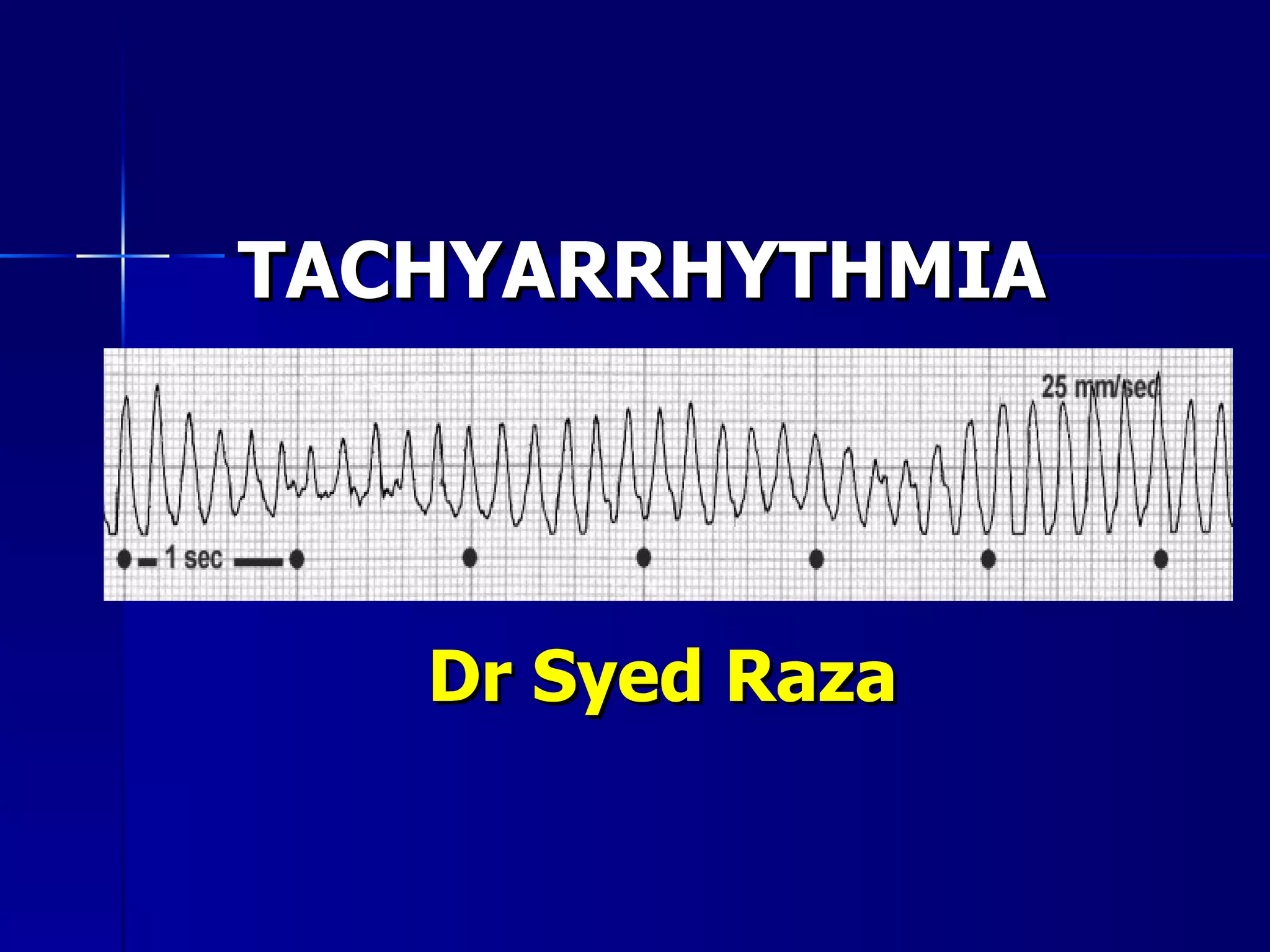
This document provides an overview of evaluating and treating different types of tachycardia, including:
1) It discusses evaluating the patient's hemodynamic stability, history, and ECG to determine the characteristics and cause of the tachycardia.
