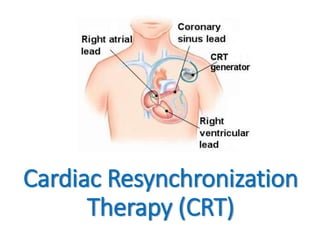
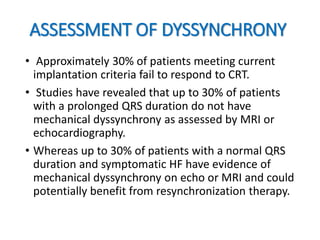
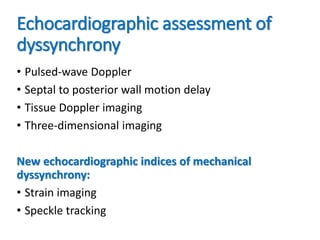
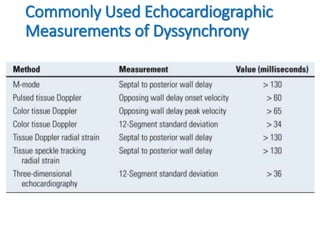
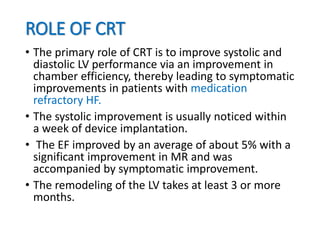
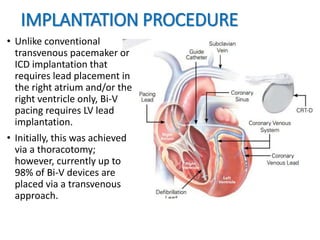
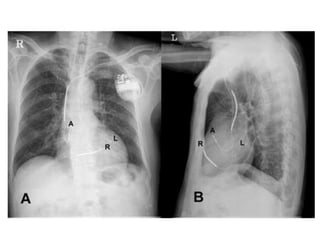
This document provides an overview of cardiac resynchronization therapy (CRT). It discusses how conduction delays can lead to electromechanical dyssynchrony and impair the heart's function. CRT aims to improve this synchrony and thereby improve systolic and diastolic function. The document outlines different types of dyssynchrony and methods to assess it, including echocardiography. Current guidelines recommend CRT for symptomatic heart failure patients with low ejection fraction and wide QRS duration. The implantation procedure involves placing right atrial/ventricular leads and a left ventricular lead via the coronary sinus.