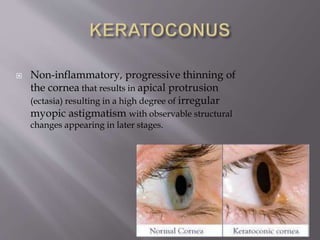
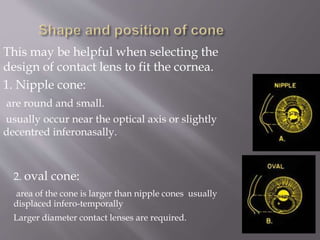
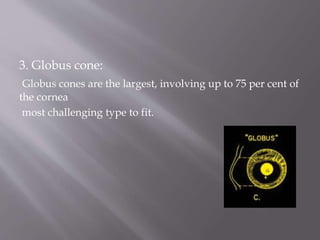
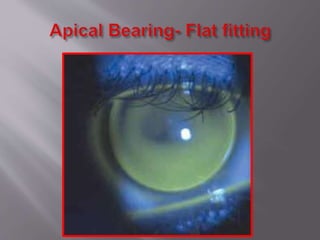
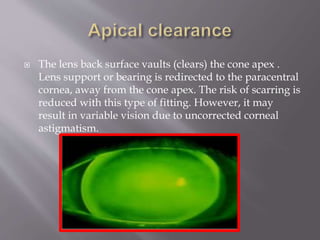
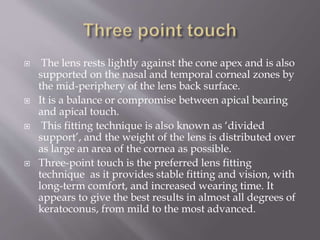
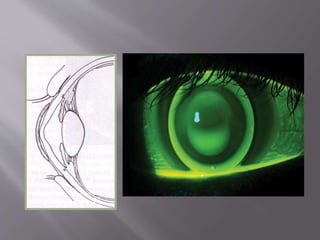
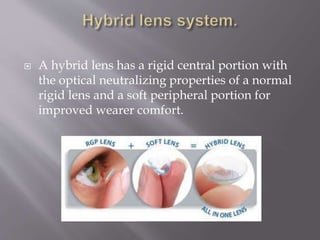
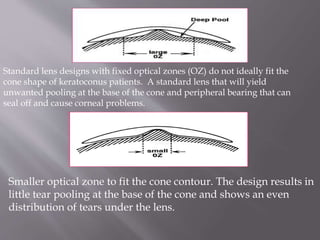
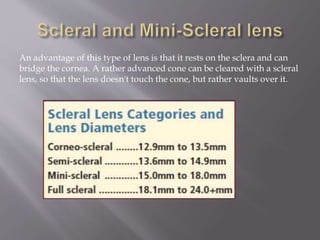
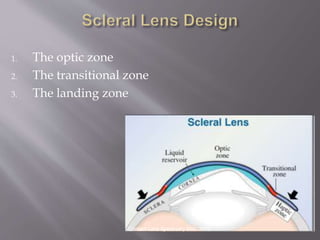
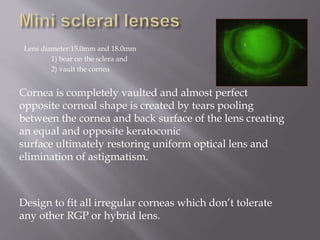
This document discusses keratoconus and contact lens fitting options for keratoconus patients. It begins by describing the different types and stages of keratoconus cones. It then discusses the various contact lens options including soft lenses, rigid gas permeable lenses, and scleral lenses. For rigid gas permeable lenses, it explains the different fitting philosophies of apical bearing, apical clearance, and three point touch. Specific lens designs like Rose K2 and scleral lenses are also summarized. Key factors for determining the appropriate contact lens are also listed.