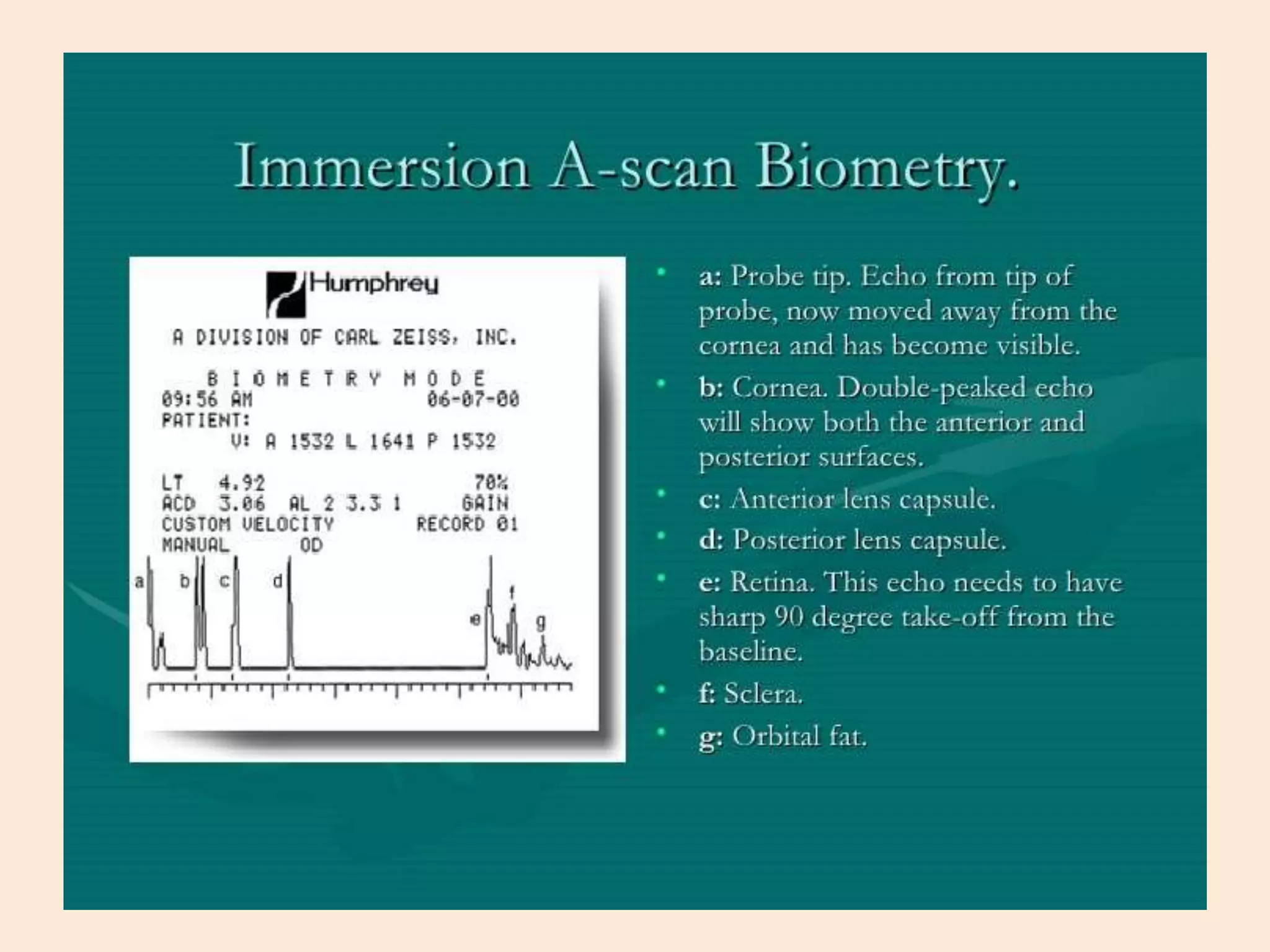
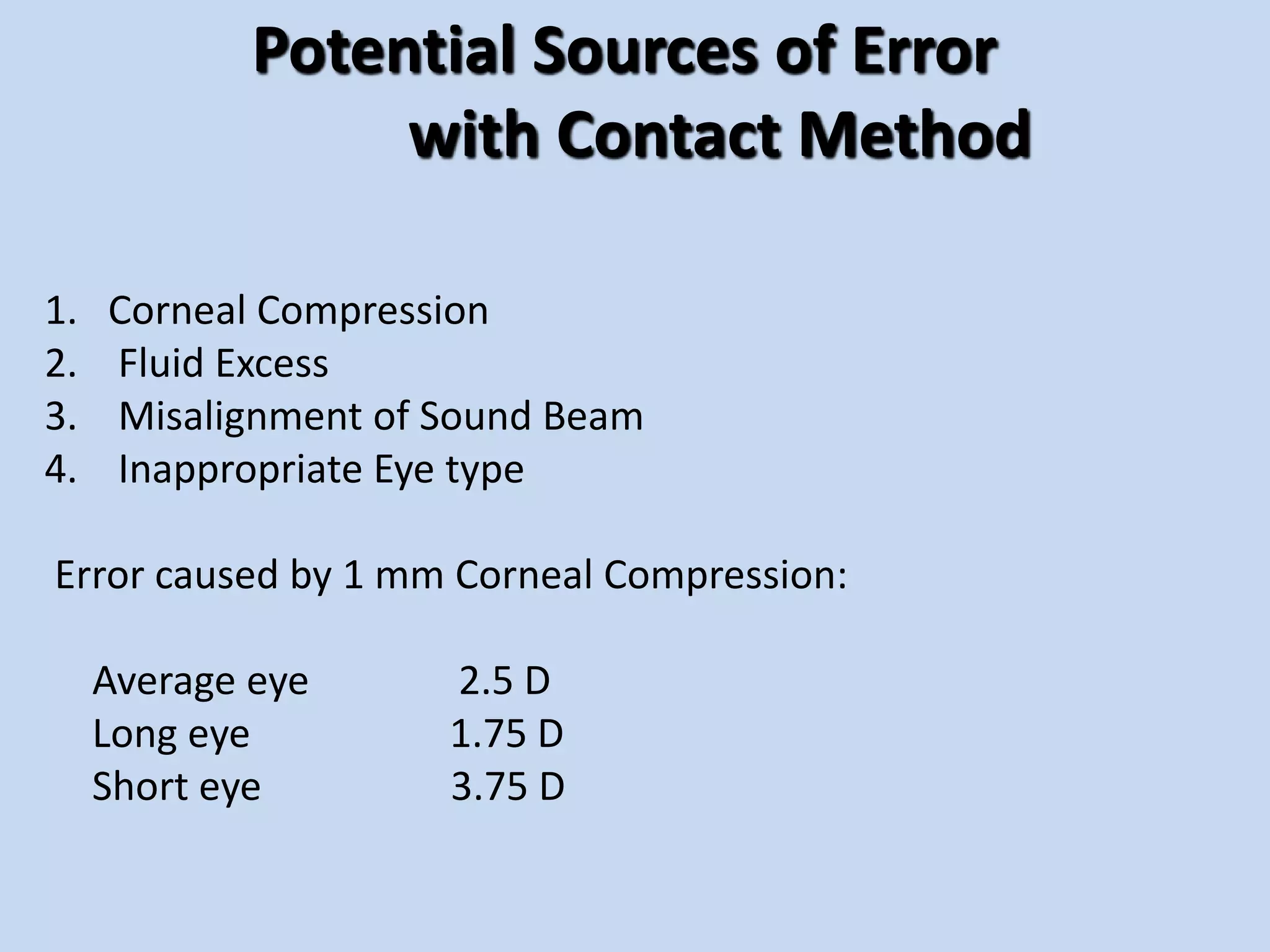
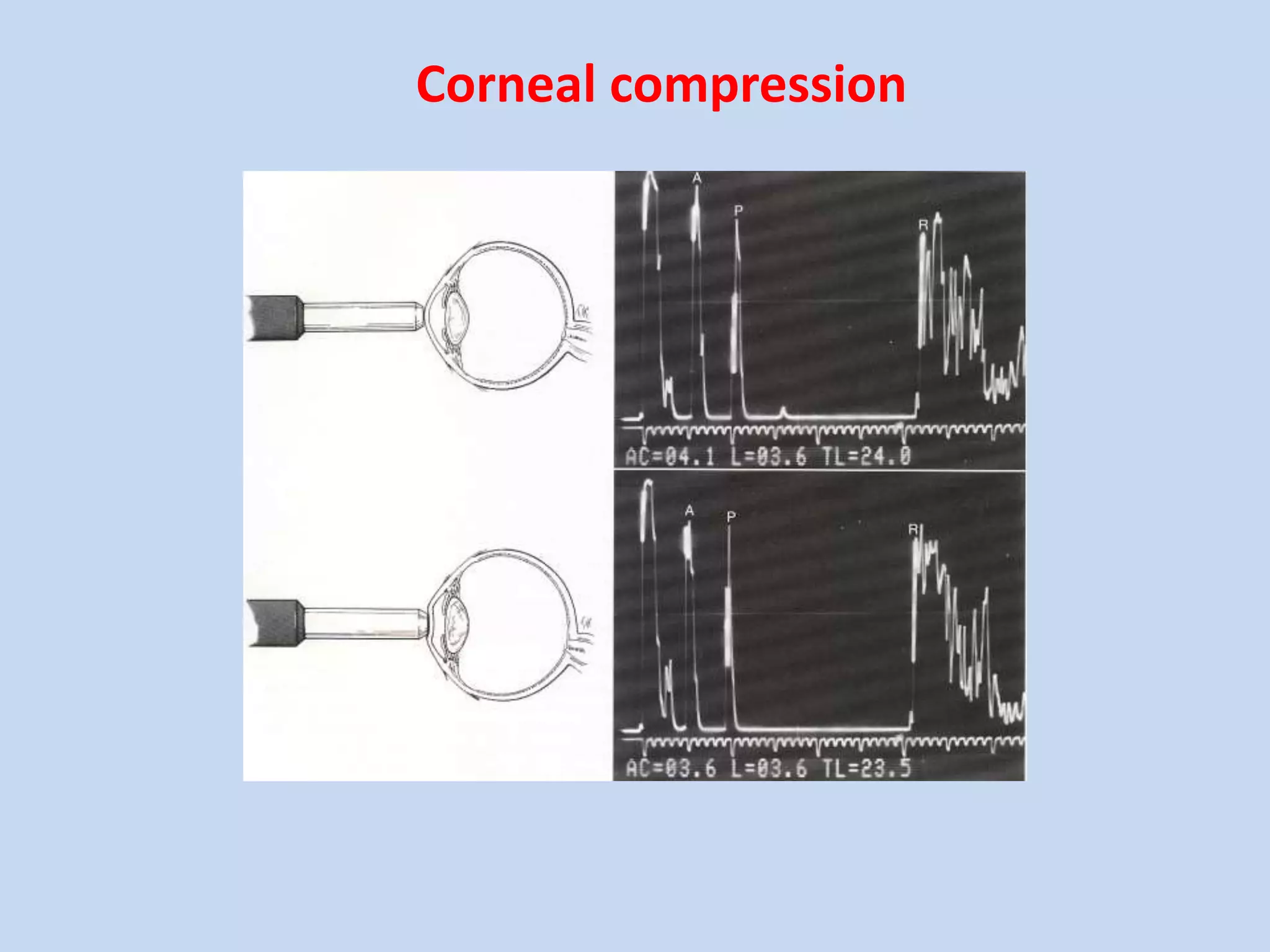
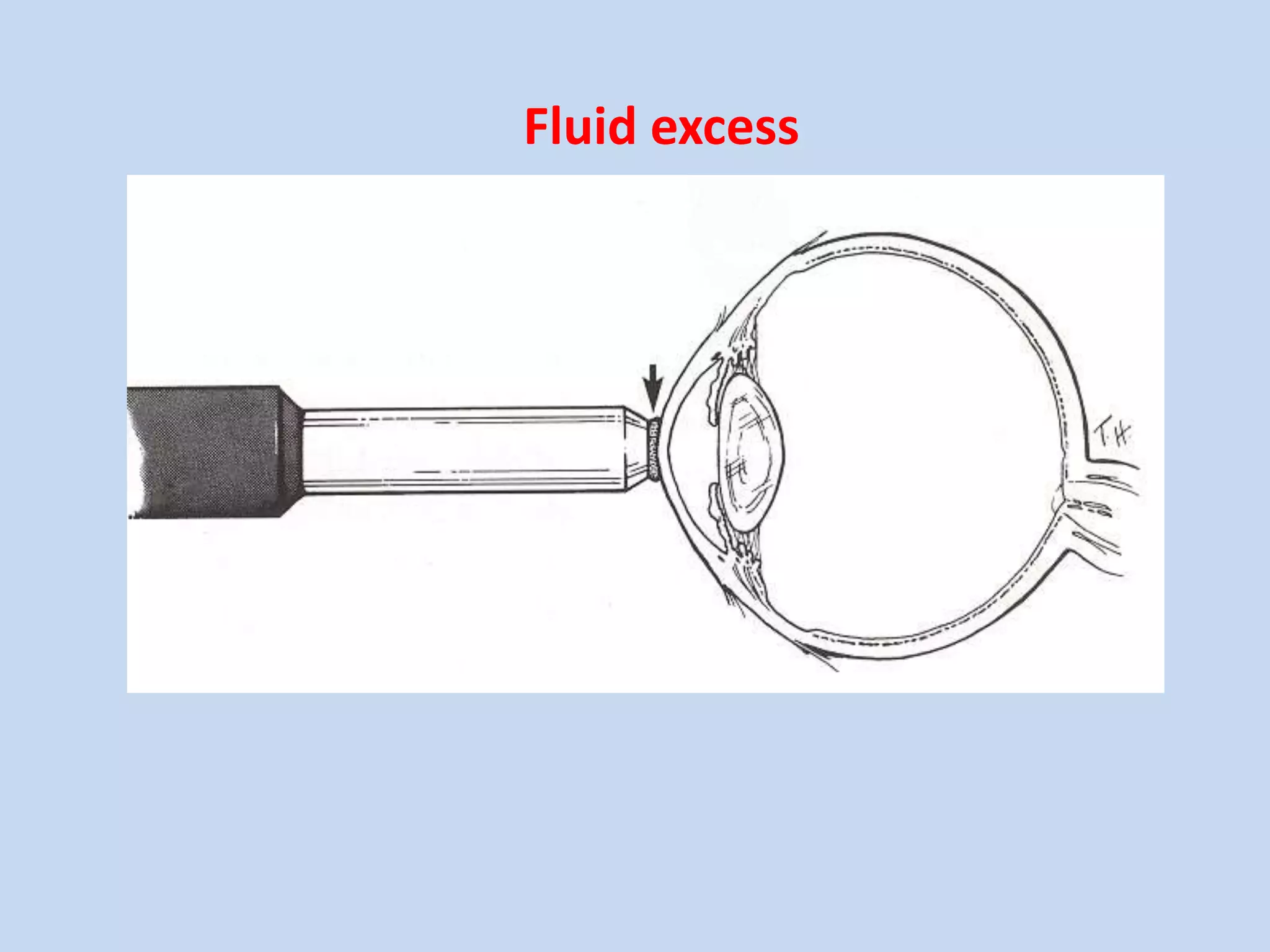
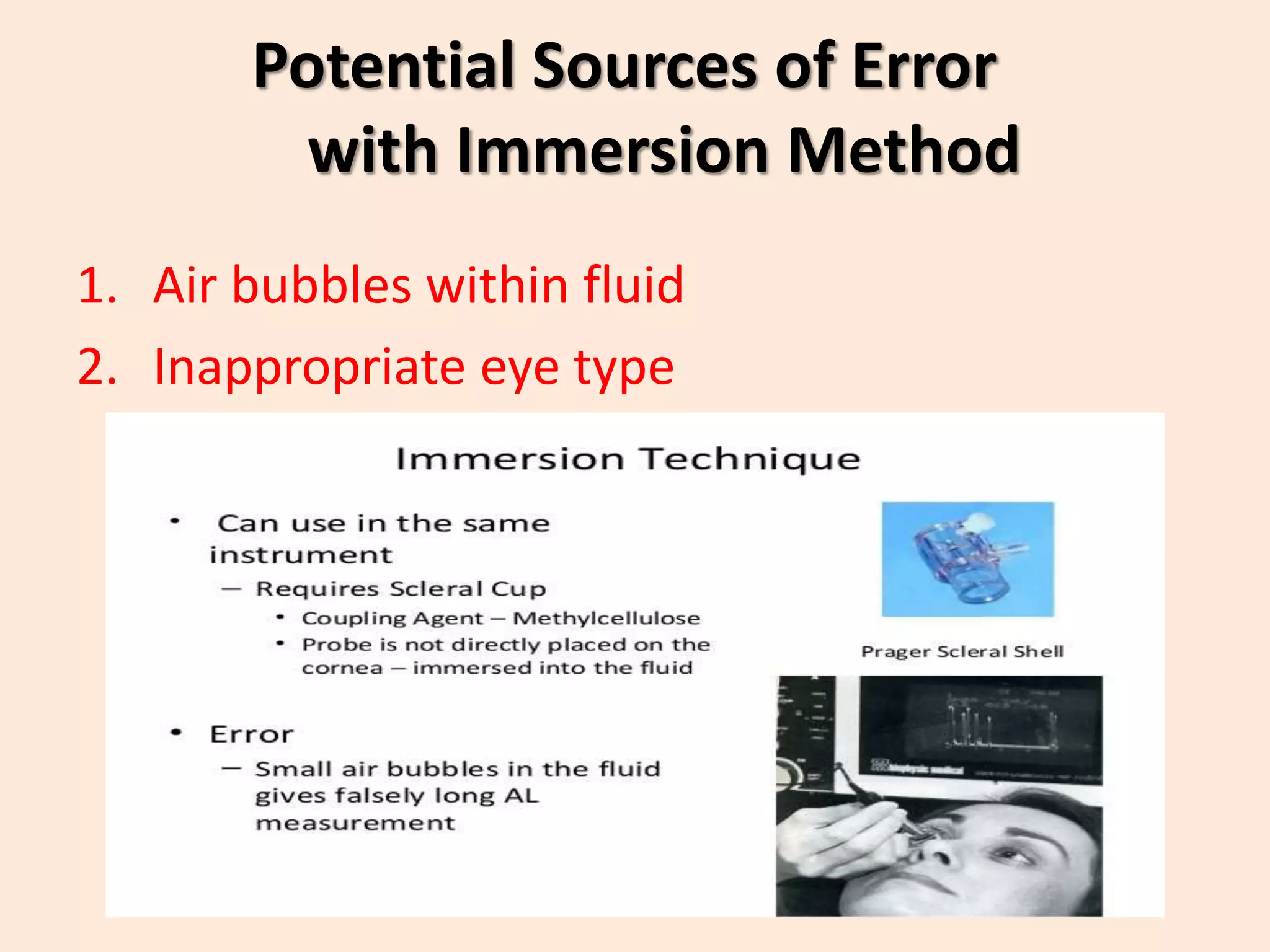
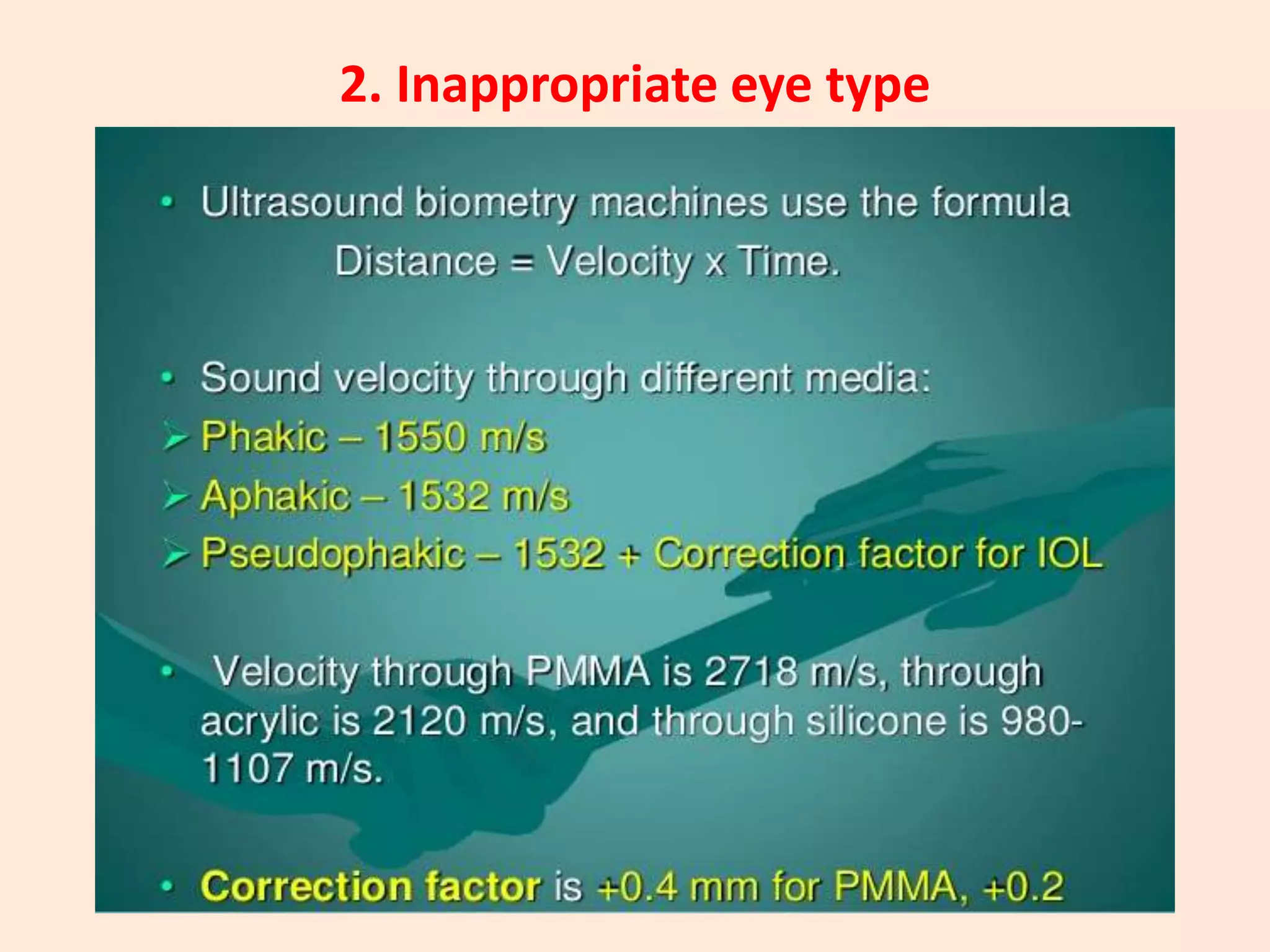
