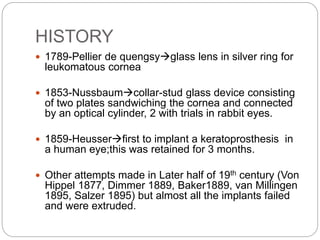
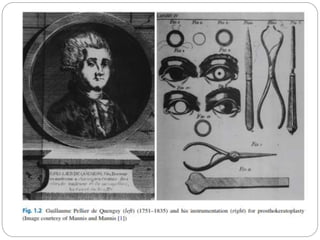
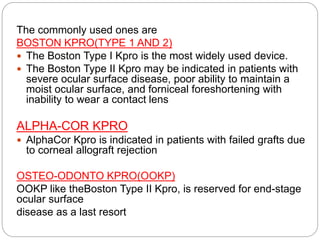
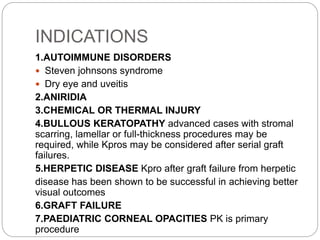
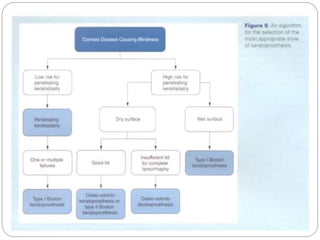
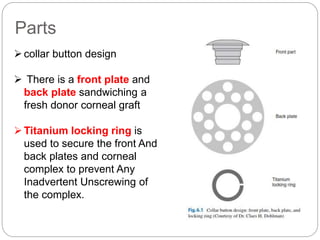
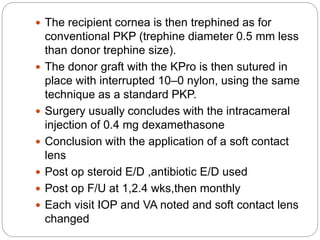
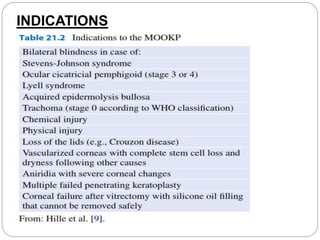
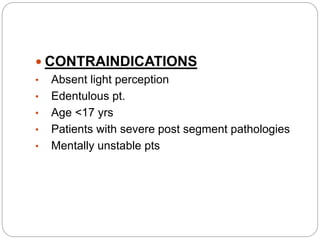
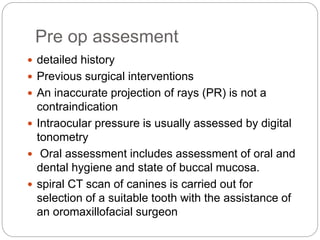
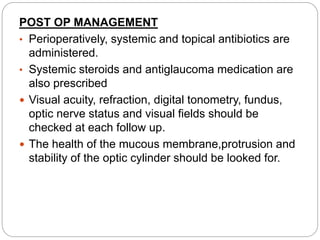
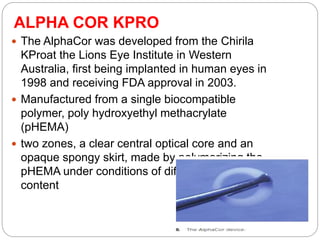
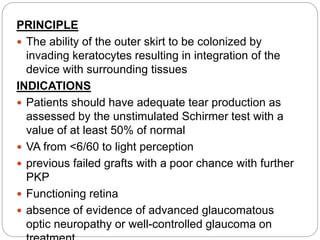
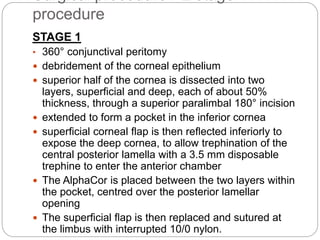
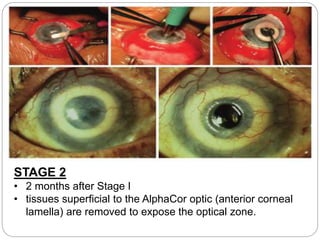
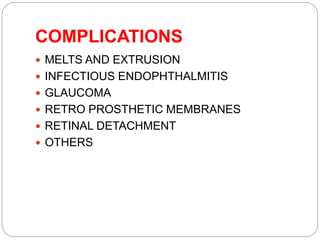
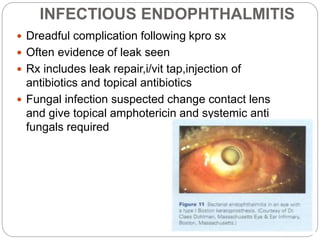
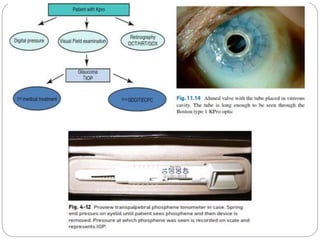
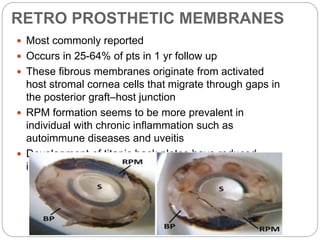
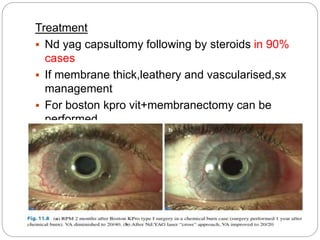
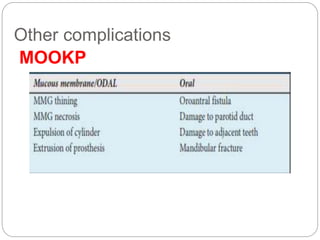
Keratoprosthesis is a surgical procedure that replaces a severely damaged or diseased cornea with an artificial cornea to restore vision. The first attempts at keratoprosthesis in humans date back to the mid-19th century, but most implants failed. Modern keratoprosthesis designs like the Boston KPro and AlphaCor KPro sandwich a donor corneal graft between plastic plates. Complications can include melting/extrusion of the implant, infection, glaucoma, retinal detachment, and formation of membranes behind the implant. Close post-operative monitoring is required to manage complications and maintain vision with keratoprosthesis implants.