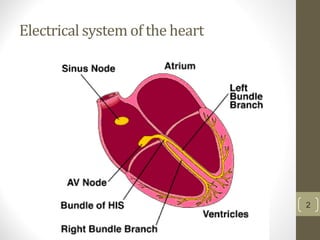
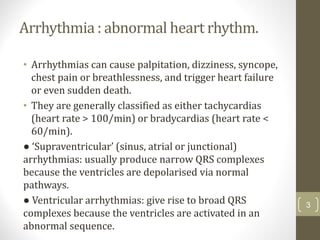
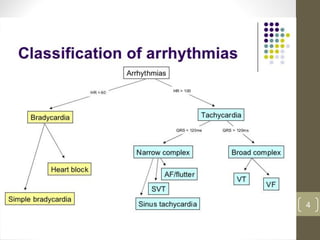
This document discusses arrhythmias and their classification, pathogenesis, clinical presentation, diagnosis and management. It covers topics such as:
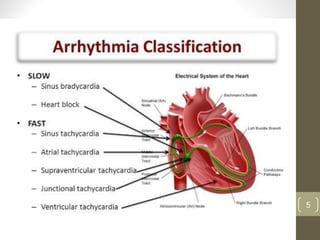
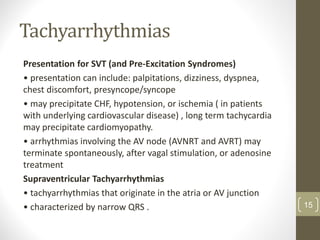
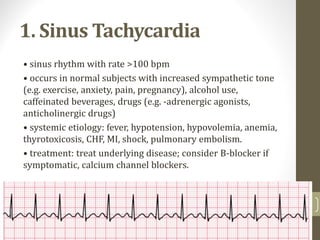
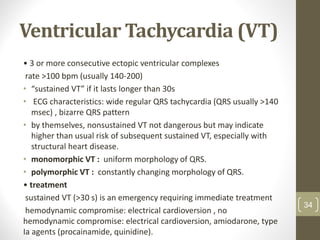
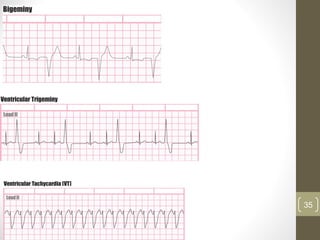
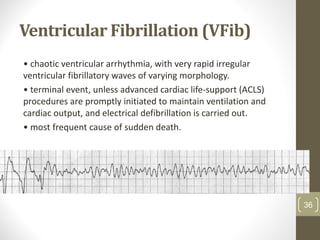
1. Arrhythmias are abnormal heart rhythms that can cause symptoms and health risks if left untreated. They are classified as bradyarrhythmias or tachyarrhythmias.
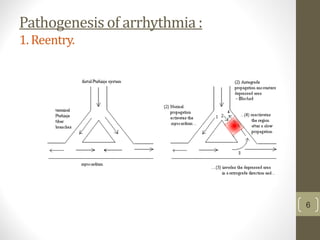
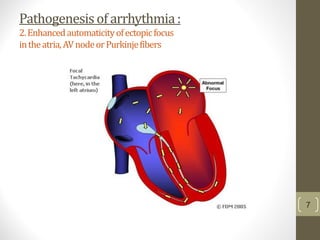
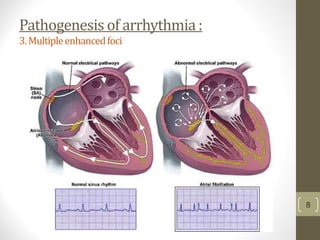
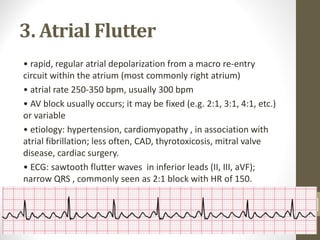
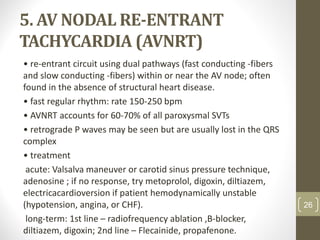
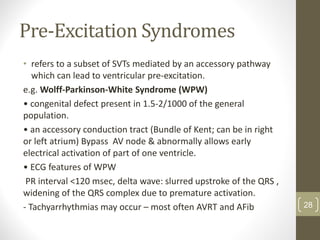
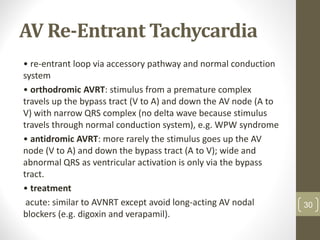
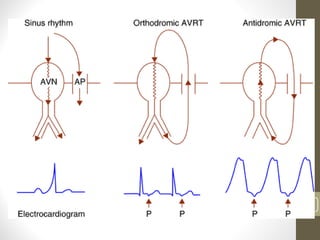
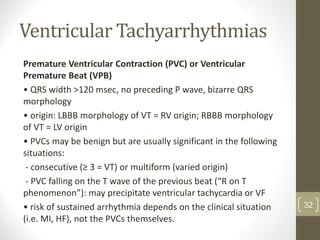
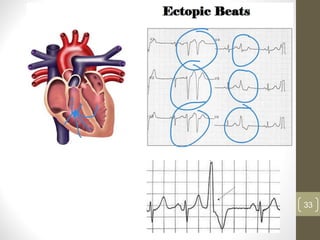
2. Causes of arrhythmias include reentry mechanisms, enhanced automaticity of ectopic foci, and multiple enhanced foci.
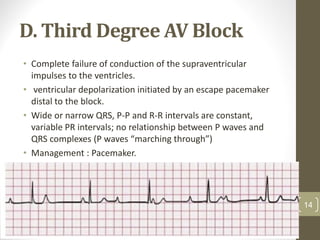
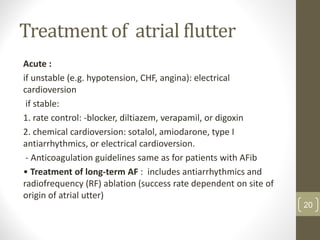
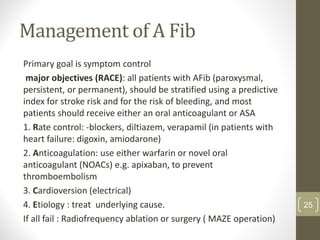
3. Management depends on the specific arrhythmia but may involve rate control with medications, cardioversion, ablation procedures, or pacemaker implantation.