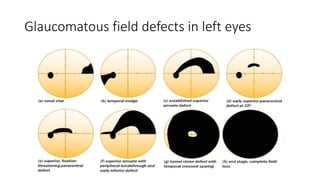
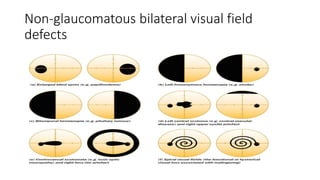
Visual field tests are used to detect peripheral vision changes in glaucoma patients. There are several types of visual field tests, but they generally involve the patient looking straight ahead and pressing a button when they see flashes of light in their peripheral vision. The tests are repeated over time to monitor for progression of vision loss. Common visual field defects seen in glaucoma include nasal steps, arcuate defects, and constriction of peripheral vision. Careful visual field testing is important for glaucoma diagnosis and management.