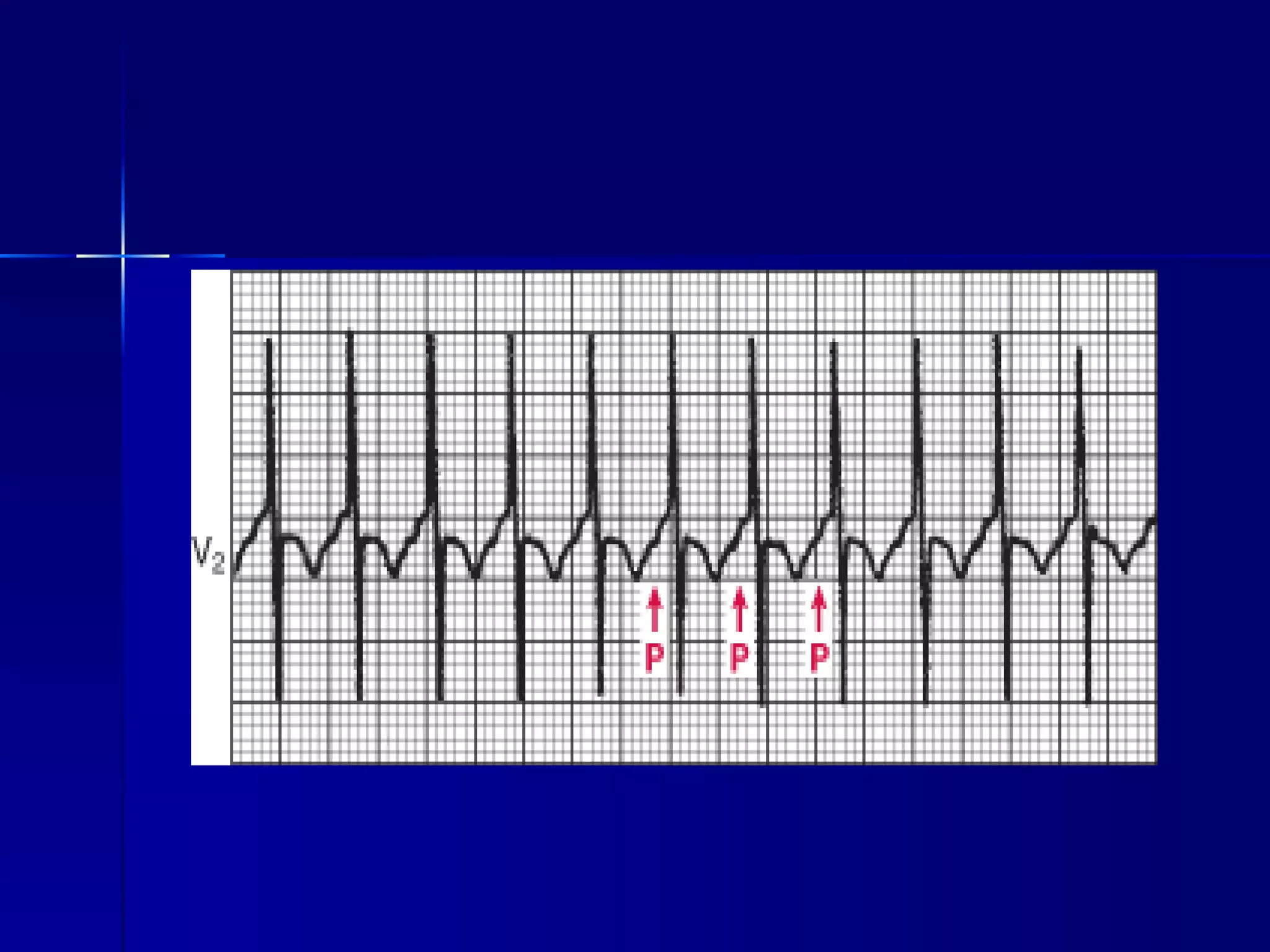
2) It describes differentiating between narrow and wide complex tachycardias, and the differential diagnoses for each, including sinus tachycardia, atrial fibrillation, AV nodal reentrant tachycardia, and ventricular tachycardia.