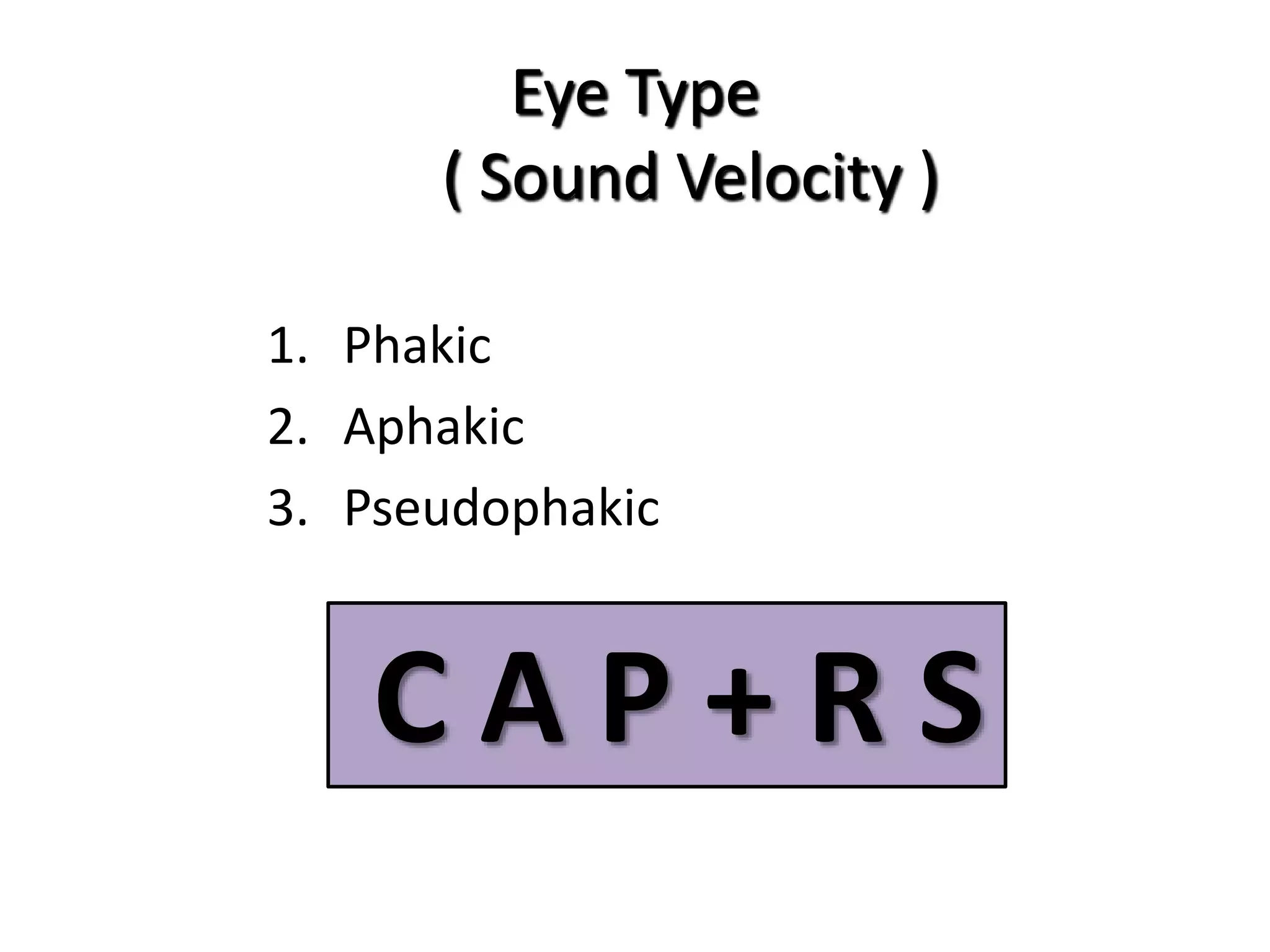
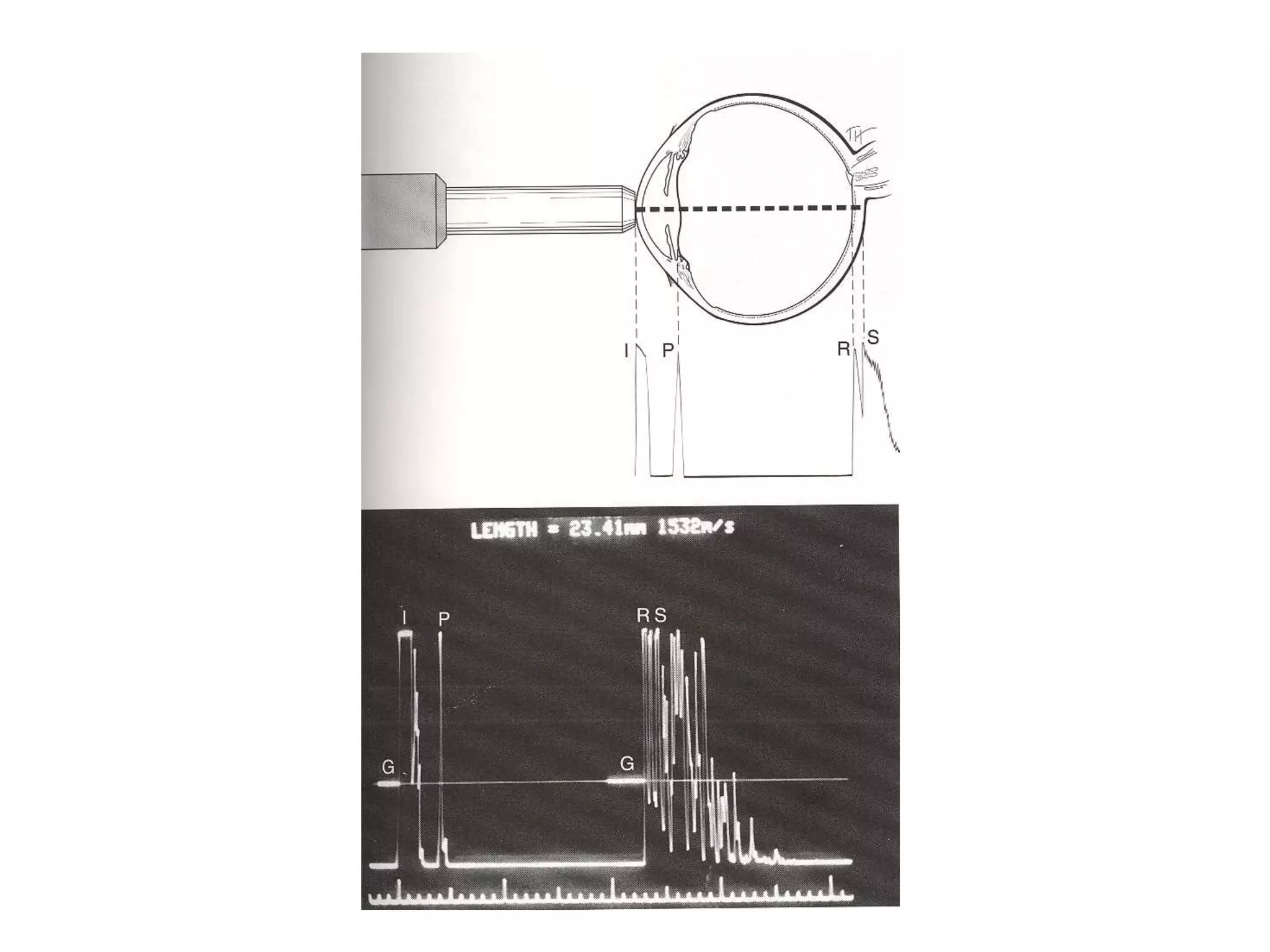
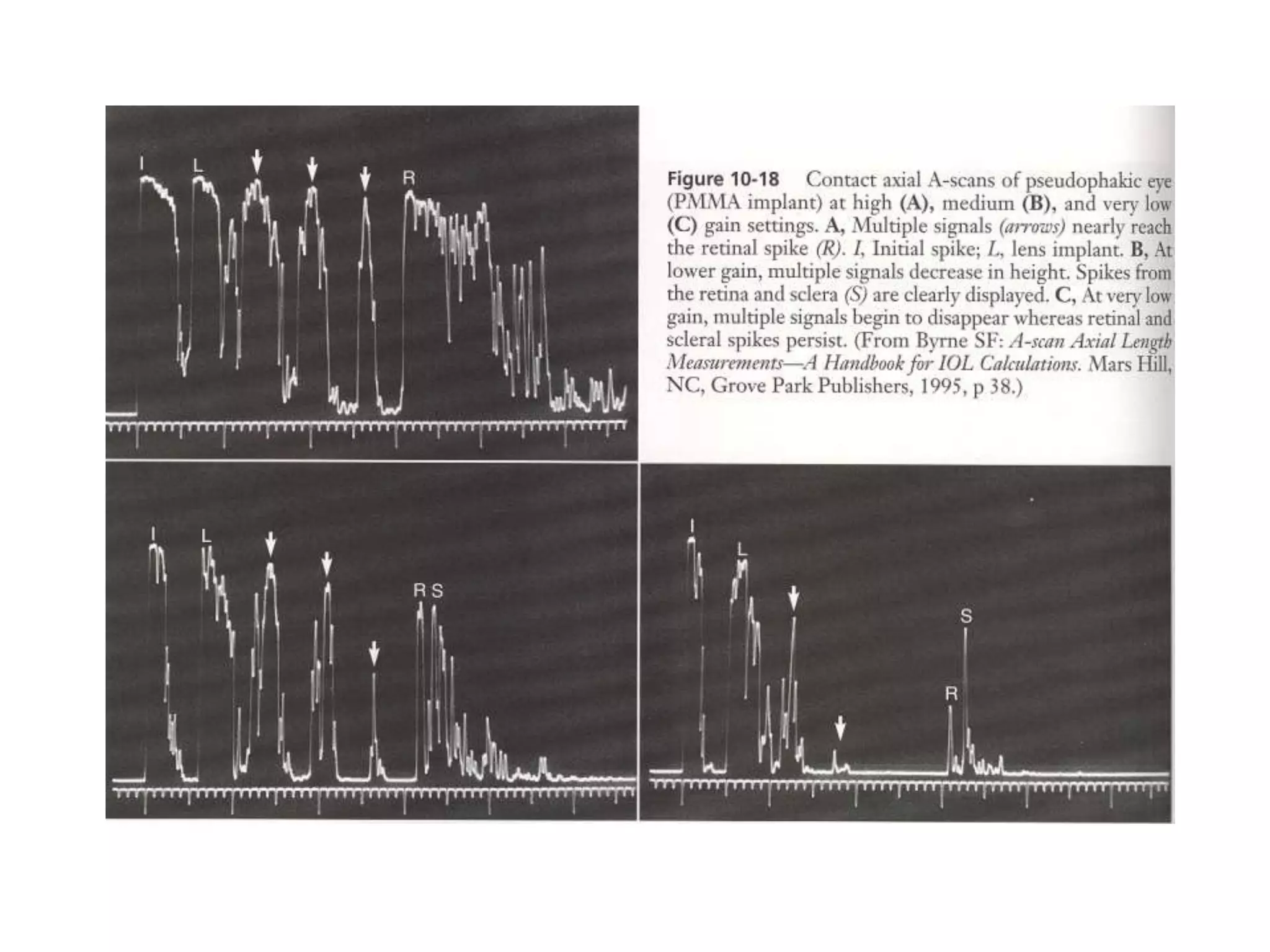
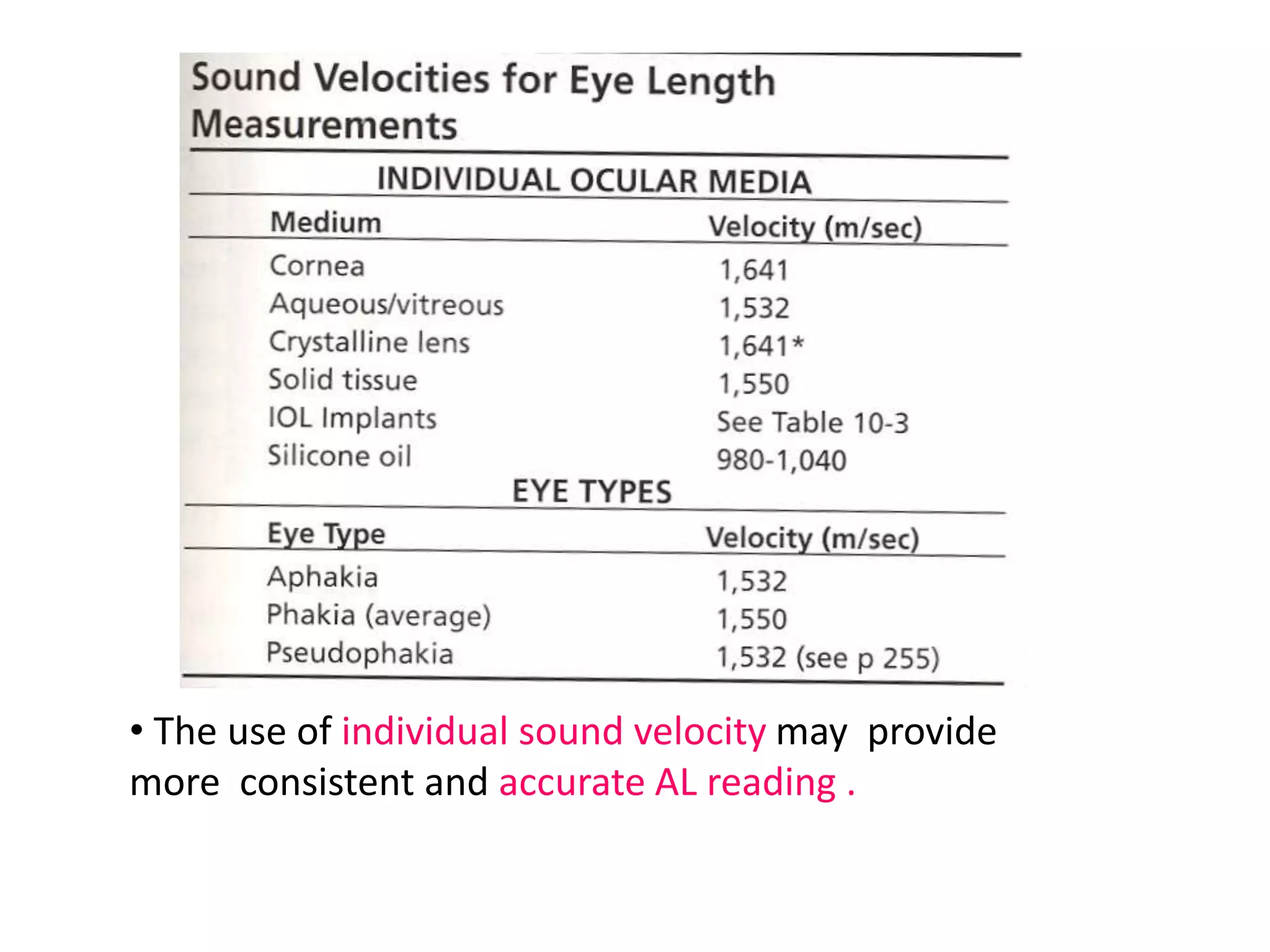
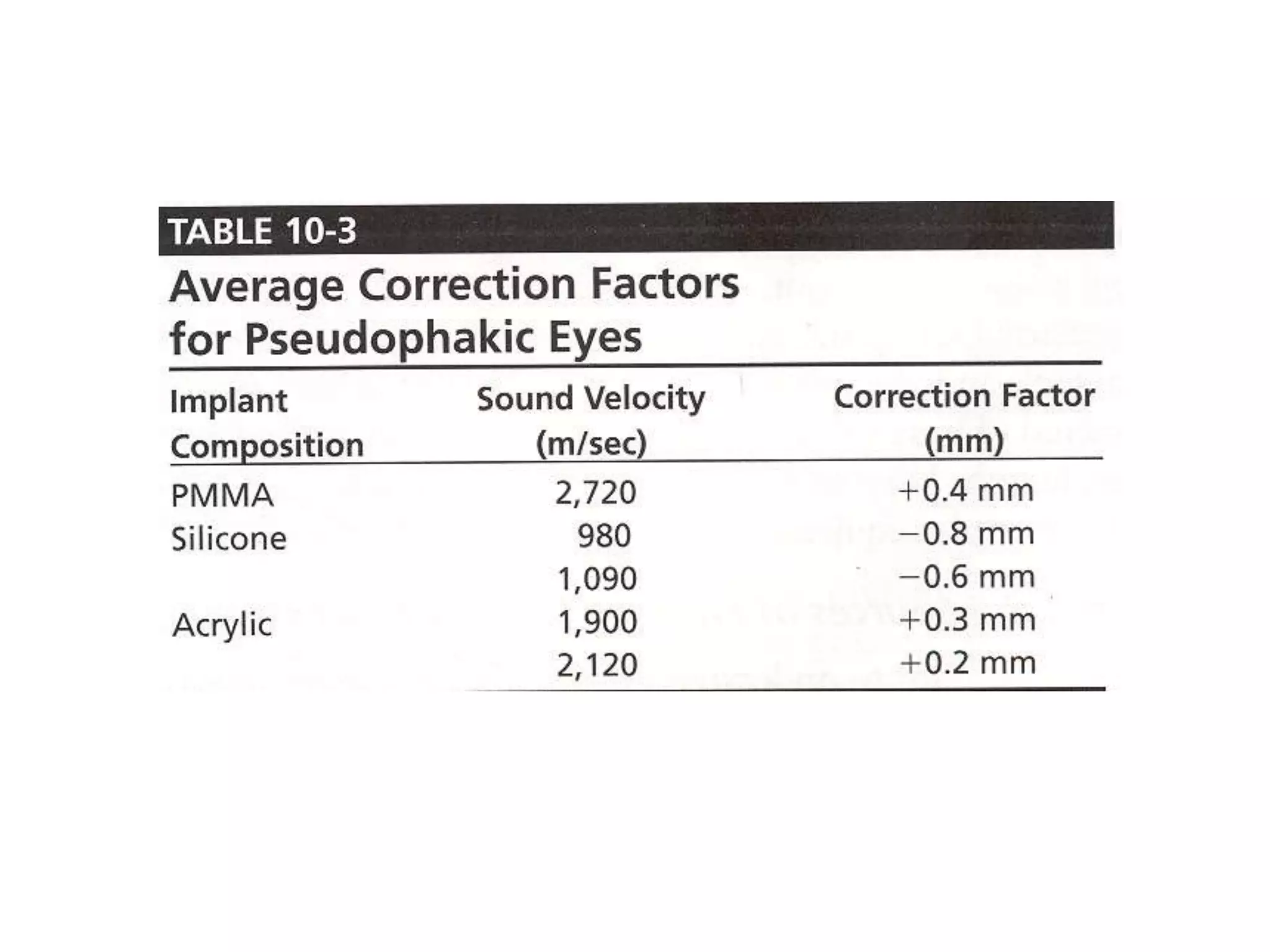
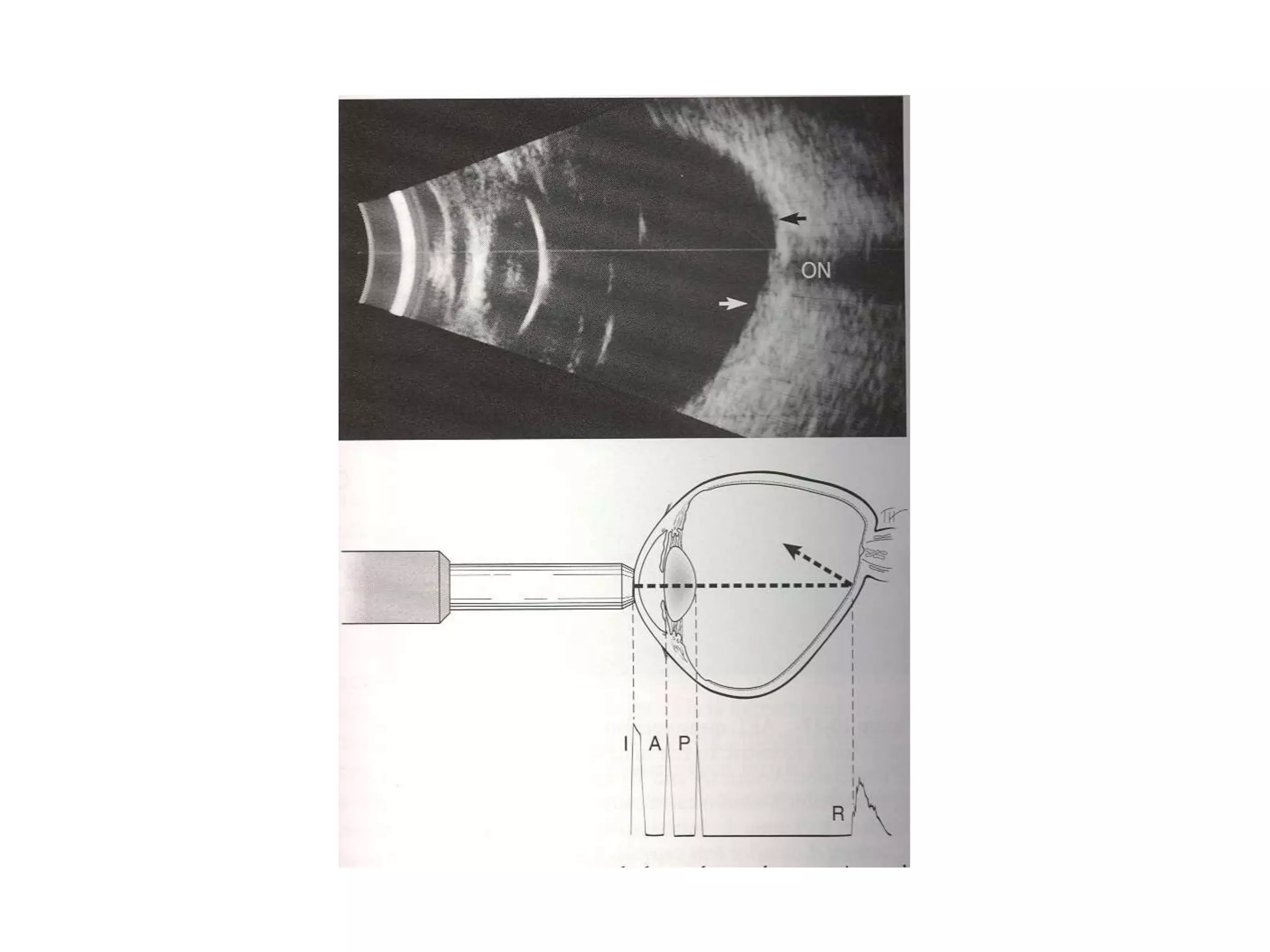
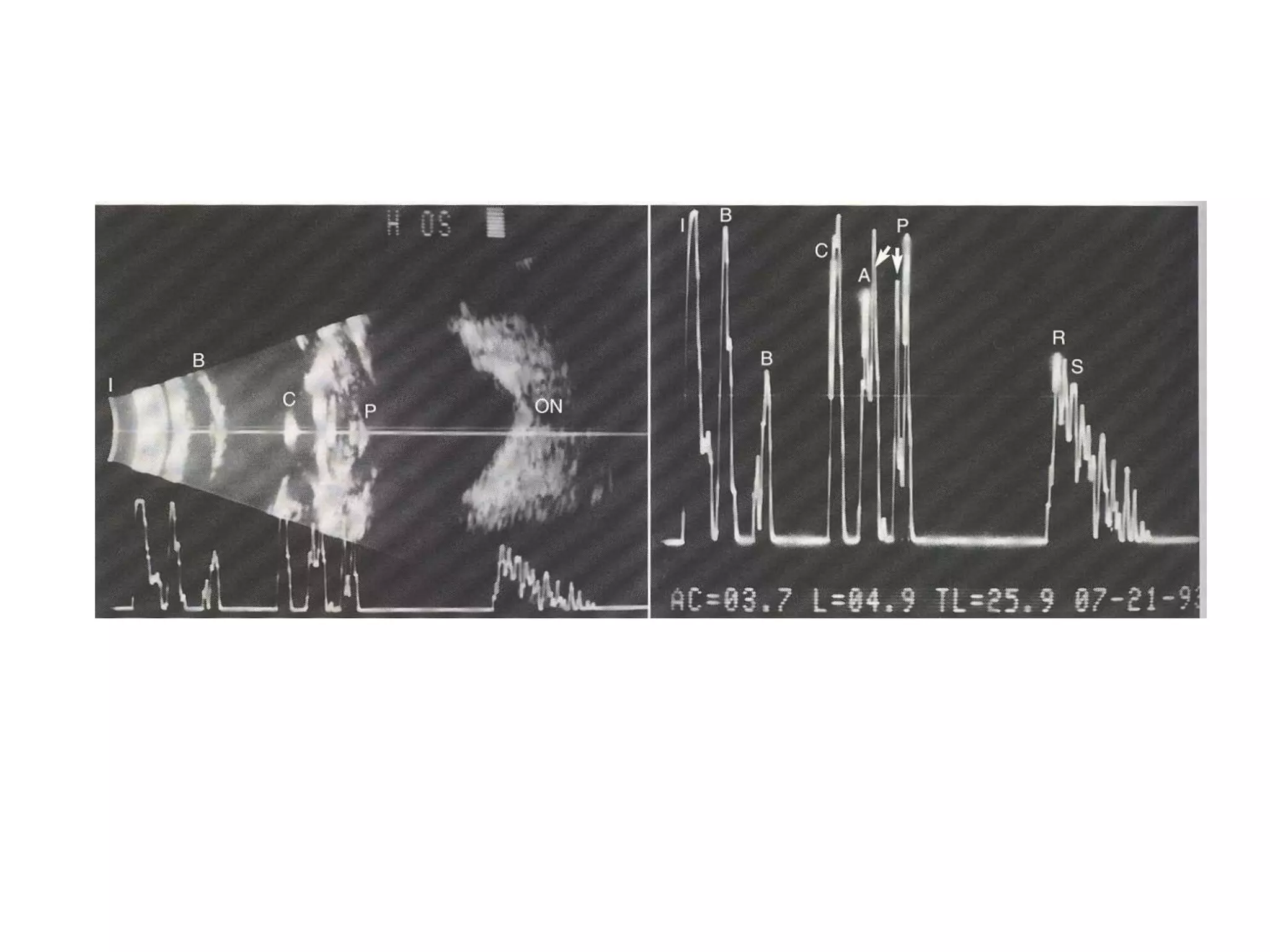
