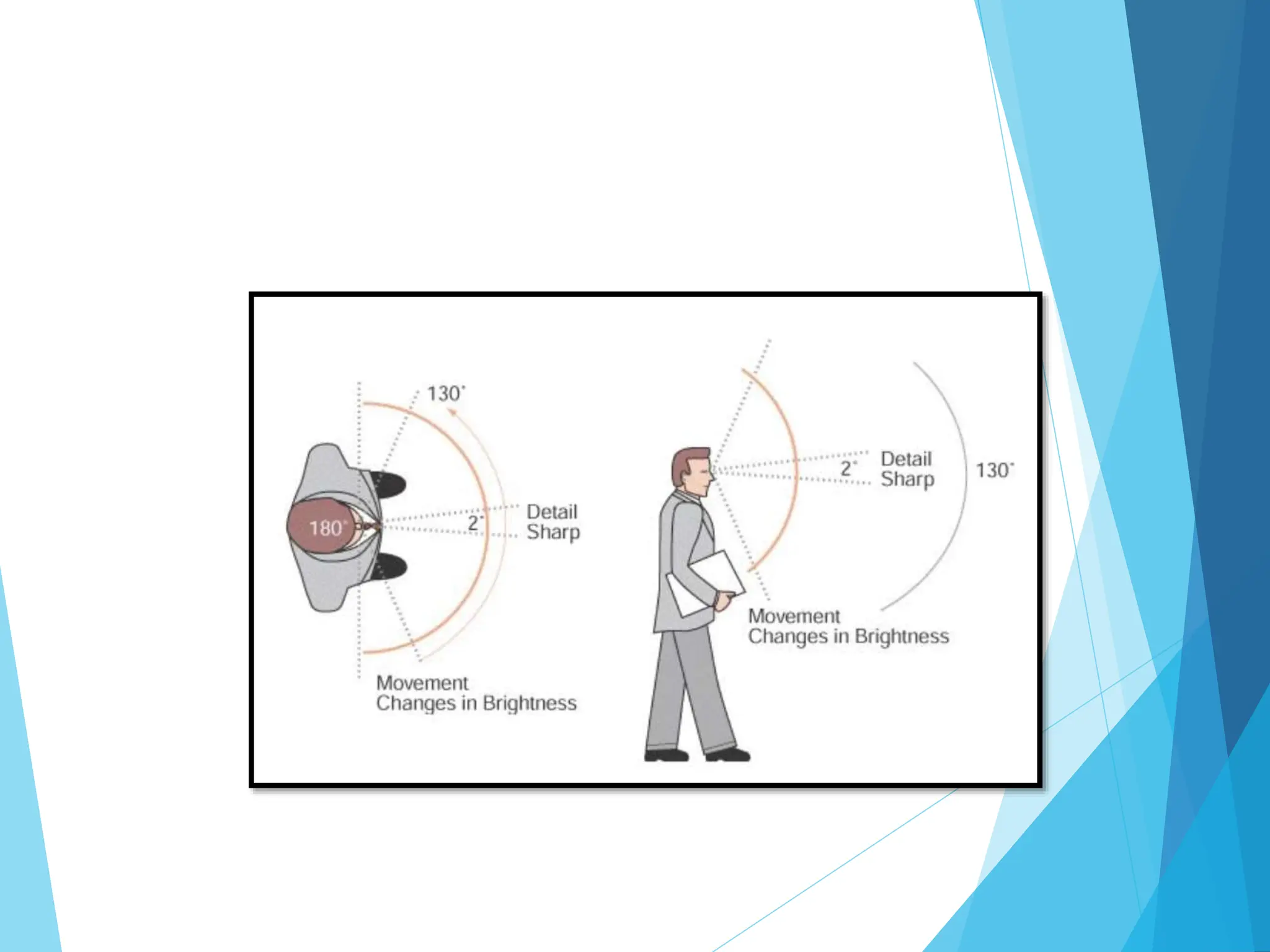
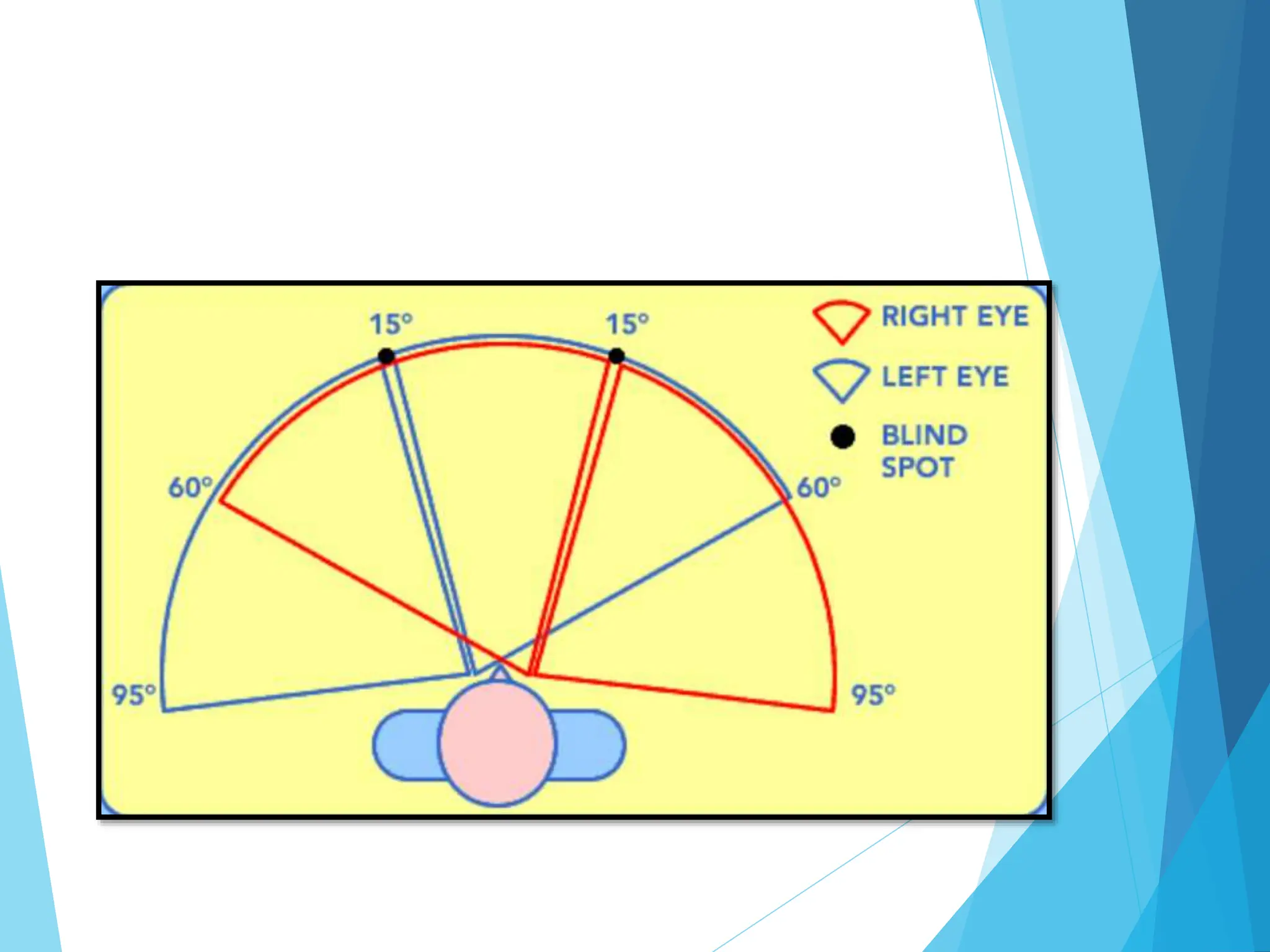
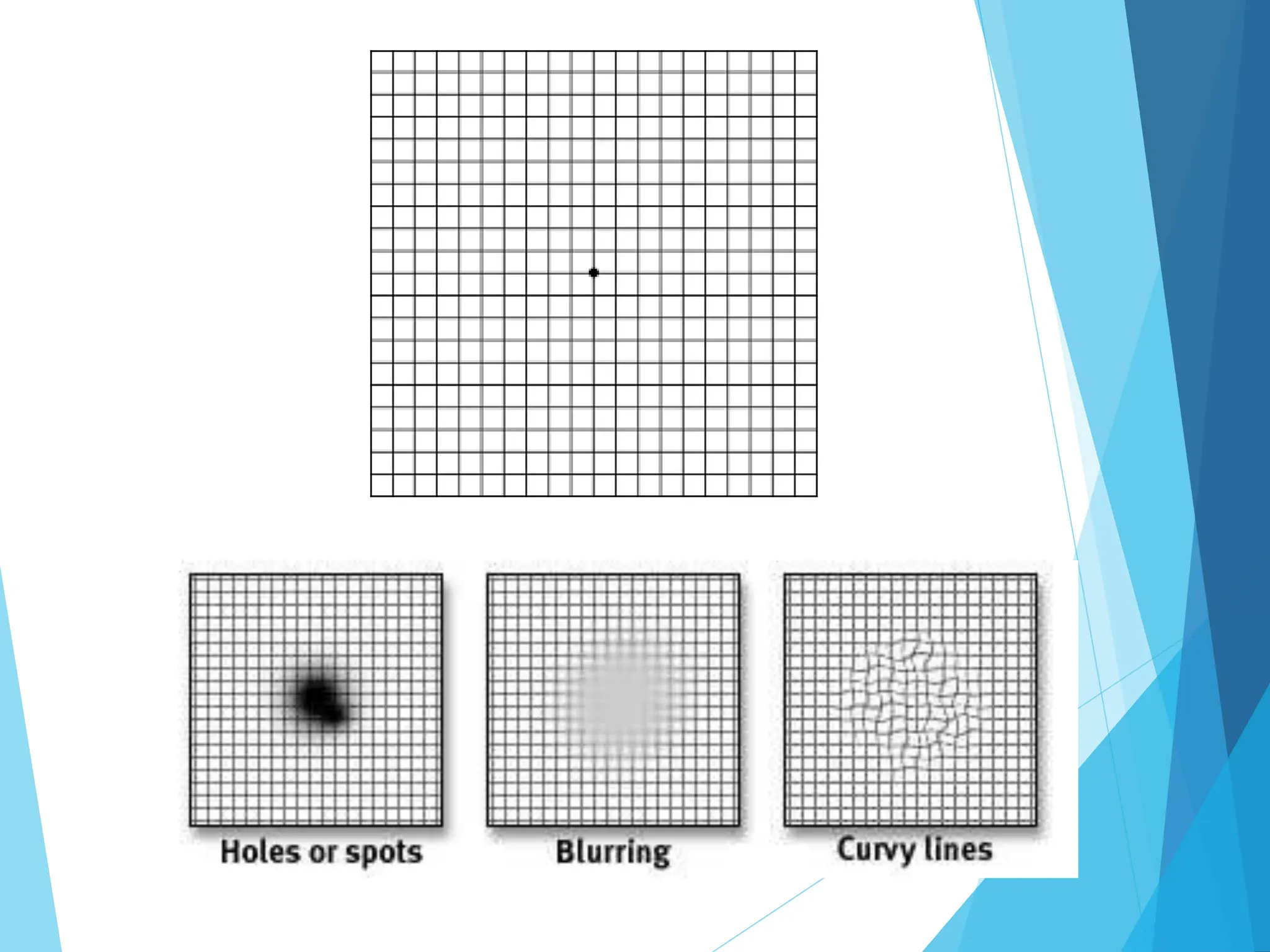
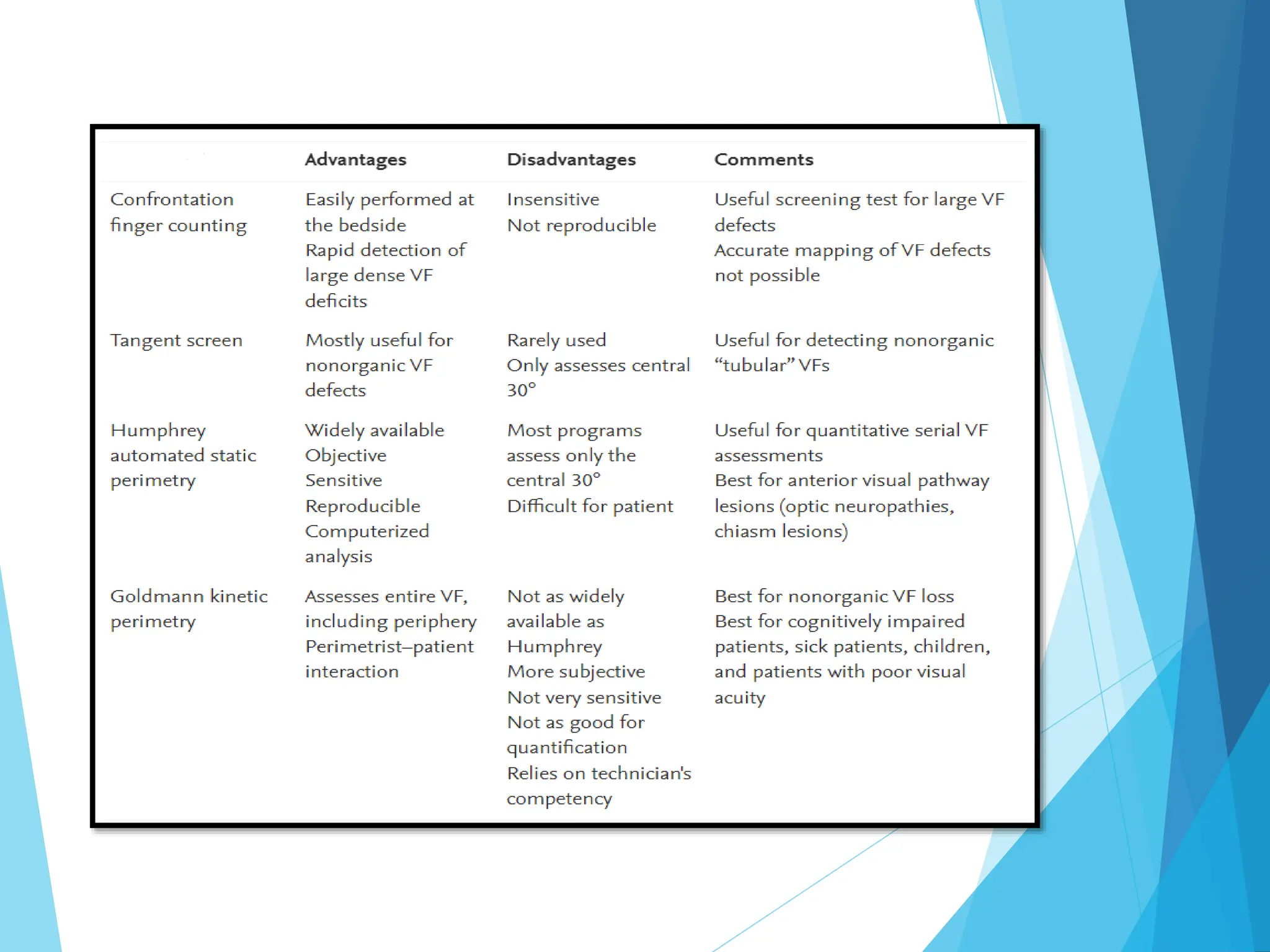
This document discusses visual field testing methods. It defines the visual field as the area that can be seen simultaneously without moving the eyes. Common testing methods are described, including confrontation testing, Amsler grid, tangent screen, kinetic perimetry, and static perimetry. Traquair's representation of the visual field as a hill is introduced. Physiological features like the blind spot are explained. Automated static perimetry is now the standard due to its ability to systematically and objectively measure sensitivity across the visual field. Factors affecting perimetry results are also reviewed.