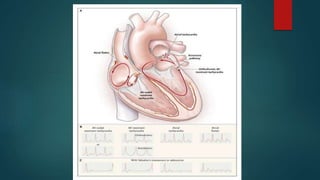
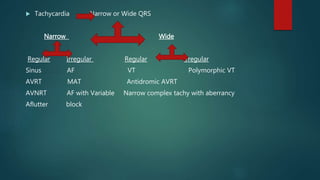
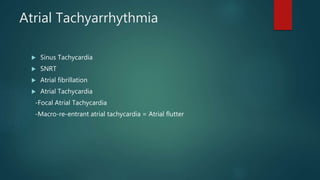
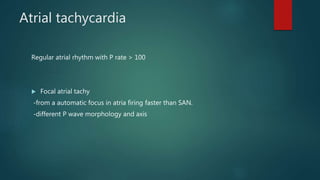
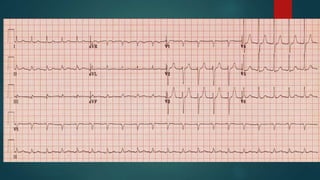
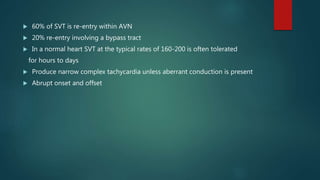
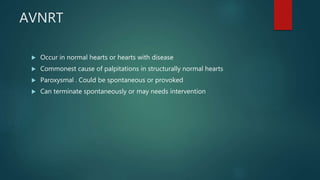
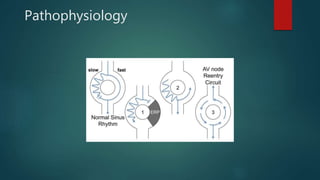
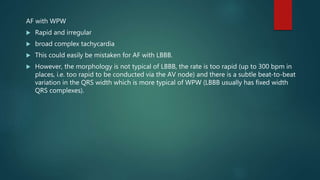
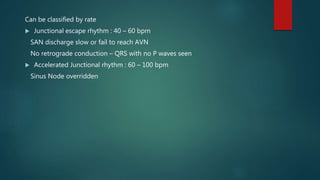
This document discusses various types of tachyarrhythmias categorized by their anatomical location and electrophysiological mechanisms. It describes atrial arrhythmias including sinus tachycardia, atrial fibrillation, atrial flutter, and atrial tachycardia. It also discusses atrioventricular node reentrant tachycardia, atrioventricular reentrant tachycardia, junctional tachycardia, and ventricular arrhythmias including monomorphic ventricular tachycardia, polymorphic ventricular tachycardia, and ventricular fibrillation. Key features and mechanisms of each type are outlined to aid in diagnosis and classification.

![Sinus Tachycardia
Physiological[exercise/emotion] or pathological
-look for underlying cause
-If no underlying cause found consider SNRT or focal Atrial tachycardia
-Sinus tachycardia in a normal heart with no underlying cause is called
inappropriate sinus tachycardia](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-8-320.jpg)

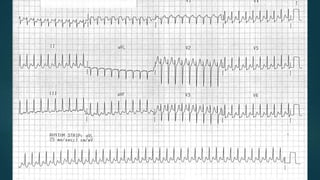
![Atrial Flutter
Caused by re-entry circuit over a large area of a atrium[R/L]
Atrial rate >240[usually 300]. AV block 2:1 usually or more occasionally
1:1 if sympathetic stimulation or Accessary pathway[unstable/VF]
Ventricular rate usually 125-175
Narrow complex tachycardia
Flutter waves best seen in leads II, III, aVF
Flutter waves in V1 may resemble P waves
Irregular with variable AV block
Loss of isoelectric baseline](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-11-320.jpg)

![ Sinus tachycardia
P waves hidden within T [camel hump appearance]](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-17-320.jpg)