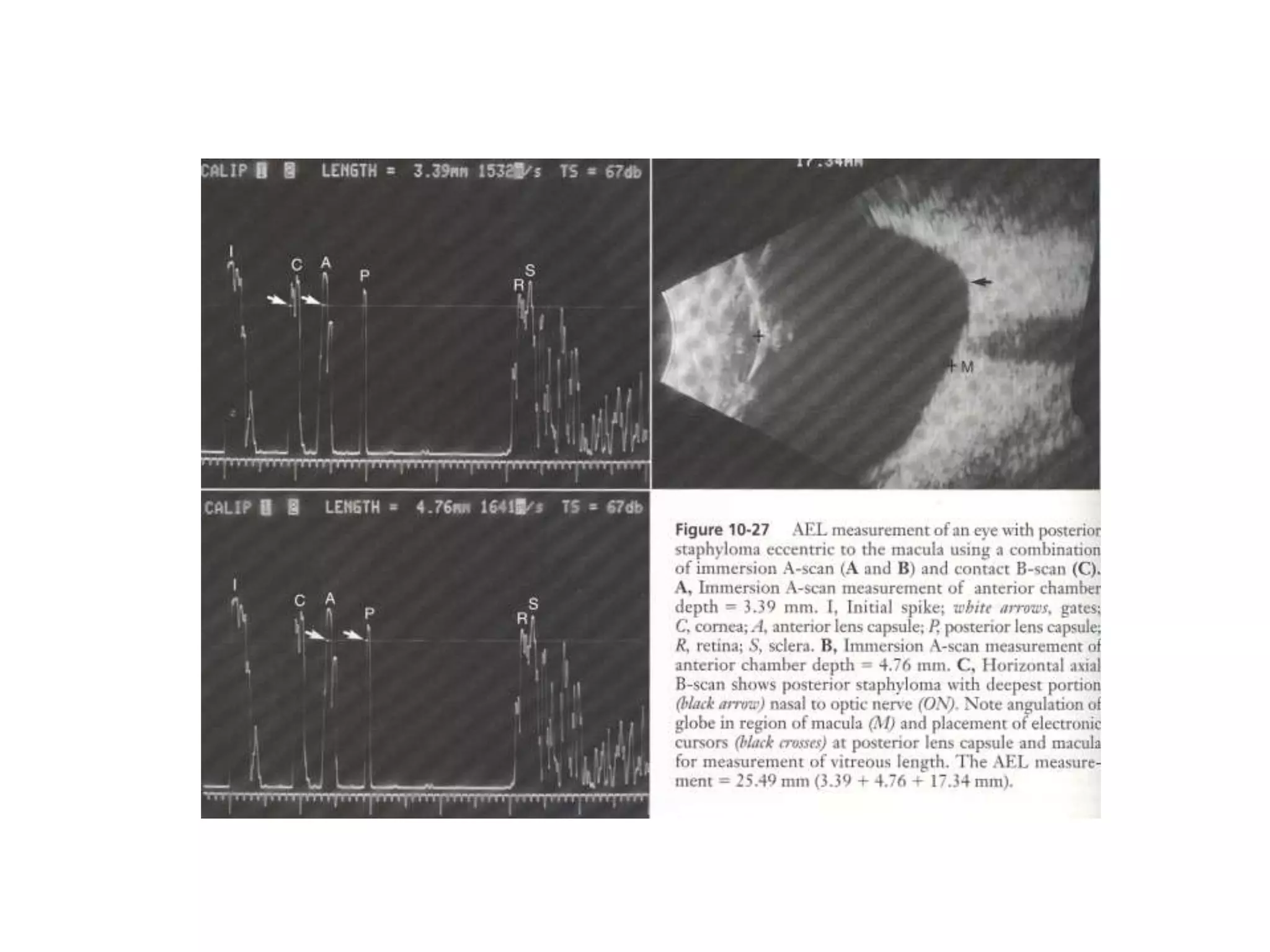
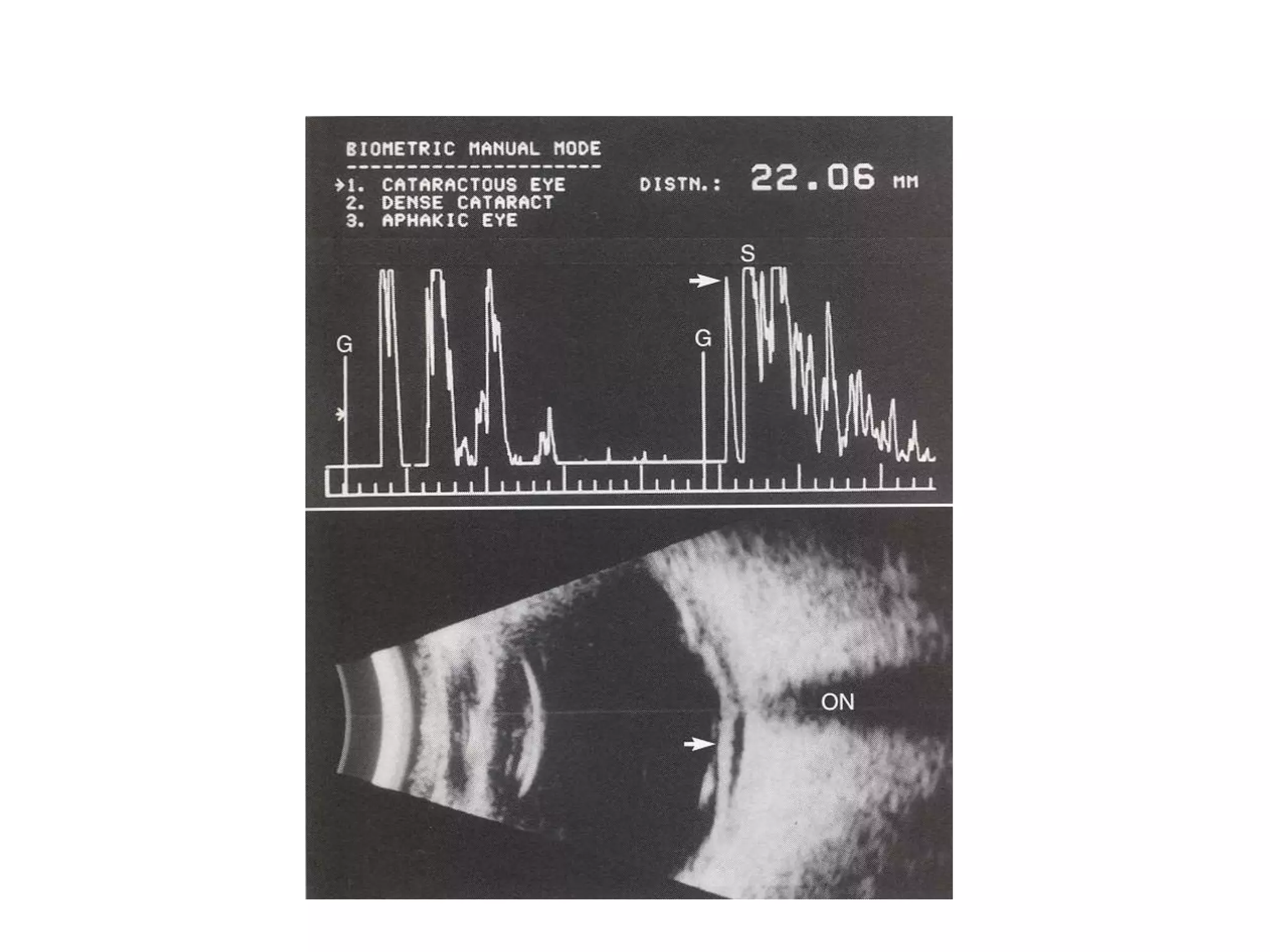
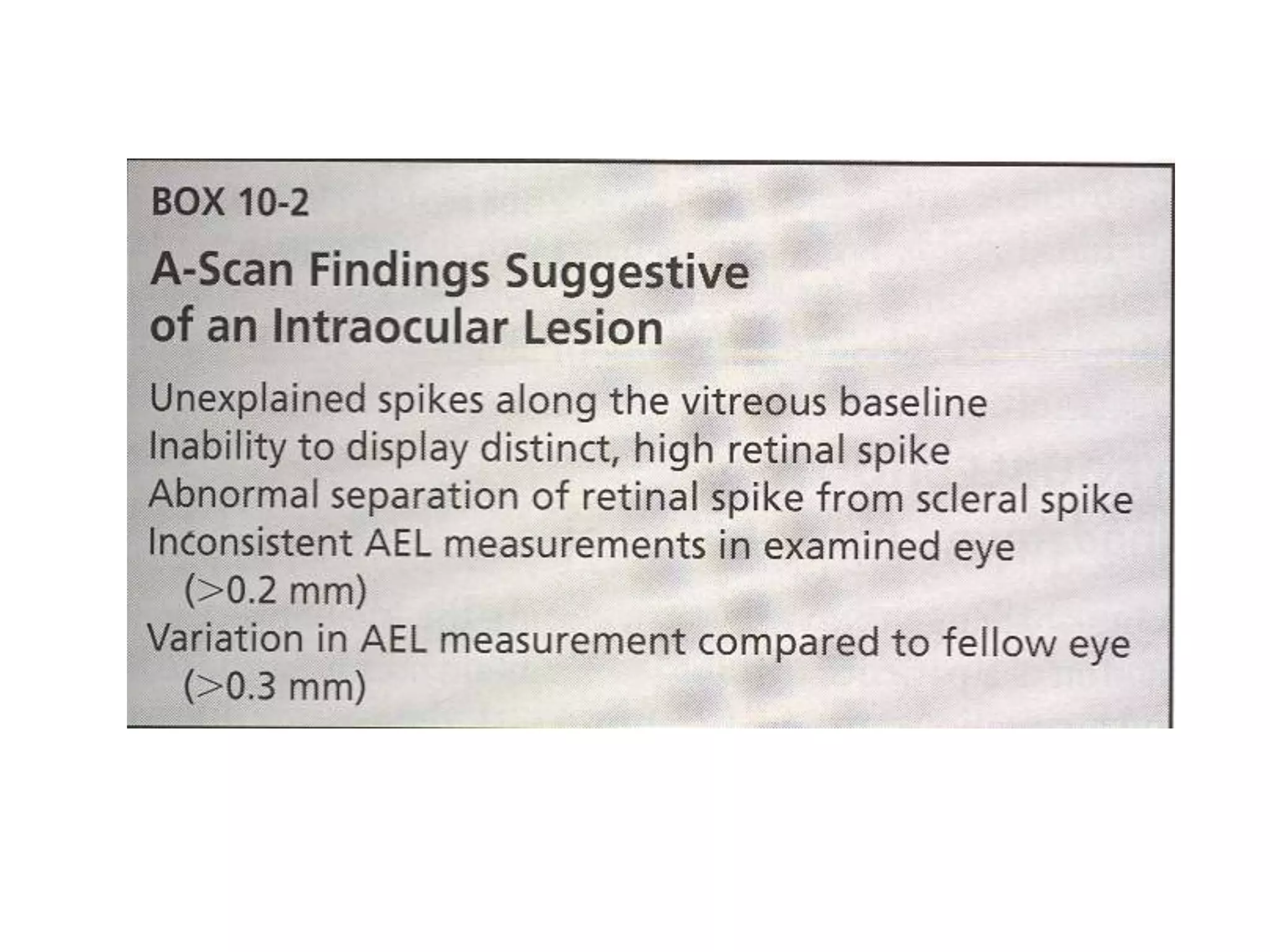
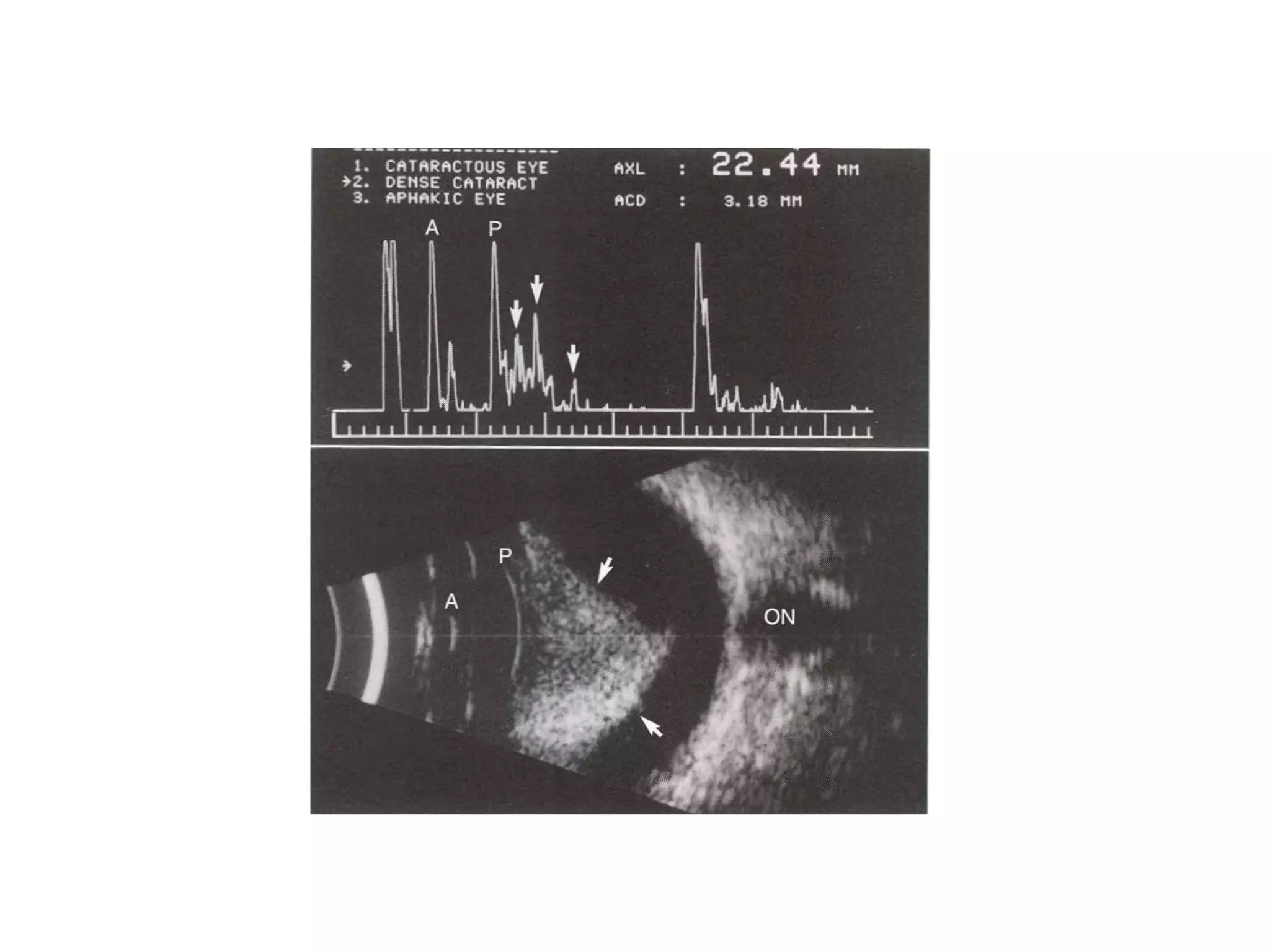
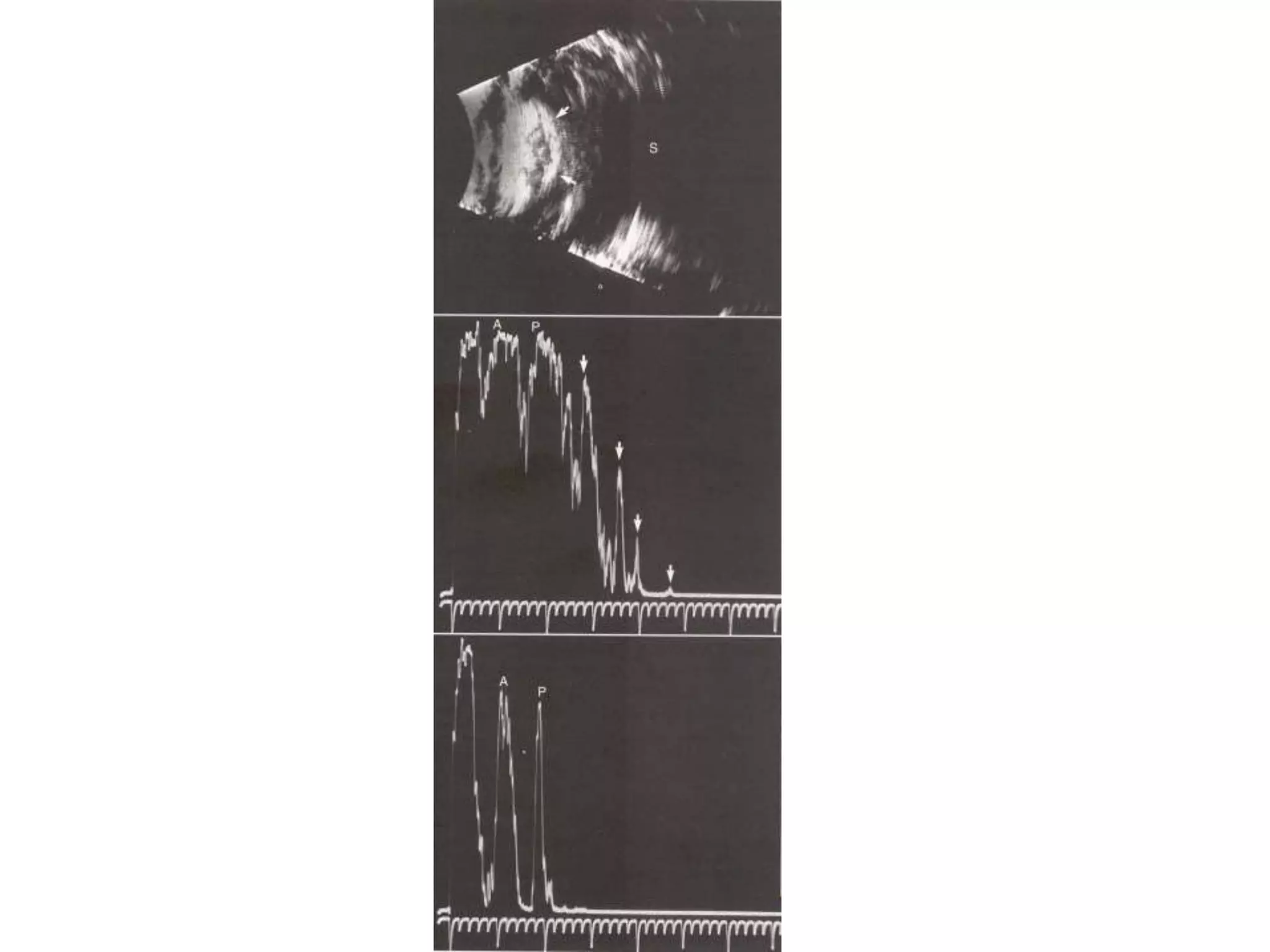
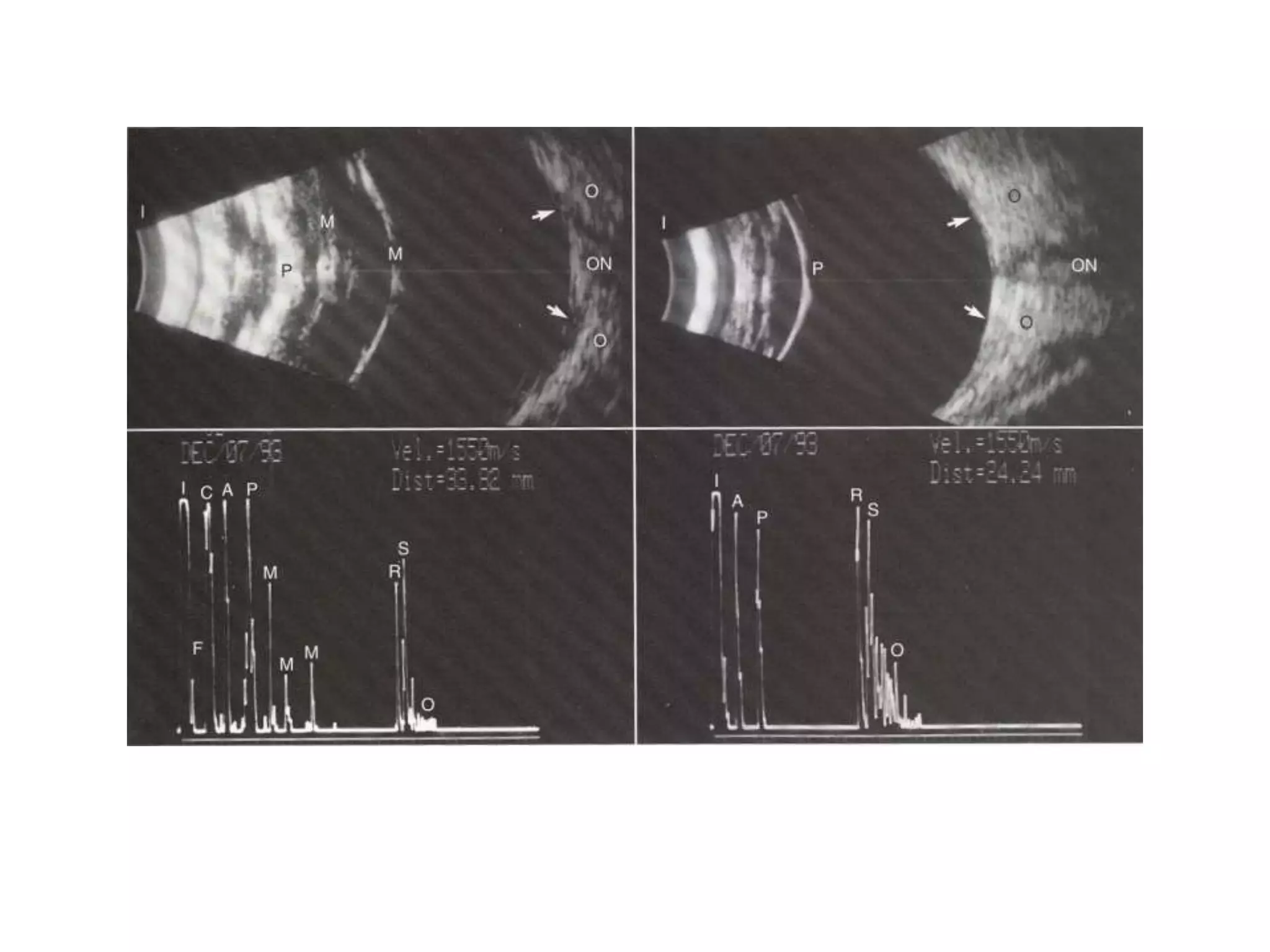
