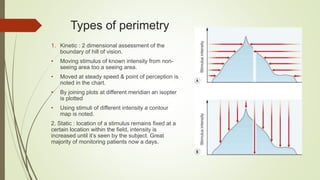
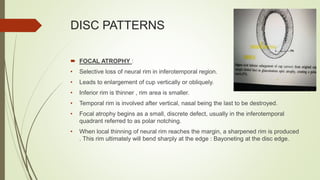
This document discusses visual field assessment and changes related to glaucoma in the optic nerve and retina. It defines key terms like visual field, isopters, and scotomas. It describes different types of visual field defects seen in glaucoma like arcuate defects, nasal steps, and generalized depression. It also discusses optic nerve head anatomy and the effects of increased intraocular pressure on the lamina cribrosa and retinal ganglion cell axons. Different techniques for visual field testing like kinetic, static, and threshold perimetry are summarized along with reliability indices.