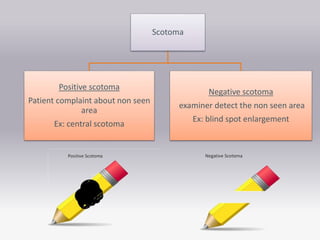
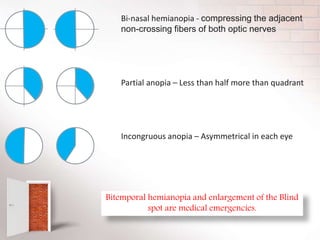
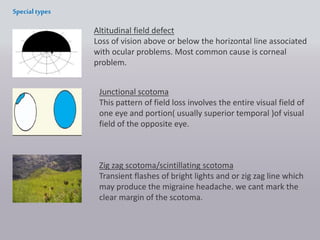
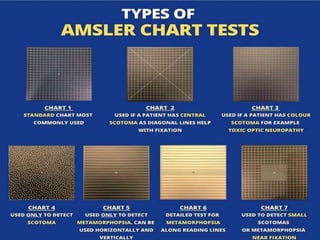
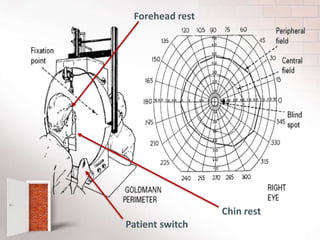
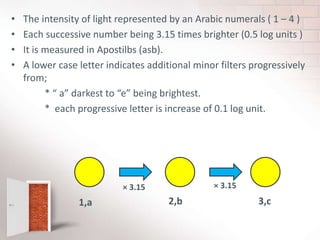
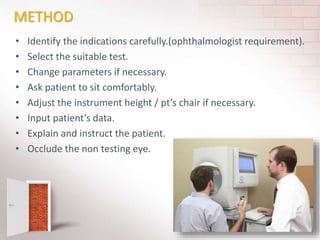
The document covers the concept of visual fields in ophthalmic technology, focusing on definitions, evaluation techniques, and disorders associated with the visual pathway. It details various visual field testing methods, such as confrontation tests, Amsler grid tests, and automated perimetry, effectively used to diagnose conditions like glaucoma and scotomas. Additionally, it discusses classical visual field defects and the anatomical and physiological aspects of the visual pathway, providing insight into how visual information is processed by the brain.