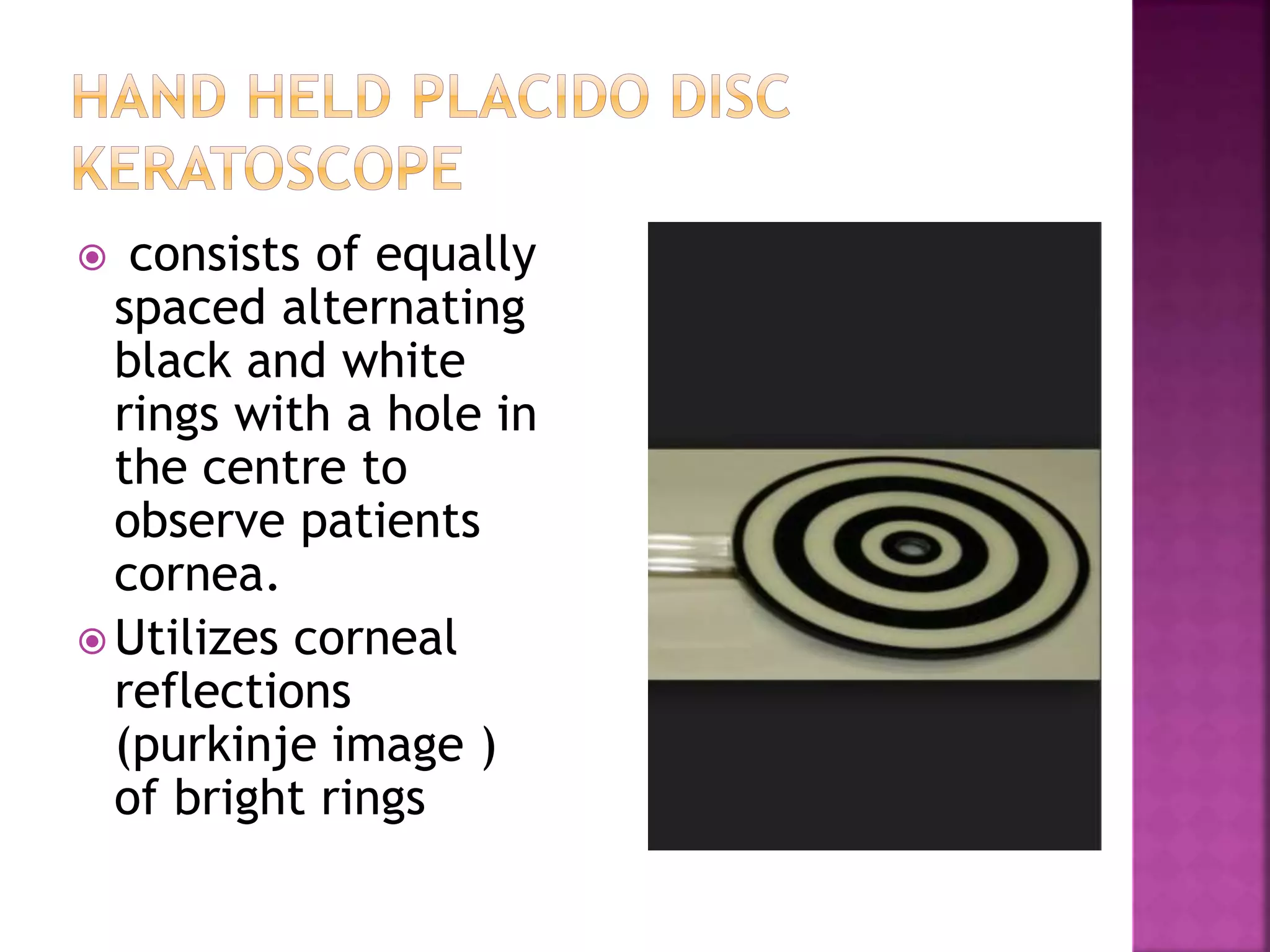
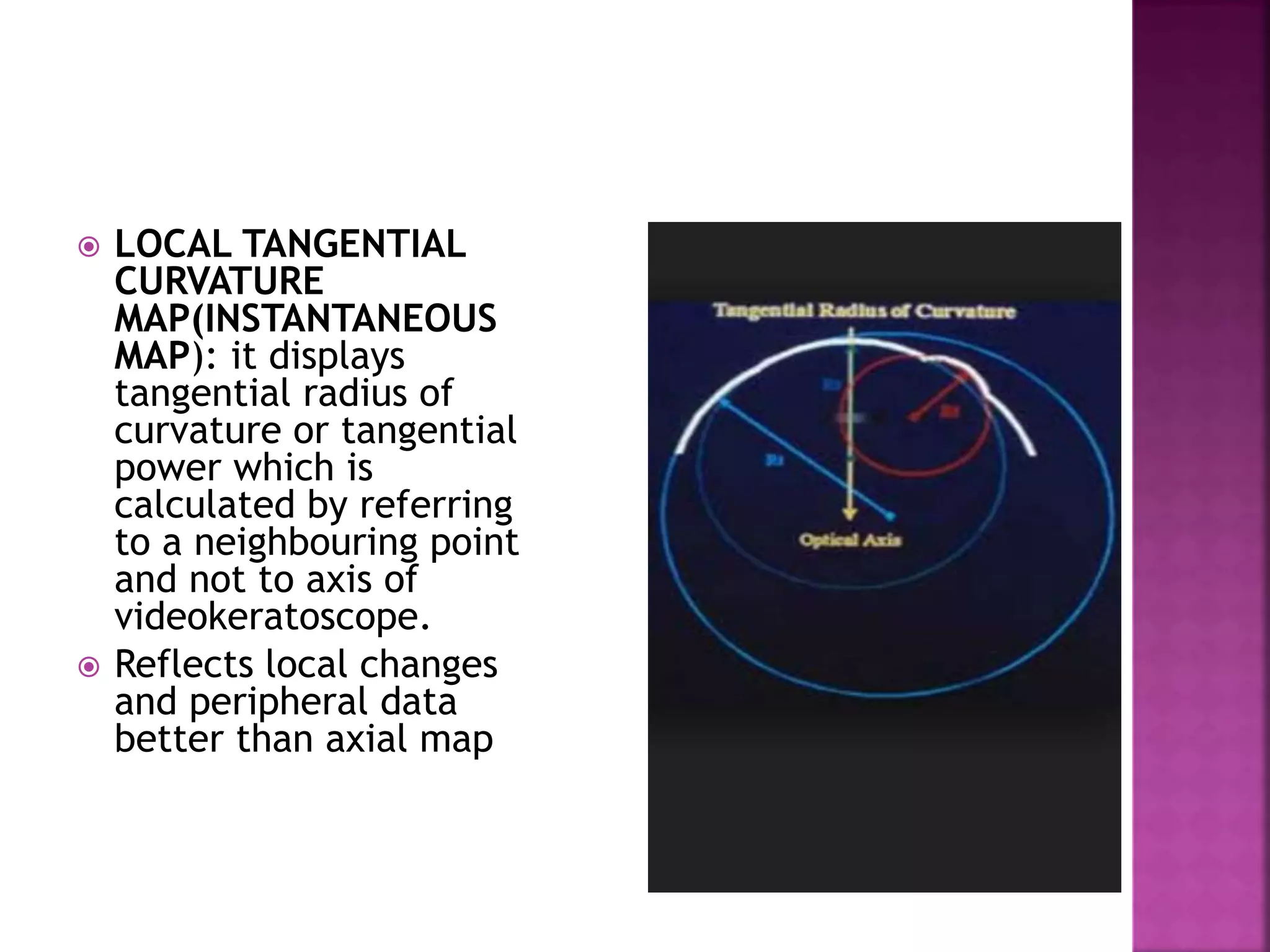
The cornea is the main refractive element of the eye, contributing 70% of the eye's refractive power. Even minor changes to its shape can significantly alter the image formed on the retina. The cornea has an elliptical anterior surface and a circular posterior surface. It varies in thickness from center to periphery. Corneal topography is used to map the shape of the cornea using various techniques such as Placido disk, elevation-based, and Scheimpflug imaging. Topography provides quantitative data on corneal curvature, thickness, and irregularities that aid in diagnosing conditions like keratoconus.