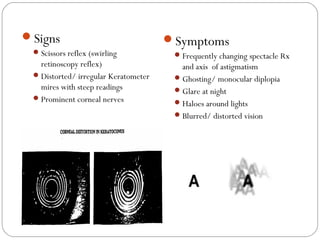
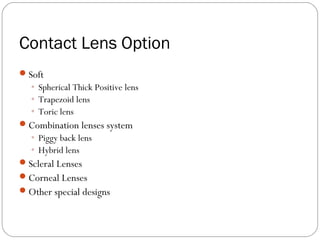
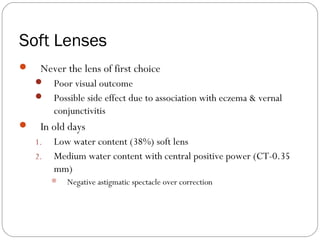
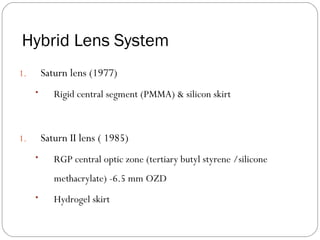
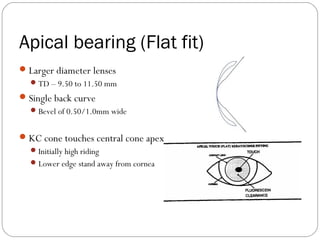
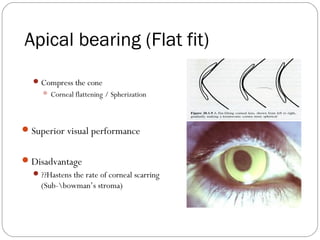
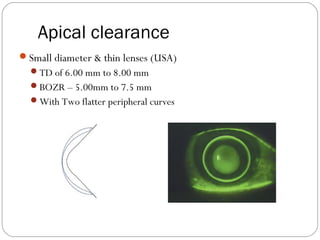
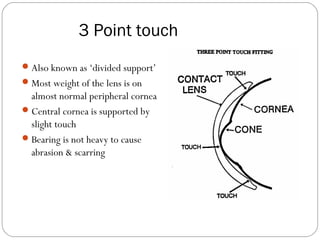
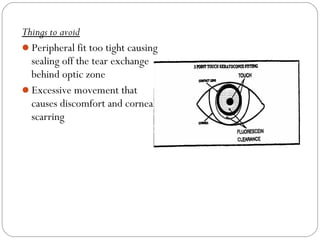
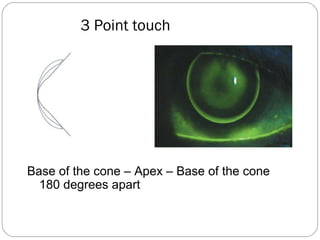
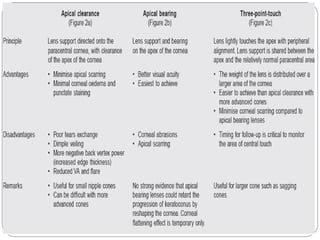
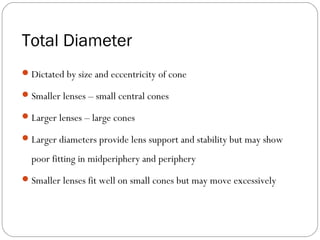
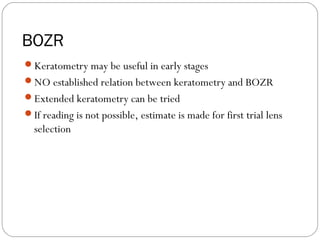
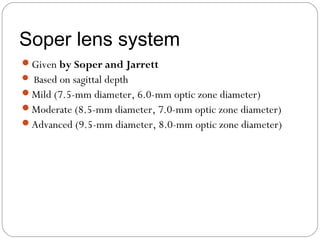
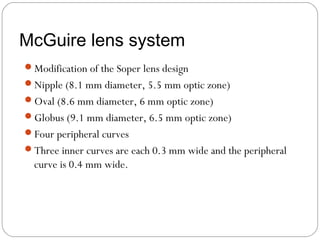
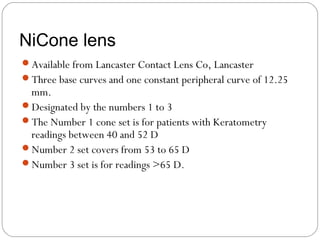
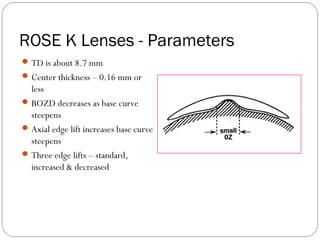
This document provides information on contact lens options for managing keratoconus. It discusses various soft lens designs, scleral lenses, corneal lenses, and hybrid lens systems. For corneal lenses, it describes two fitting philosophies - apical bearing and apical clearance. Specific lens designs are also outlined, including Soper, McGuire, NiCone, and ROSE K lenses, which are designed to closely fit the irregular shape of the cornea in keratoconus. The document provides details on parameters like total diameter, base curve radius, optic zone diameter, and materials for fitting these specialized lenses.