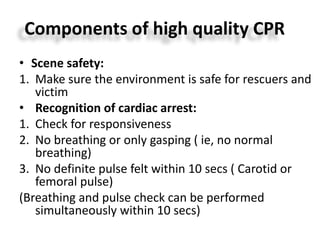
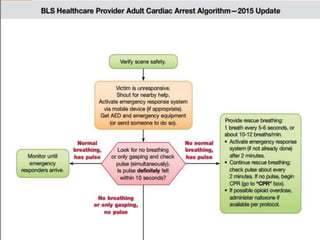
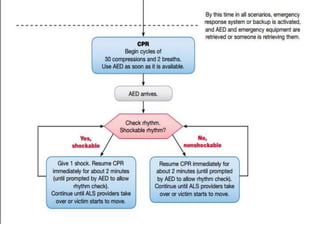
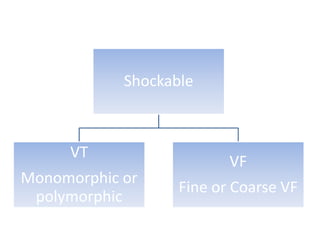
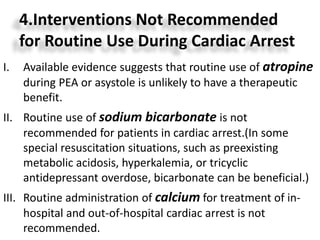
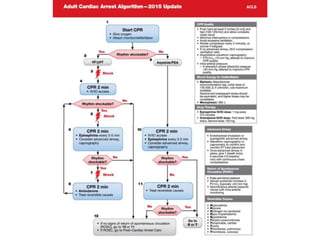
This document summarizes guidelines for adult advanced cardiovascular life support. It outlines the key components of basic life support including immediate recognition of cardiac arrest, activation of emergency response, early CPR, and use of an automated external defibrillator. For advanced life support, it describes the treatment of shockable (ventricular fibrillation, pulseless ventricular tachycardia) and non-shockable (asystole, pulseless electrical activity) cardiac arrest rhythms. It also reviews adjuncts to CPR including oxygen supplementation, capnography, ultrasound, and airway management techniques.
![Adult Advanced Cardiovascular Life Support
Circulation. 2015;132[suppl 2]:S444–S464](https://image.slidesharecdn.com/2015acls-160508080923/85/2015-acls-1-320.jpg)