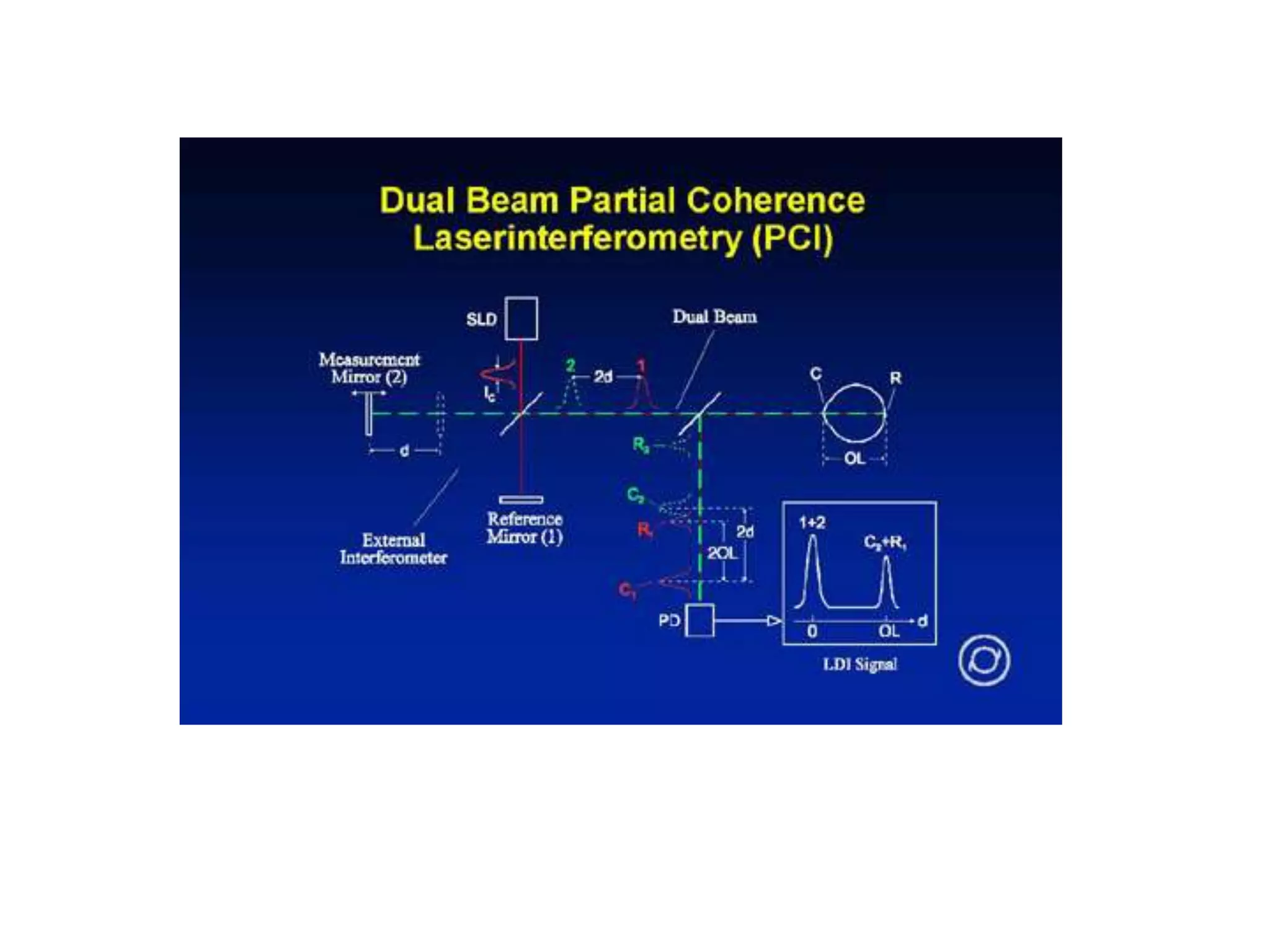
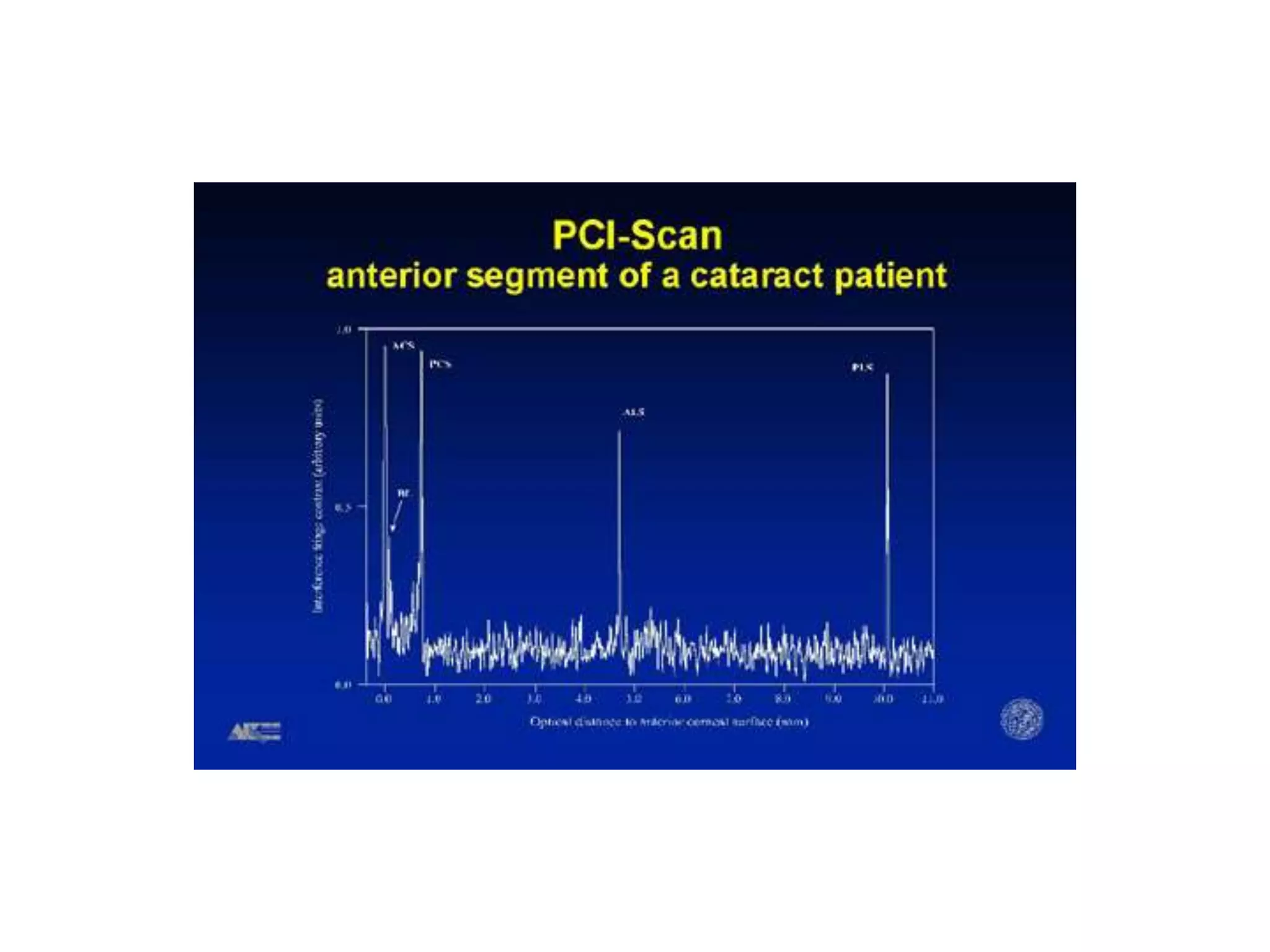
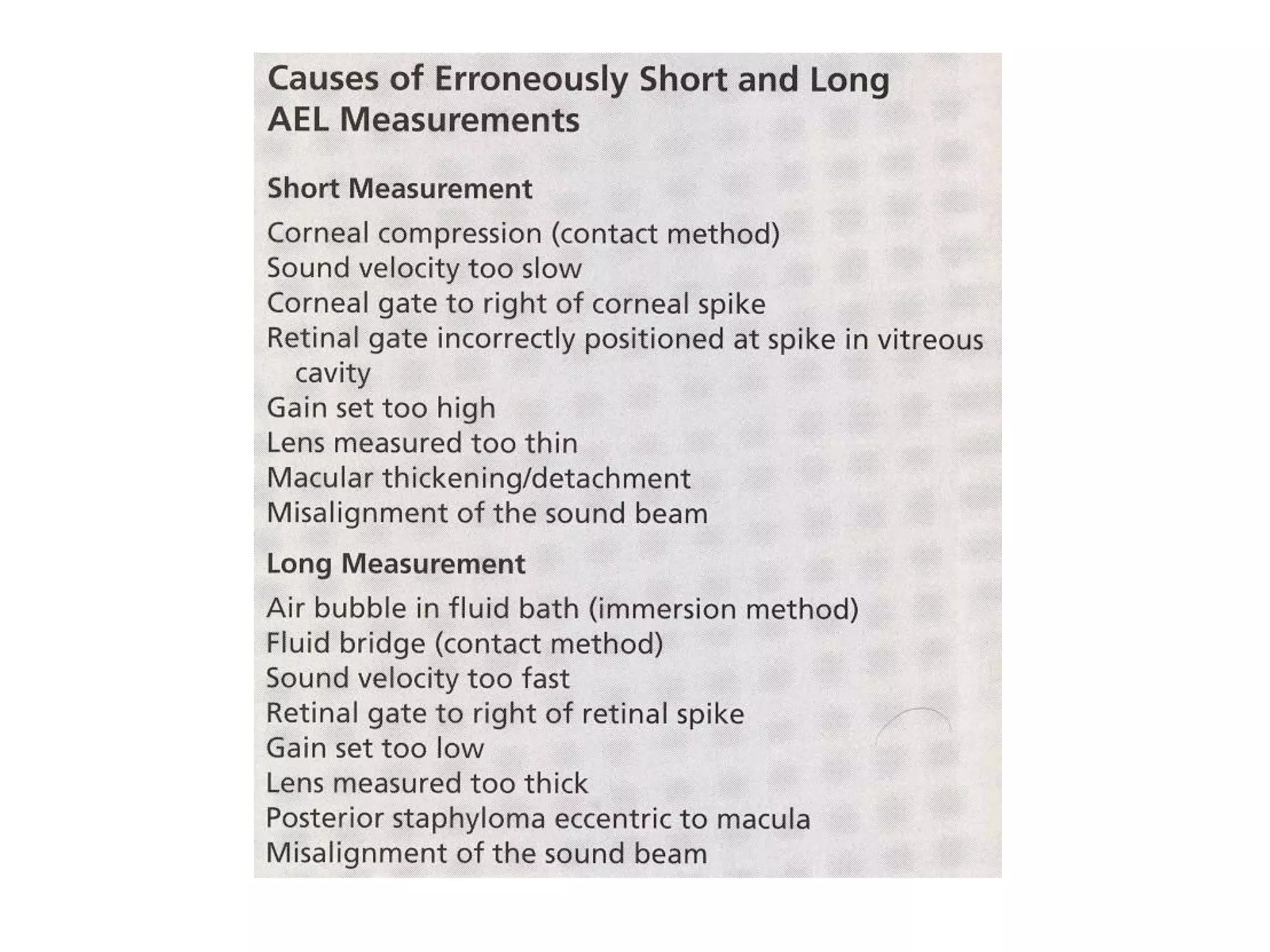
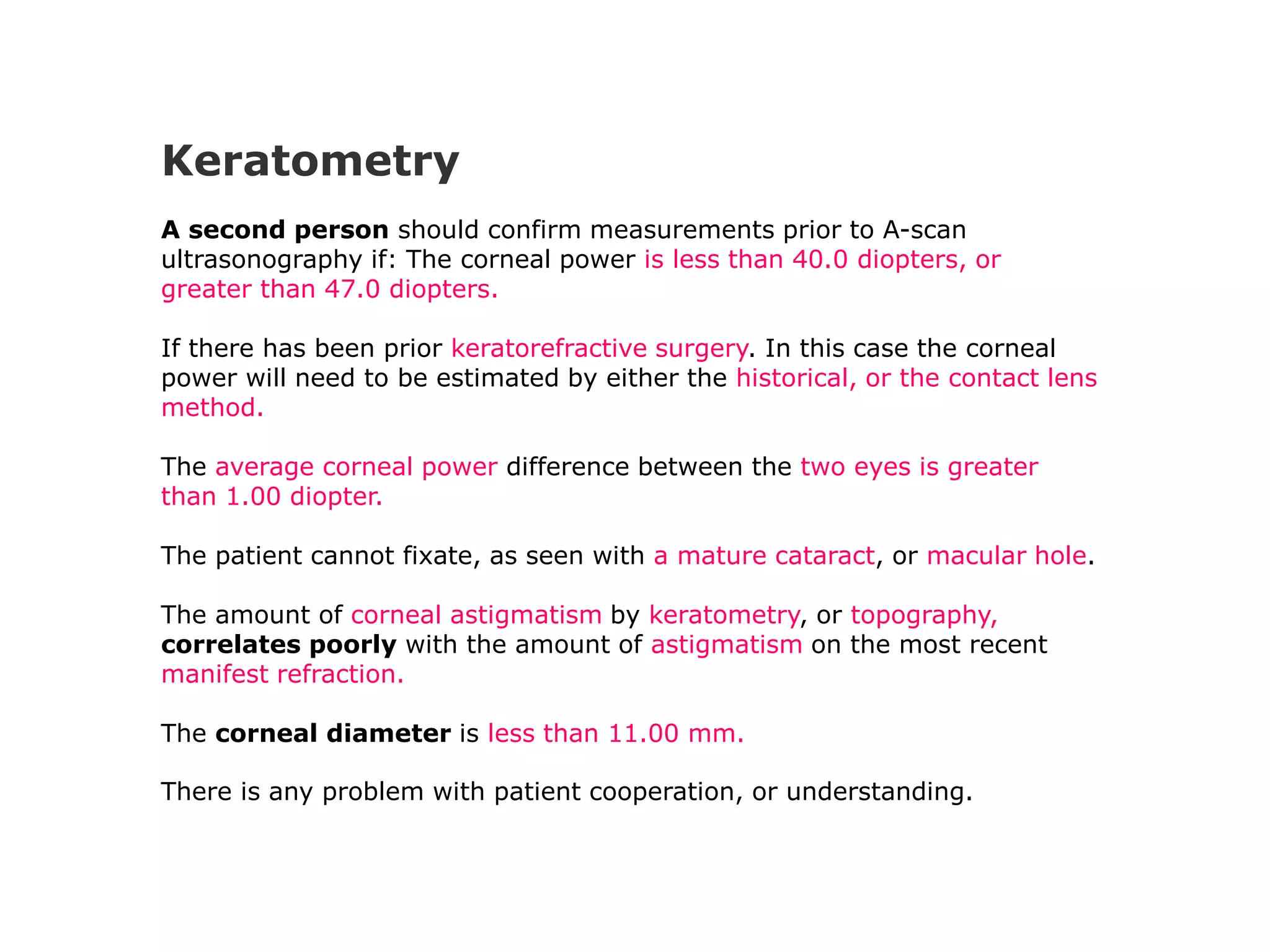
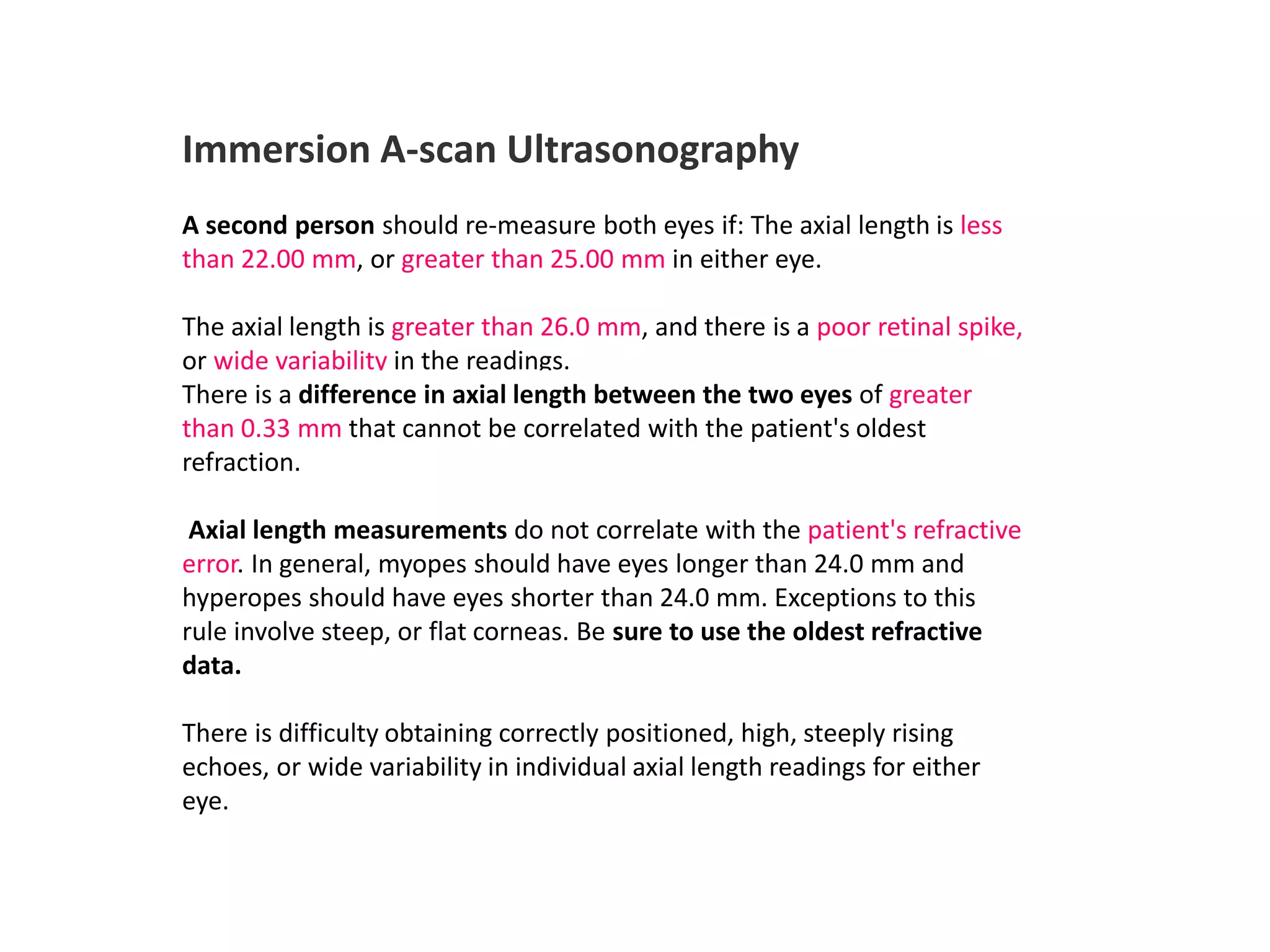
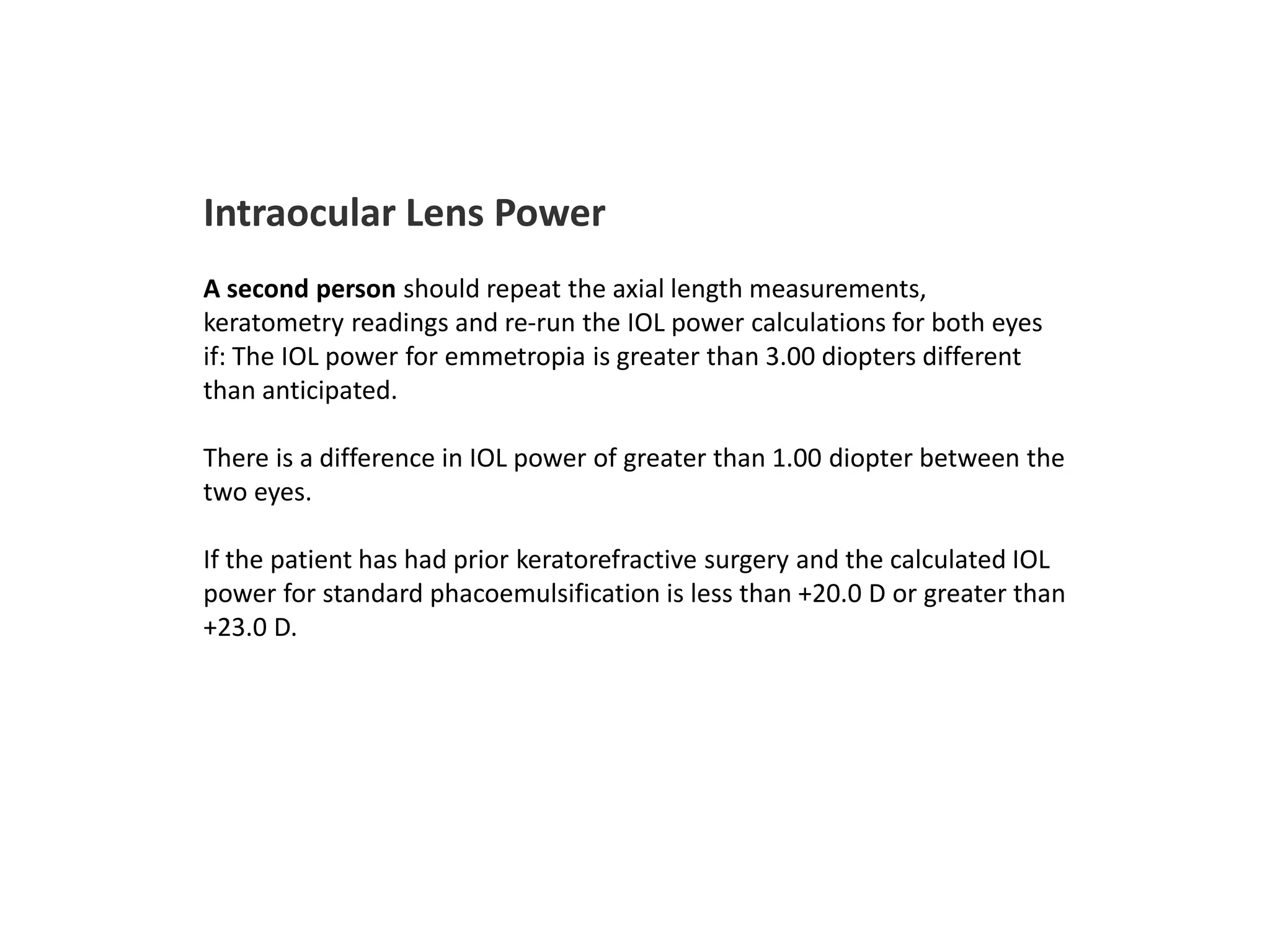
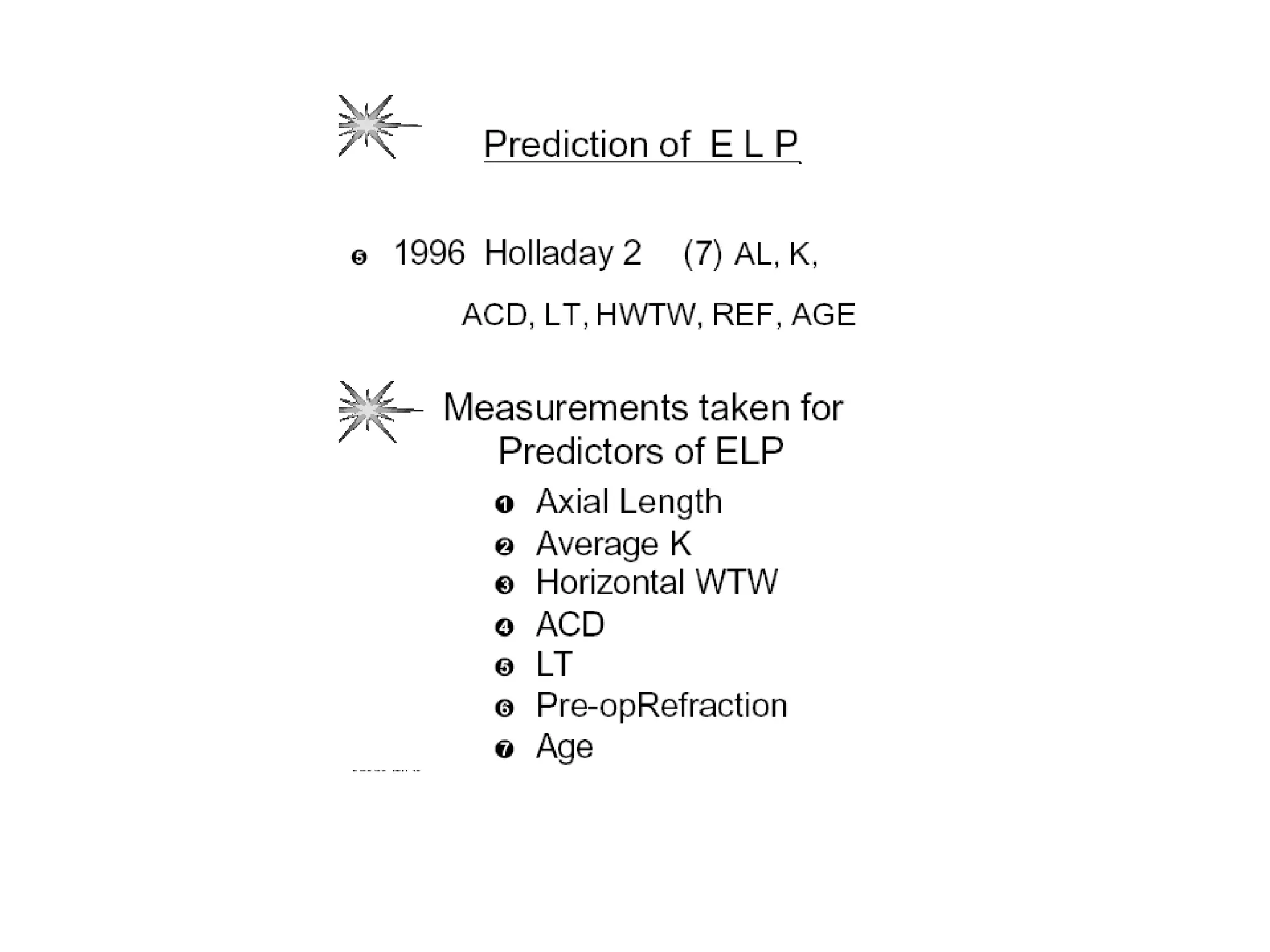