3) It provides guidance on therapies for different tachycardias, such as electrical or chemical cardioversion, rate control, and ablation. The importance of correctly diagnosing wide complex tachycard





















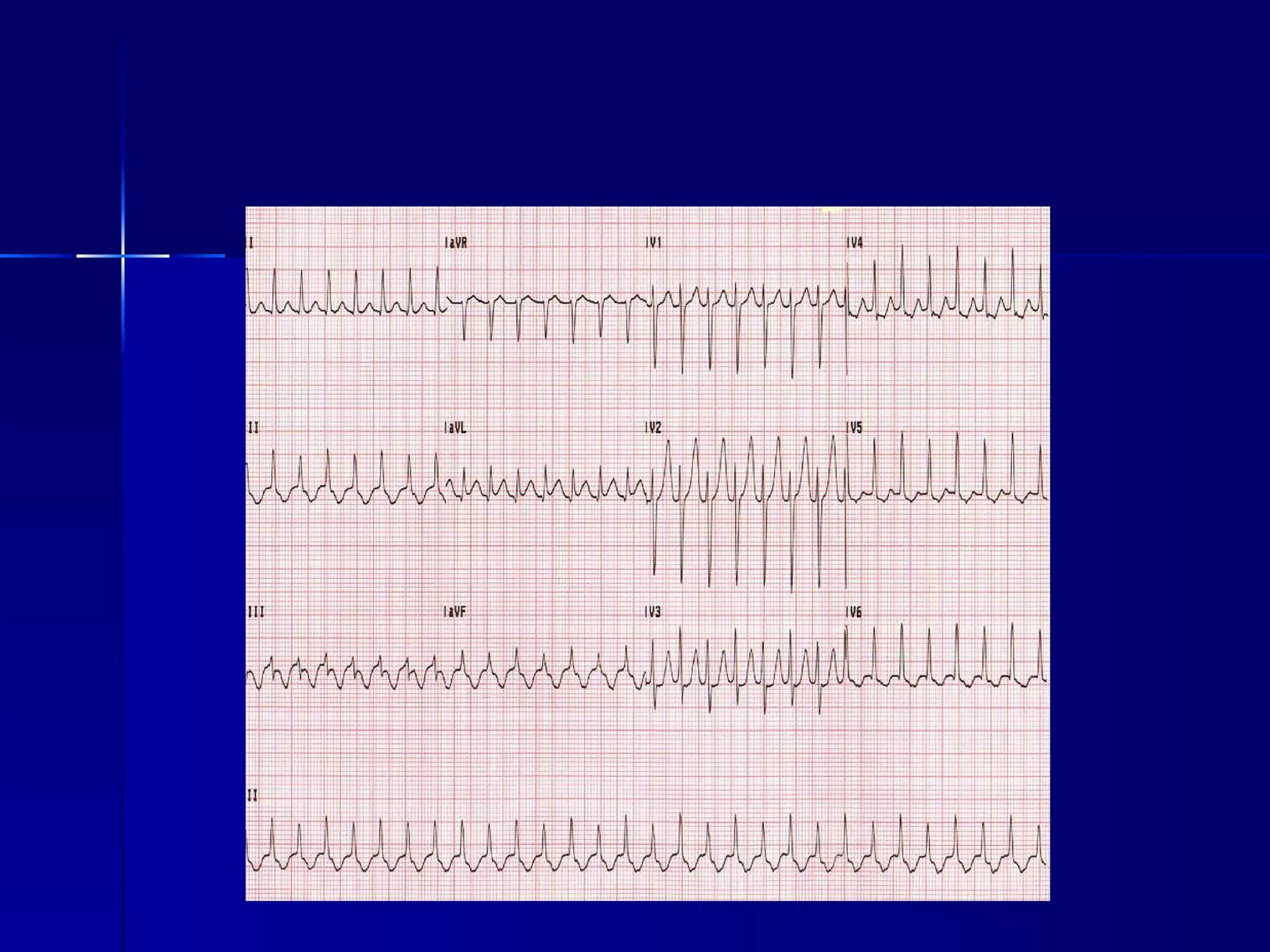



















![SVT vs VT Clinical history Medication Drug-induced tachycardia -> Torsade de pointes Diuretics Digoxin-induced arrhythmia -> [digoxin] ≥2ng/l or normal if hypokalemia Age - ≥ 35 ys -> VT (positive predictive value of 85%) Underlying heart disease Previous MI -> 98% VT Pacemakers or ICD Increased risk of ventricular tachyarrhythmia](https://image.slidesharecdn.com/tachyarrhythmia-110920115400-phpapp02/75/Tachyarrhythmia-44-2048.jpg)















