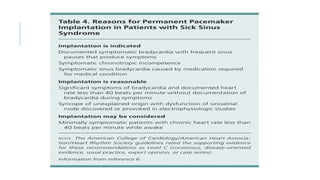
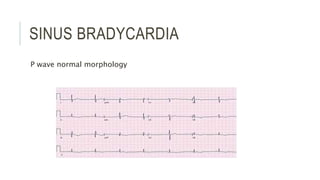
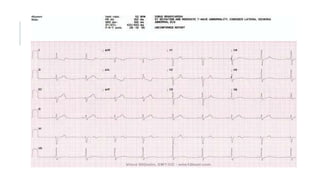
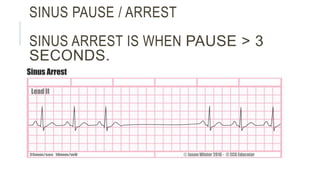
This document discusses sinus node dysfunction (SND), which refers to dysfunction of the sinoatrial node that can cause various electrocardiogram abnormalities like sinus bradycardia, sinus pauses, and inadequate heart rate response to activity. Common causes of SND include sinus node fibrosis, medications that depress sinus node function, infiltrative diseases, inflammatory diseases, and sinus node artery disease. The document recommends permanent pacing for patients with SND who experience symptomatic bradycardia or pauses, as well as those with chronotropic incompetence. It describes various ECG patterns that can occur in SND such as sinus bradycardia, sinus pause/arrest, sinus node exit block, and chronotropic incompetence.
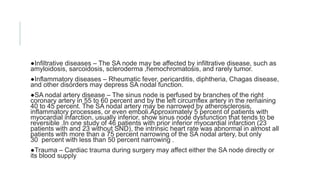
![CAUSES
Sinus node fibrosis — The most common cause of sinus node dysfunction is the replacement of sinus node
tissue by fibrous tissue, Medications and toxins — A number of medications and toxins can depress sinus node
function
●Beta blockers
●Non-dihydropyridine calcium channel blockers
●Digoxin
●Antiarrhythmic medications
●Acetylcholinesterase inhibitors such as donepezil (Aricept) and rivastigmine used in the treatment of Alzheimer's
disease
Other medications associated with depression of sinus node function include parasympathomimetic agents,
sympatholytic drugs (eg, methyldopa, clonidine), cimetidine, lithium, and ivabradine [35,36]. In addition,
poisoning by grayanotoxin, produced by some plants (eg, Rhododendron sp.) and found in certain varieties of
honey, has been associated with depressed sinus node function [37].
Childhood and familial disease — SND is rare in children, but when present it is most often seen in those with
congenital and acquired heart disease, particularly after corrective cardiac surgery [38-41]. Familial sinus node
dysfunction is rare, with mutations in the cardiac sodium channel gene SCN5A and the HCN4 gene (](https://image.slidesharecdn.com/sinusnodedysfunction-210129110500/85/Sinus-node-dysfunction-3-320.jpg)