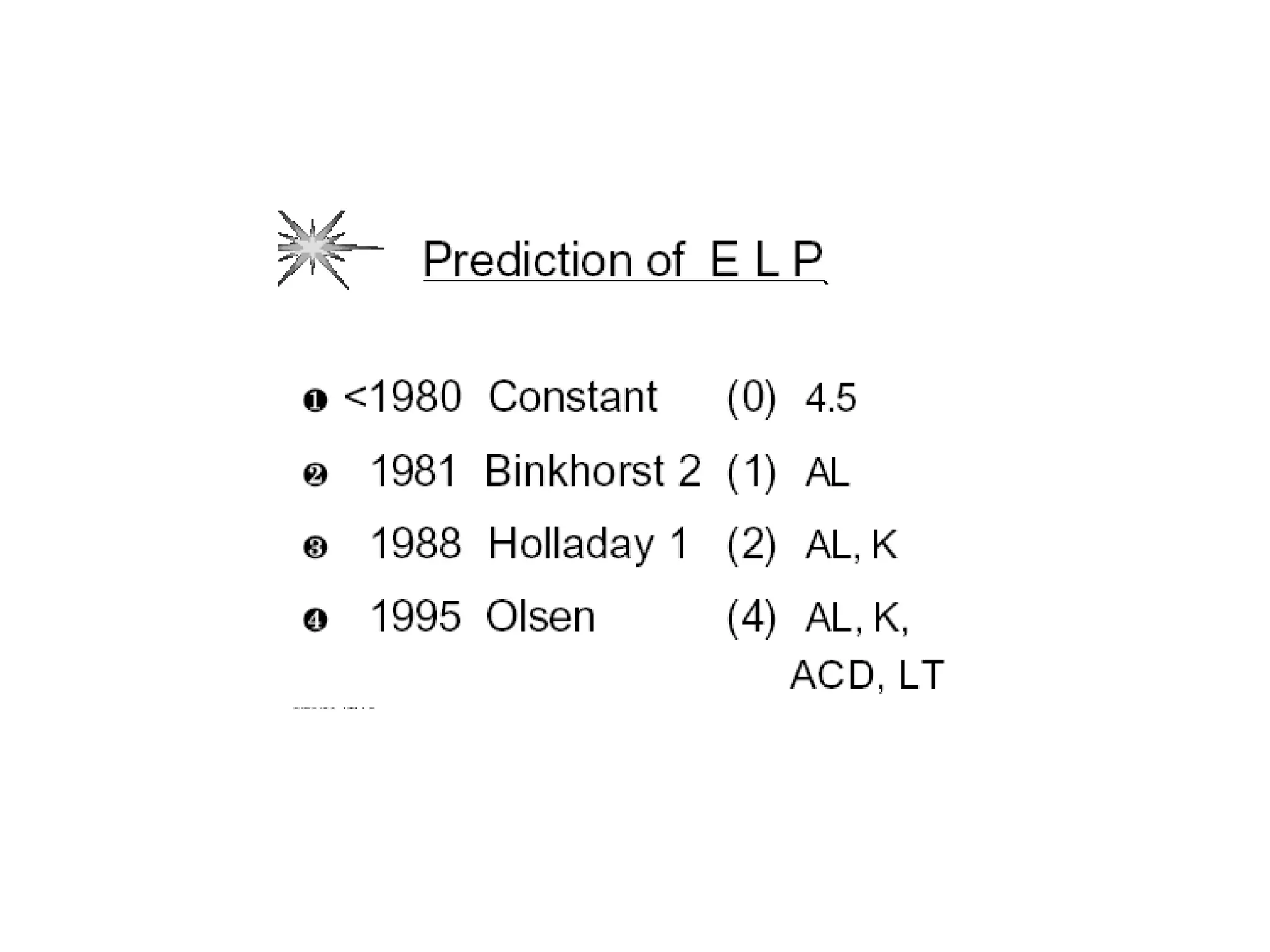
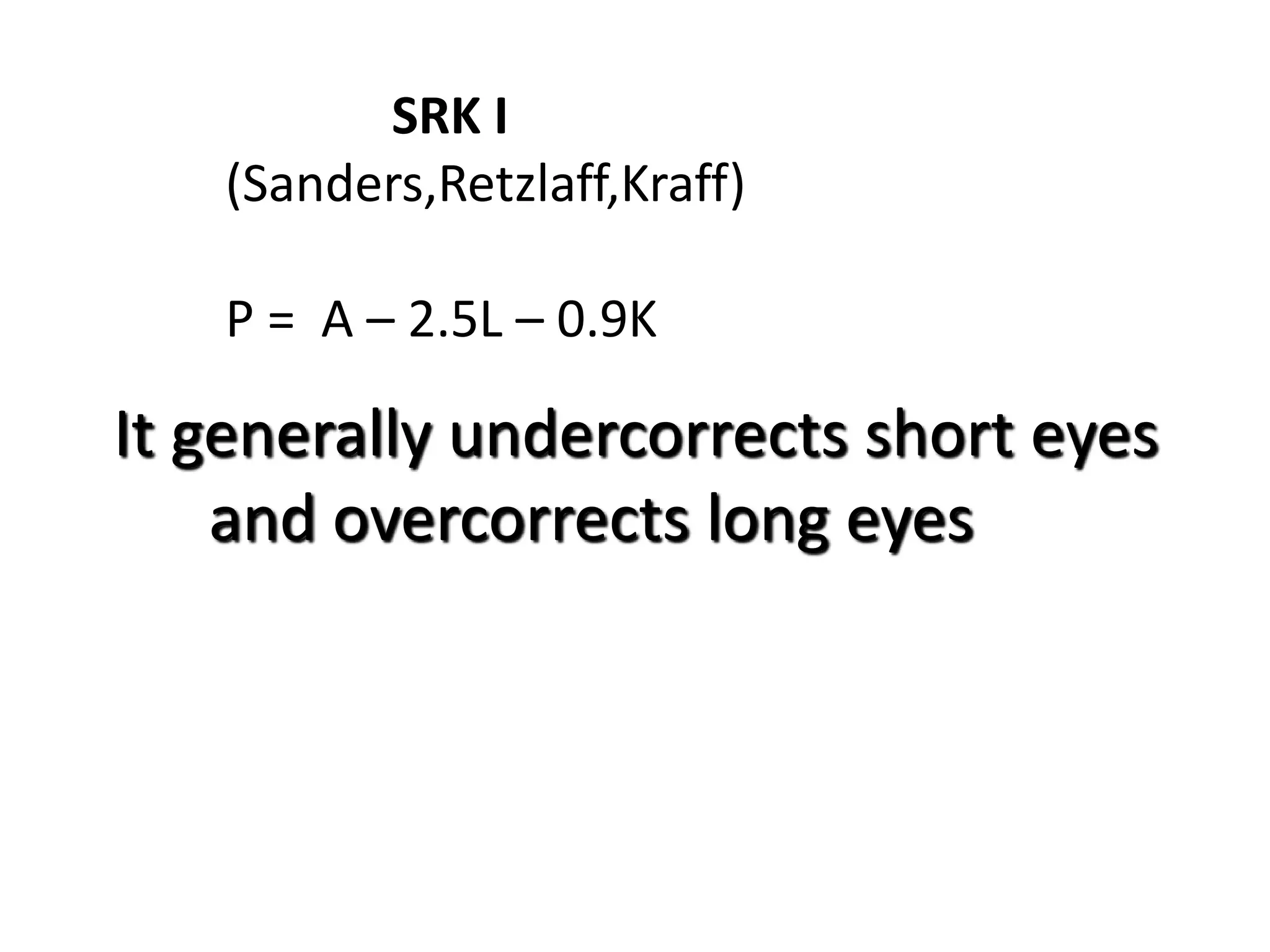
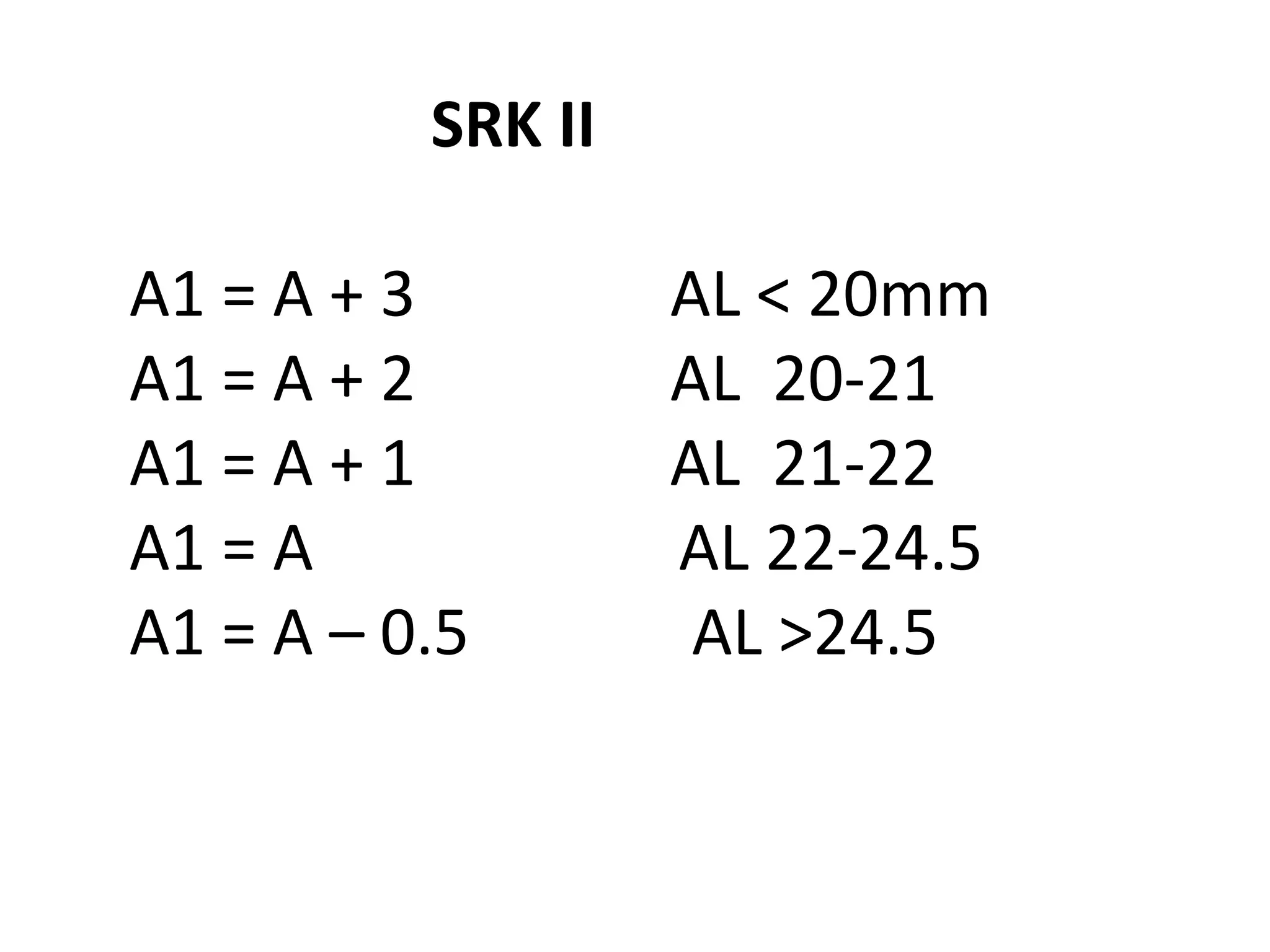
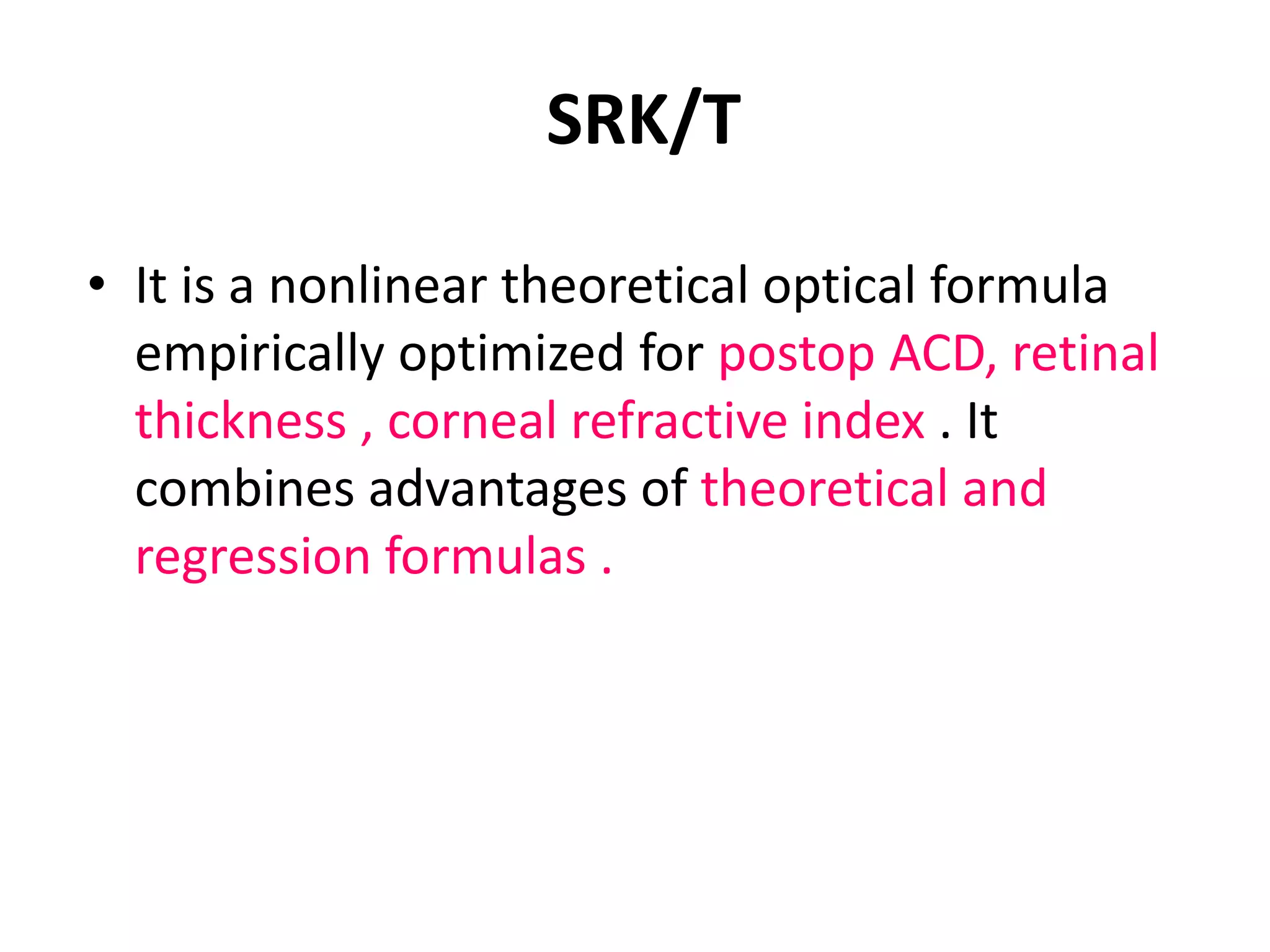
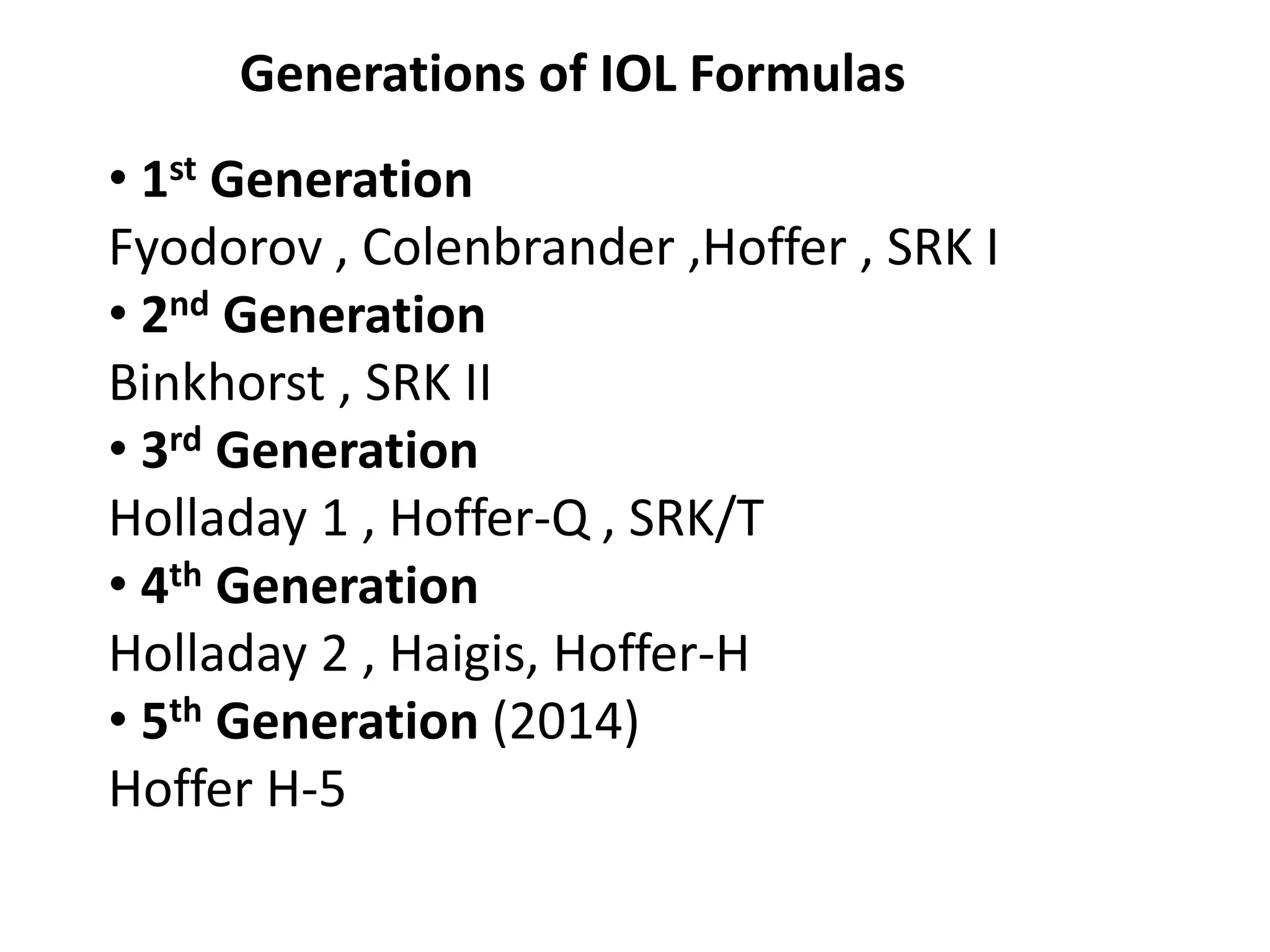
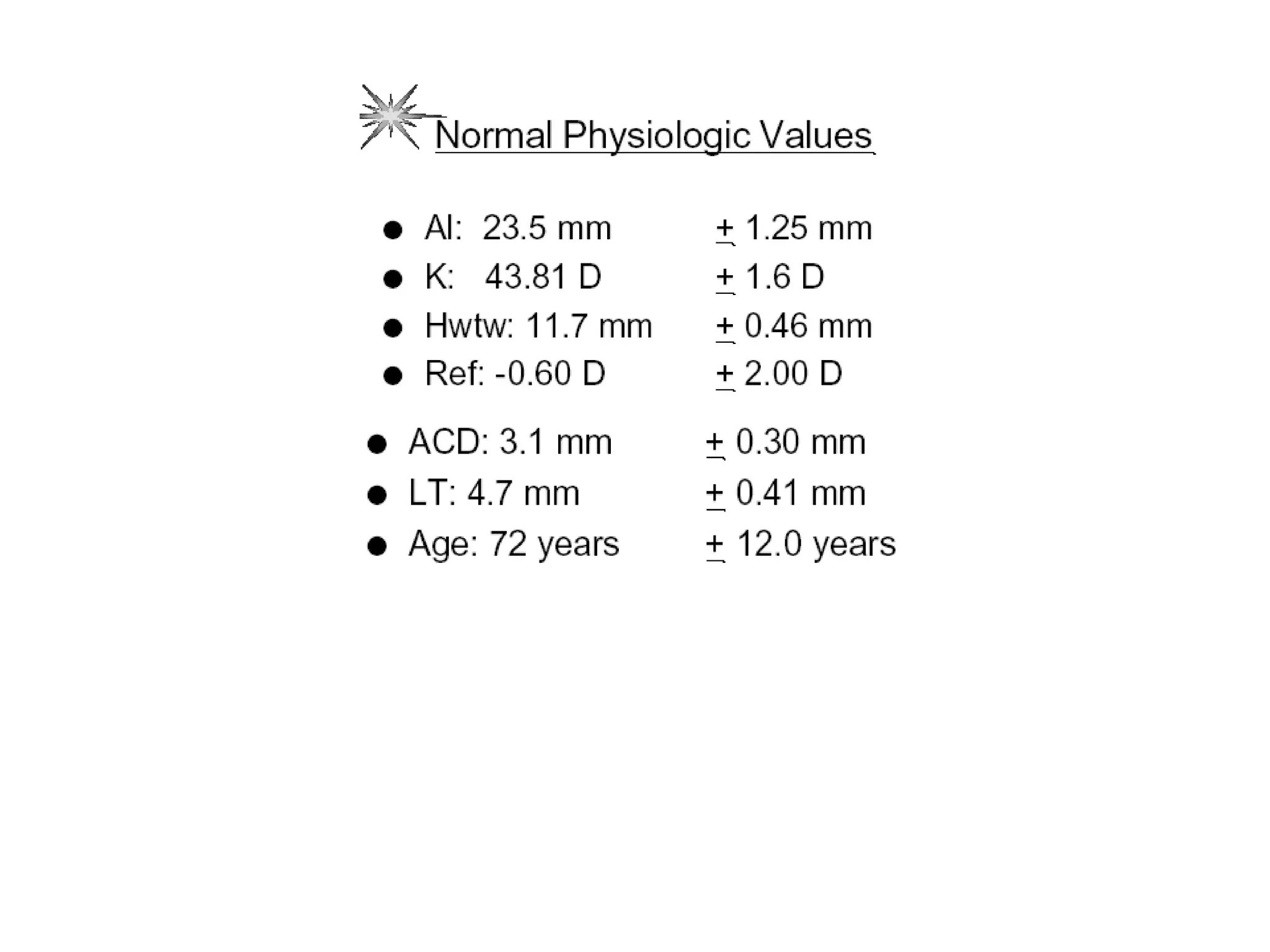
