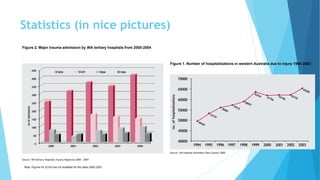
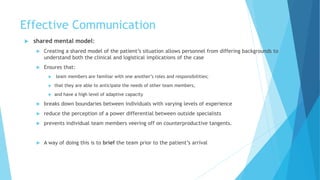
The document discusses trauma teams and their roles. It defines a trauma team as a multidisciplinary group that works together to assess and treat severely injured patients. A team approach has been shown to significantly reduce resuscitation times compared to individual doctors. The roles of trauma team members are outlined, as well as techniques for effective communication, briefing, handover, and speaking up if concerns arise. Statistics from Western Australia in 2015 show the most common causes of death for major trauma patients were head injuries and brain death. Overall mortality rates were lower than the national average.