![Atrioventricular tachyarrhythmia
Depends on activation between atria and ventricles or AVN
AVNRT
AVRT
Junctional tachycardia
[commonly called SVT]](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-20-320.jpg)
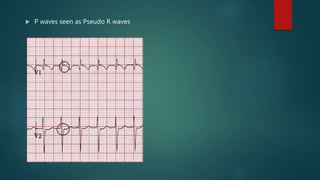
![ECG
Regular tachycardia [140-280]
Narrow QRS [<120] –unless known BBB, accessory pathway or rate related aberrant
conduction
P waves
-Not visible usually
-if visible inverted in 11,111,aVF or as pseudo s waves
-May be seen as a Pseudo R wave after QRS V1-2
ST depression with or without CAD-rate related](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-24-320.jpg)

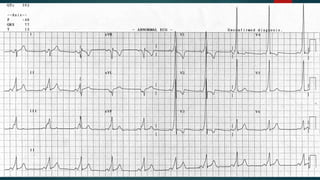
![ECG-WPW
In SR
Short PR < 120
Delta wave [positive /negative]
QRS – wide > 110
ST and T discordant changers](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-28-320.jpg)




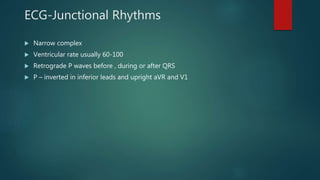
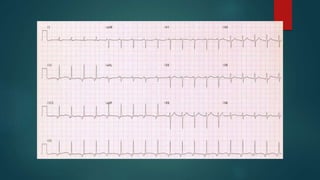
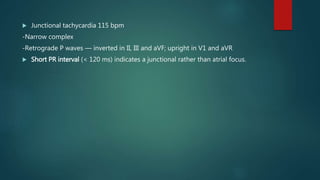
![Junctional Tachycardia
Arise from AVN or bundle of His
Junctional pace maker rate > SAN
Impulses spread retrograde to Atria and antegrade to Ventricles
Atria may activate before, during or after ventricles
If no retrograde conduction and faster Junctional pace maker rate [than
SAN ]can cause AV dissociation
Uncommon in healthy hearts
Seen with CHF, IHD and Digoxin Toxicity](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-42-320.jpg)
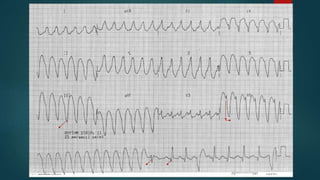
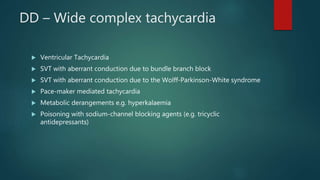
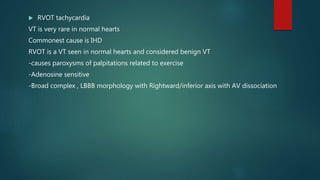
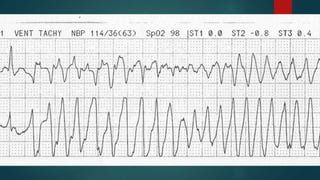
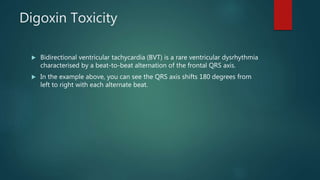
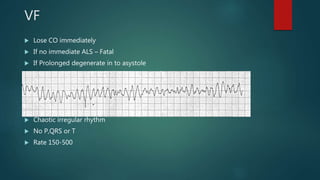
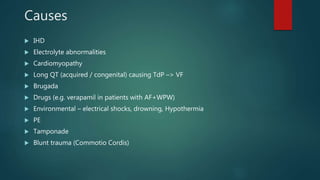
![Ventricular Tachyarrhythmia
Contained completely in the ventricle
VT
-Monomorphic VT
-Polymorphic VT [Eg-torsades de pointes]
VF](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-47-320.jpg)
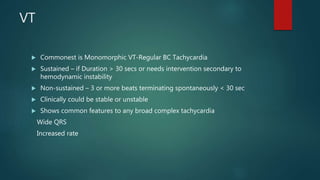
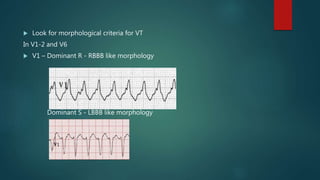
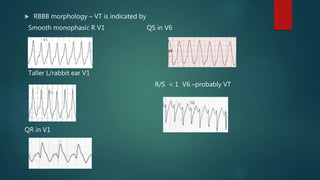
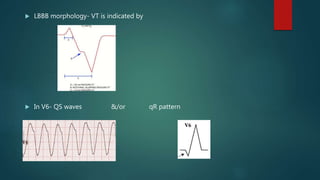
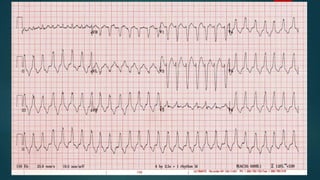
![Features suggestive of VT
Very broad >160ms
No typical RBBB or LBBB pattern
Extreme axis deviation
Capture beats and fusion beats
Positive or negative concordance with no RS complexes
Brugada sign
Taller Left rabbit ear[V1]
Josephson’s sign
AV dissociation](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-49-320.jpg)