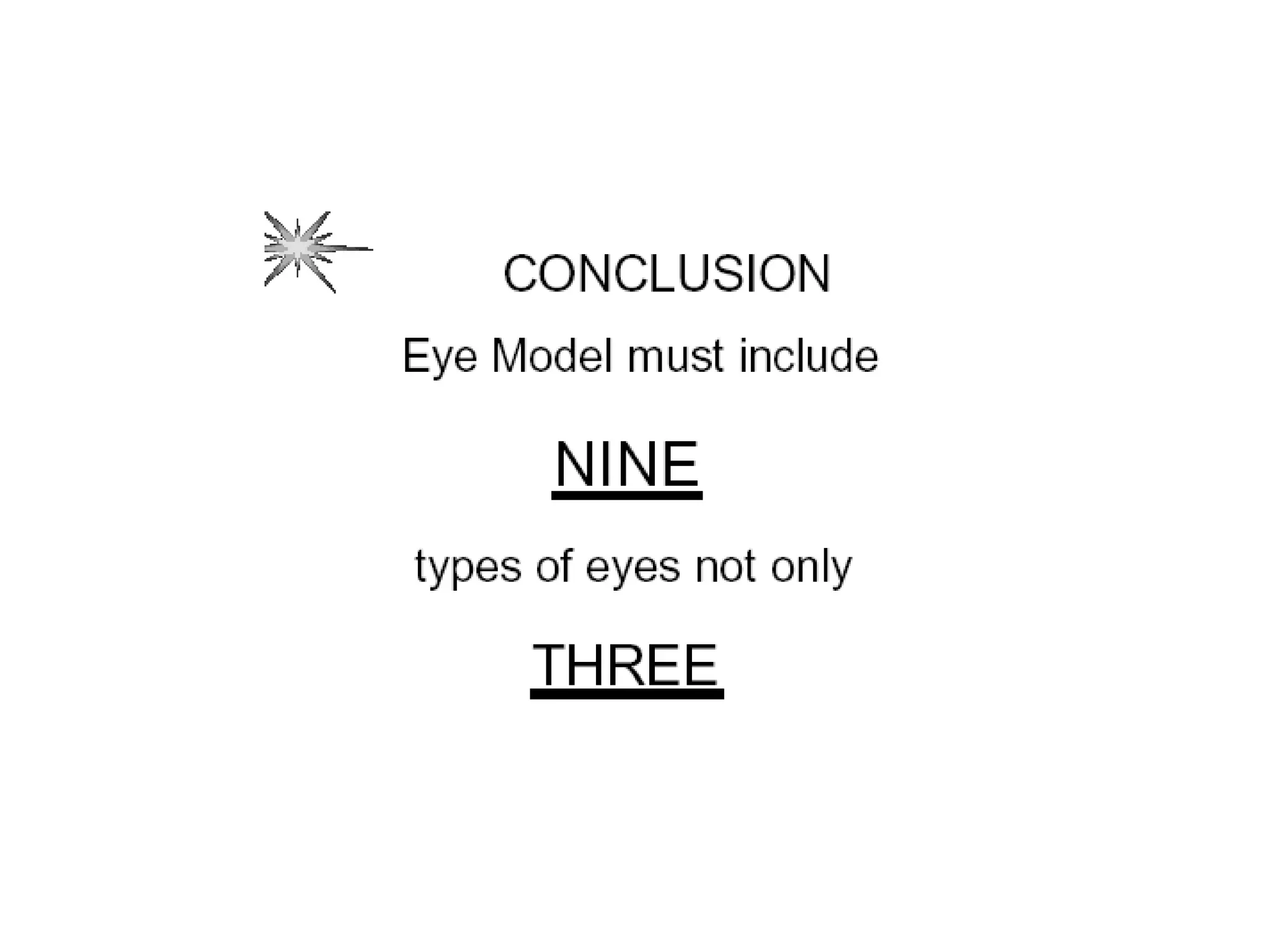
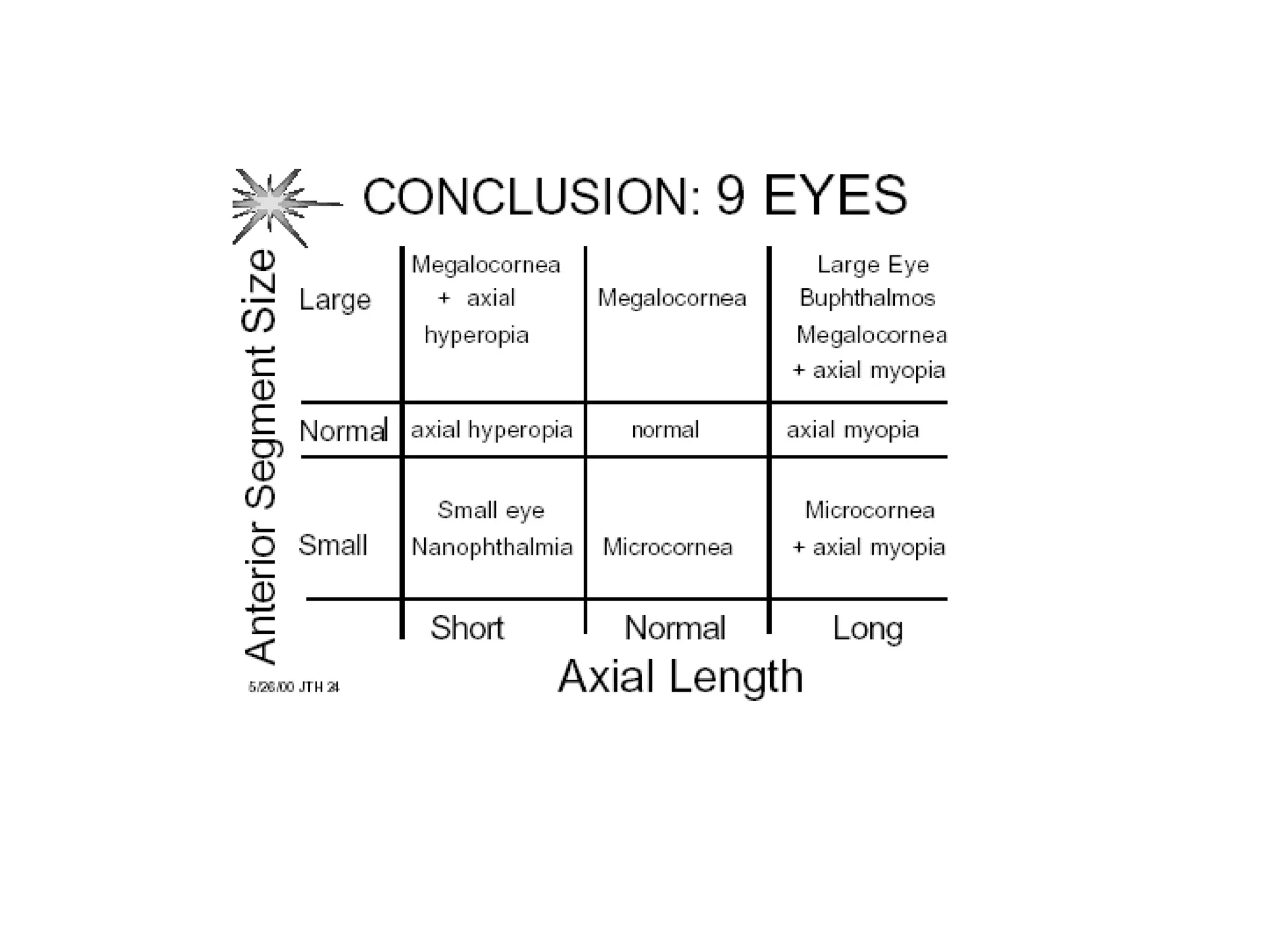
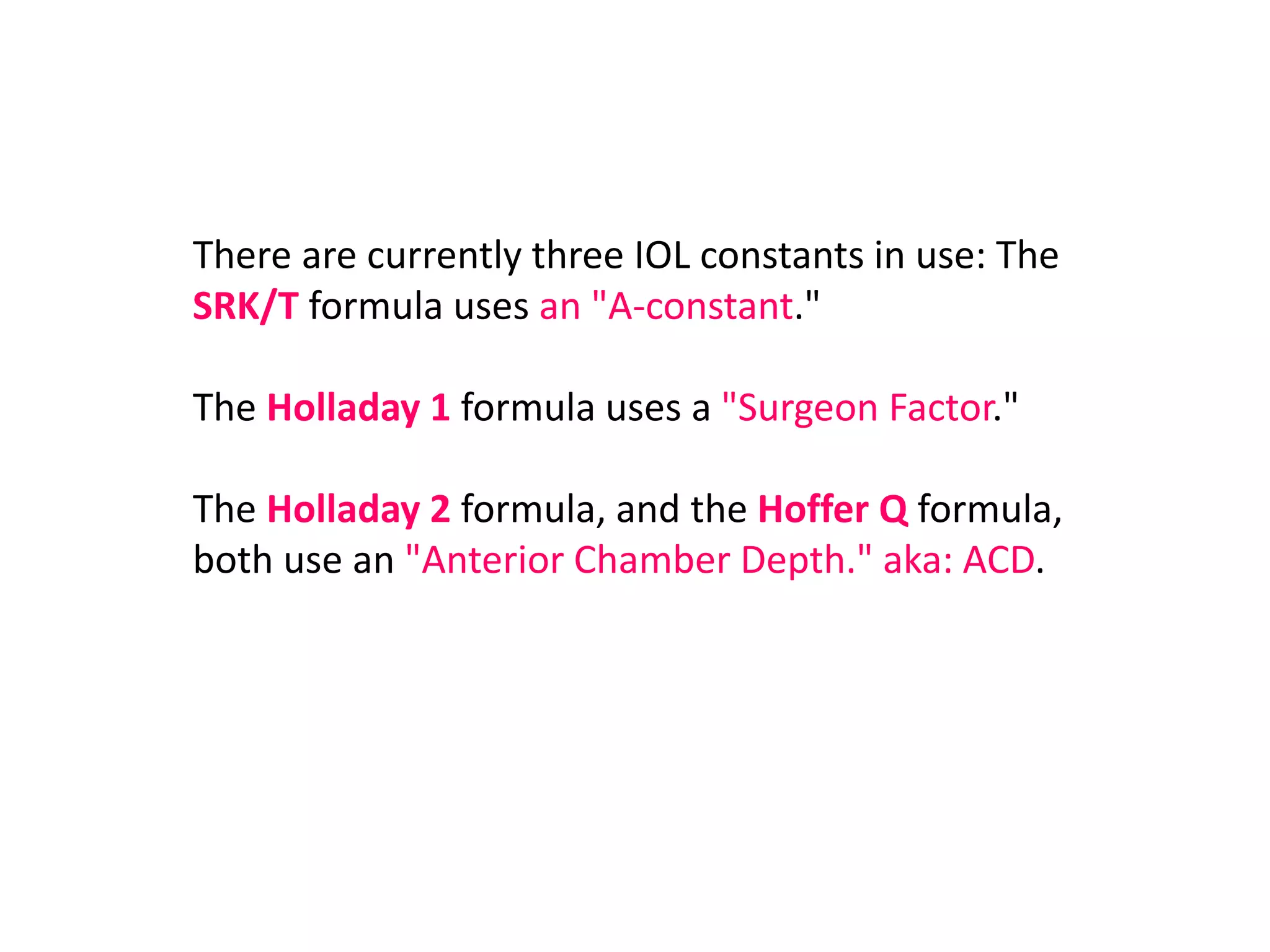
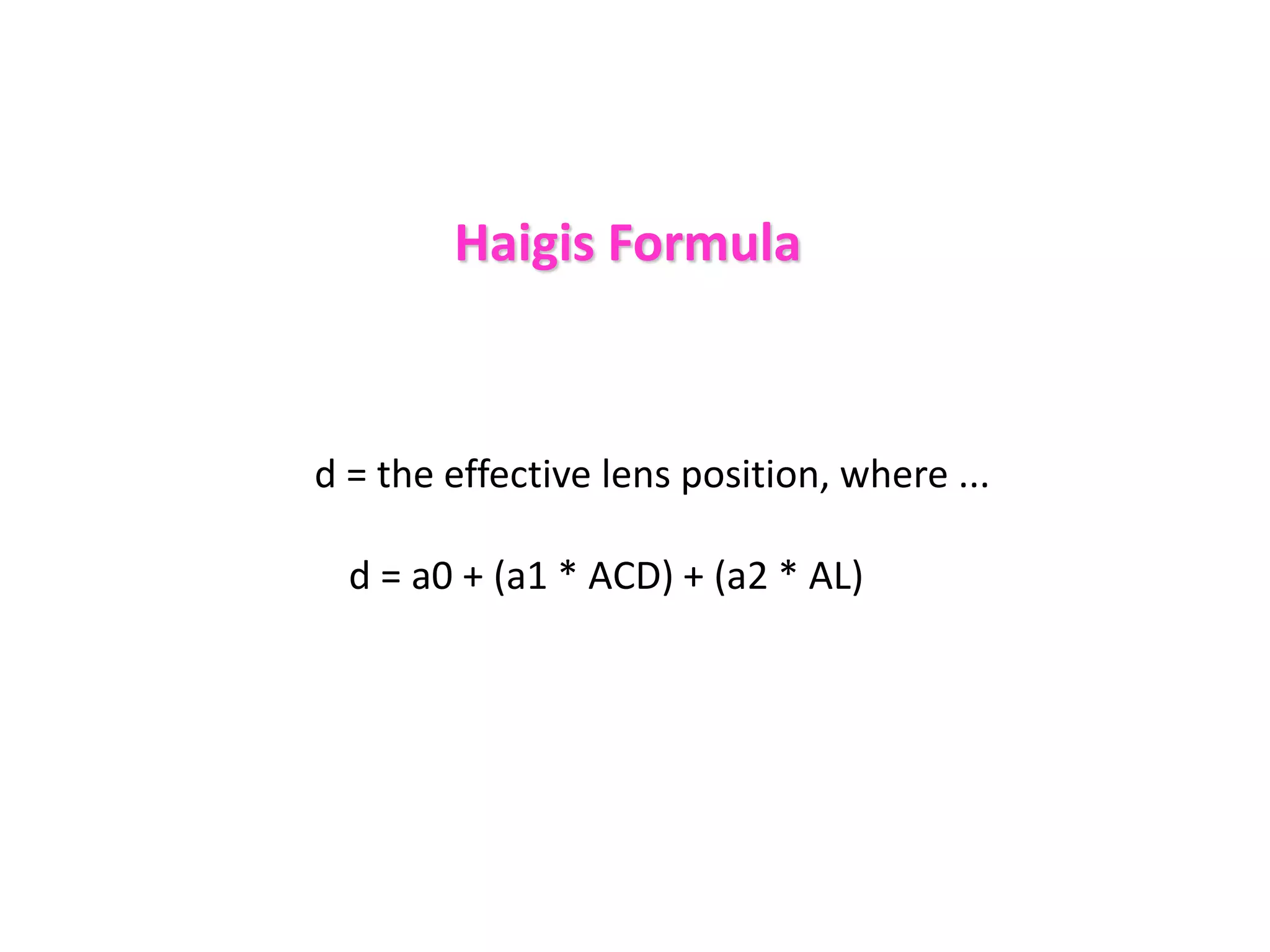
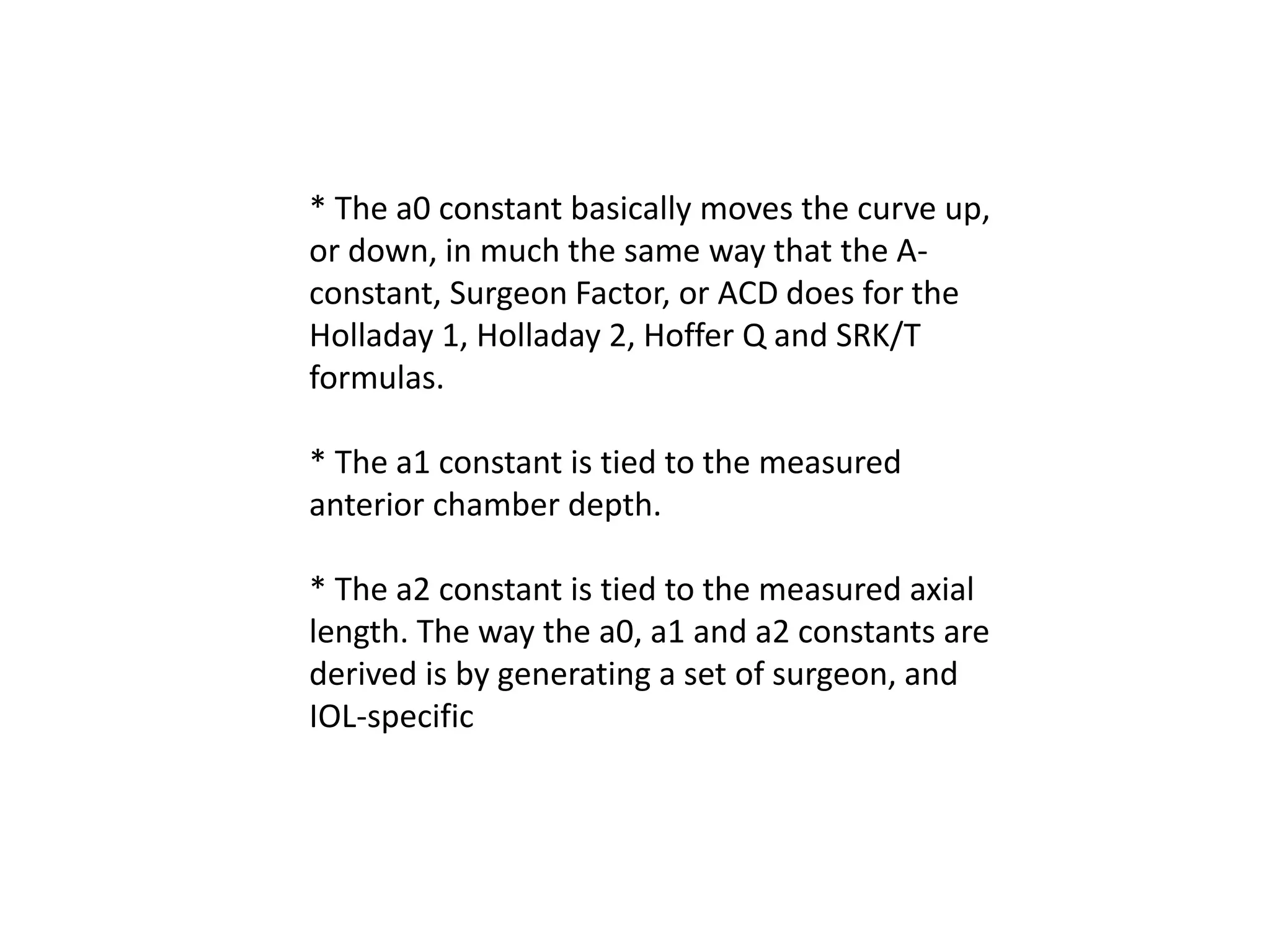
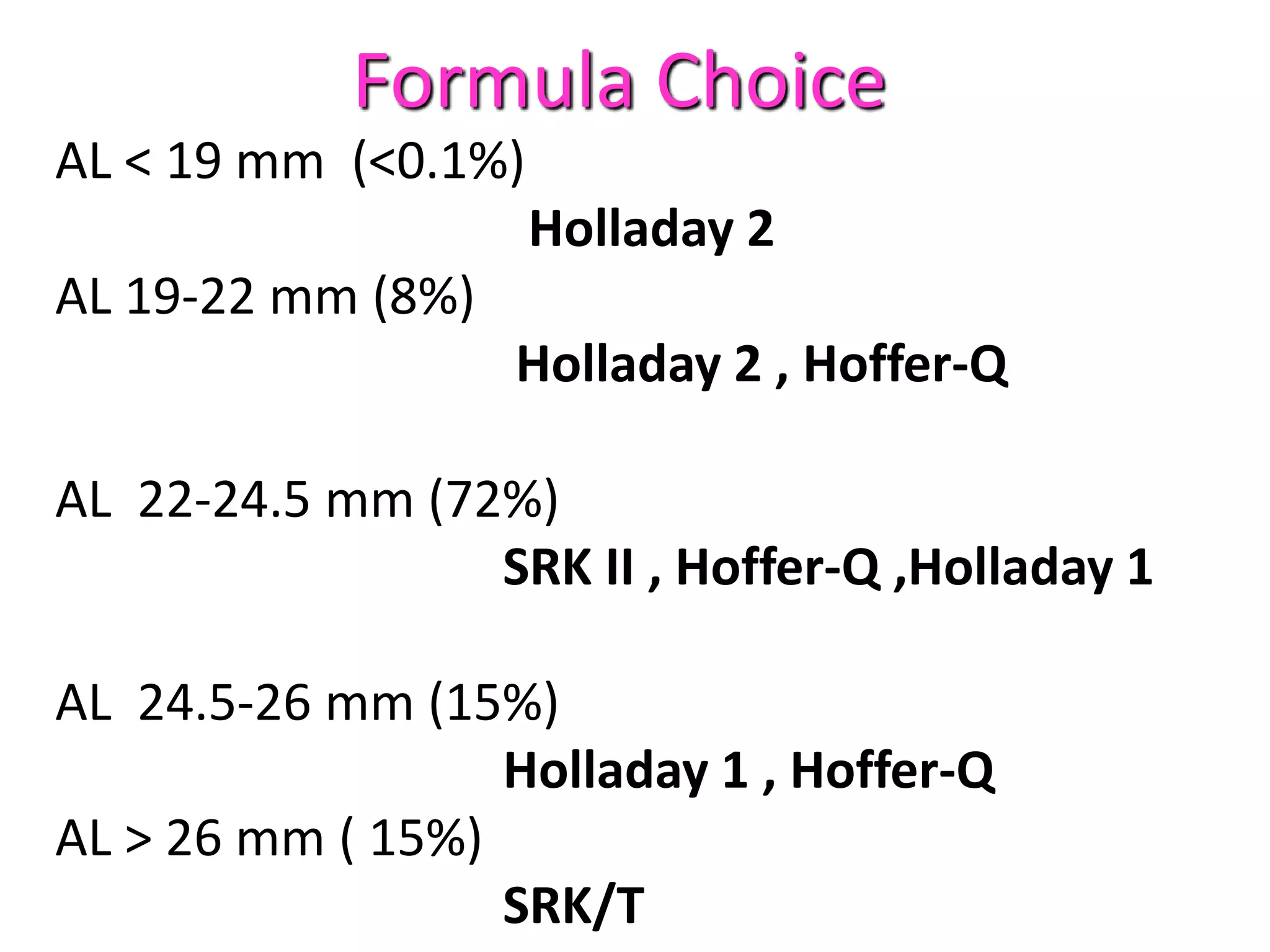
