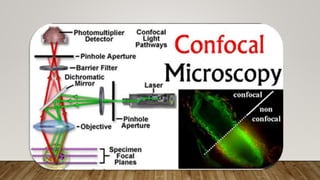
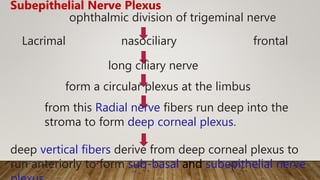
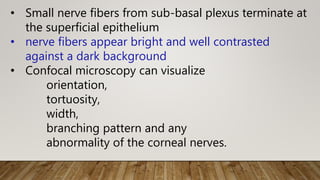
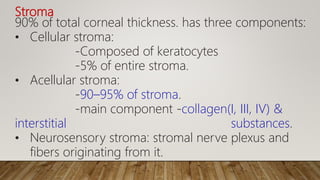
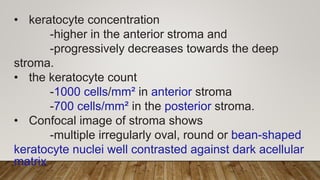
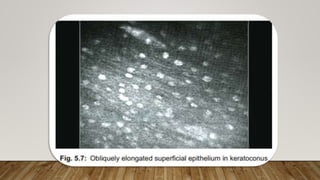
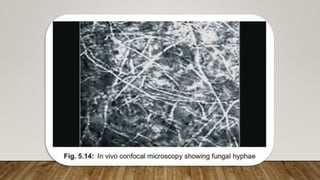
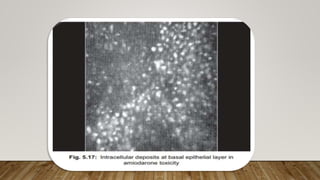
Confocal microscopy allows high-resolution imaging of the cornea. It works by only focusing on a single point and eliminating out-of-focus light to view corneal structures with 1-2 μm lateral and 5-10 μm axial resolution. This allows visualization of the epithelium, subepithelial nerves, stroma, and endothelium. Confocal microscopy is useful for evaluating corneal diseases like keratoconus and dystrophies by identifying morphological changes to these layers.