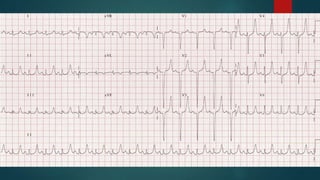
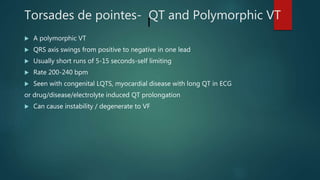
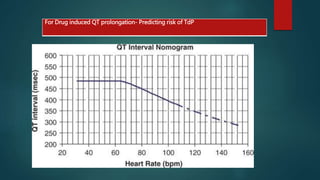
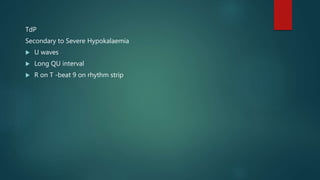
![ Long QT precipitates Early after depolarizations – Tall U waves / PVC
If a PVC occurs on a preceding T [ R on T ] TdP can be initiated
Onset is often after a long-short-long R-R interval [Pause dependent]
Bigemini with long QT– High risk of TdP
Rate > 220 – High risk of VF](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-66-320.jpg)

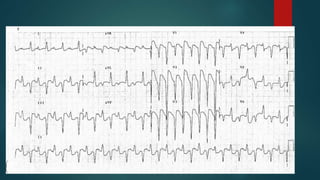

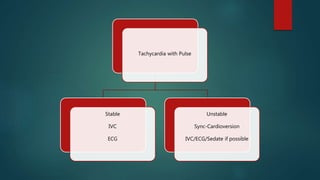

![Stable Wide-Complex
Tachycardia
Regular
VT/Uncertain Rhythm
-Amiodarone
-Prepare for Cardioversion
-If Known SVT with Aberrancy
Give Adenosine
Irregular
-If Pre-excitation with AF[AF+WPW]
NO AVN Agents[ Adenosine/CC/BB]
Consider
Antiarrhythmic[Amiodarone/Procanamide
-TdP- Mg 1-2 g over 5-60 min
-Polymorphic VT
Sync Cardioversion
-AF with Aberrancy
Follow Narrow-complex Irregular Protocol](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-77-320.jpg)
![Adenosine
Do not use –
-broad complex irregular tachycardia[AF+WPW]/ Polymorphic tachycardia
-flutter in WPW
-VT –Precipitous instability
Can be used in RVOT
Can be used in Narrow Complex Tachycardia – WPW/AF/Flutter/SVT](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-79-320.jpg)
![AF
Loan AF is Unlikely to present with instability
Treat underlying causes [ Sepsis/Hypovolemia/IHD]
Adenosine, BB, CCB, Digoxin and Amiodarone –Contraindicated in AF+WPW](https://image.slidesharecdn.com/thachyarrhthmias-160428050620/85/Tachyarrhythmia-Management-80-320.jpg)