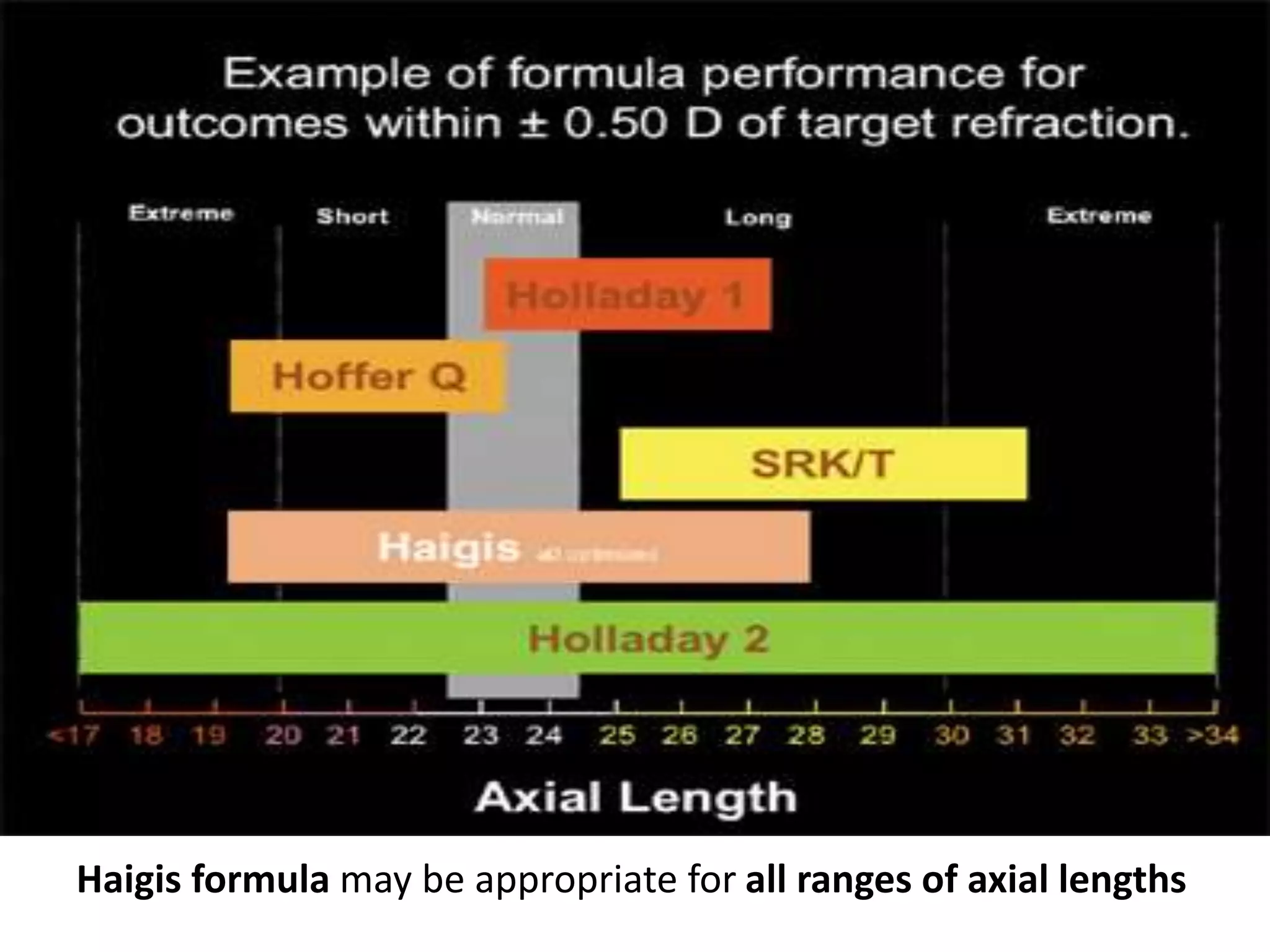
The document outlines the objectives and procedures of a national ocular biometry course, emphasizing the importance of precise biometry in cataract surgery for accurate outcomes. It discusses various biometry techniques including a-scan ultrasonography and optical biometry, highlighting their advantages, potential errors, and detailed measurement protocols. Additionally, it reviews intraocular lens power calculation methods and the evolution of different IOL formulas to optimize surgical results.