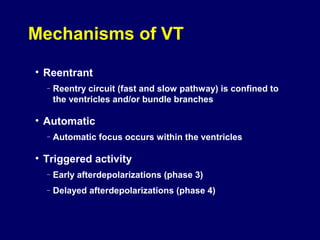
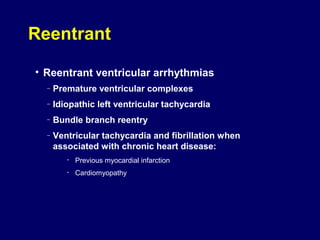
This document provides an outline for a module on ventricular tachyarrhythmias. It begins with module objectives of differentiating types of ventricular tachycardias using ECGs. The outline then describes ventricular tachyarrhythmias, discusses characteristics like mechanisms and sustained vs nonsustained types. It classifies ventricular tachyarrhythmias as monomorphic or polymorphic, and provides subcategories within each with descriptions and ECG recognition details. Specific arrhythmias discussed include idiopathic VT, bundle branch reentry, ventricular flutter, fibrillation, and Torsades de Pointes.